Introduction
The innervation of the larynx is intricate, detailed, and represents some of the more complex relationships in the anatomy of the head and neck. The vagus nerve is the large nerve that supplies the many branches of nerves that innervate the larynx. The superior laryngeal nerve, its external and internal branches, and the recurrent laryngeal nerve all have very distinct roles in motor and sensory innervation of the larynx. Superiorly, sensory and motor innervation are separated by internal and external branches of the superior laryngeal nerves. Inferiorly, the sensory and motor innervation is provided by the recurrent laryngeal nerve.
Structure and Function
The innervation of the larynx is similar to other areas of the body with both sensory and motor components. There is superior and inferior innervation, and these nerves' names reflect as much. The superior laryngeal nerve is a branch from the vagus nerve arising above the carotid bifurcation as it descends down the neck. The superior laryngeal nerve then divides into external and internal branches.[1] The external branch of the superior laryngeal nerve follows a course with the superior thyroid vessels and contains motor fibers that innervate the cricothyroid muscle.[2][3] While the internal branch of the superior laryngeal nerve pierces through the thyrohyoid membrane and carries sensory fibers that innervate the laryngeal mucosa superior to the vocal cords.[1][2]
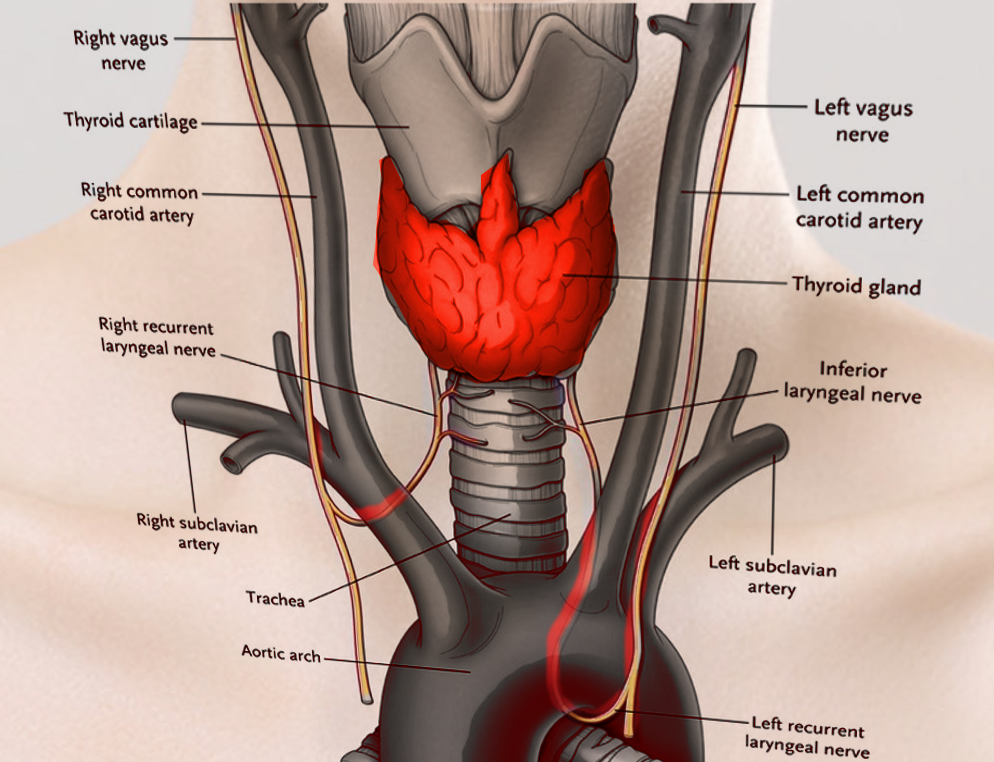
The recurrent laryngeal nerve anatomy differs depending on its laterality—the right recurrent laryngeal nerve branches from the vagus nerve in proximity to the right subclavian artery. The left recurrent laryngeal nerve lies inferior to the aortic arch distal to the ligamentum arteriosus. Both recurrent laryngeal nerves travel superiorly along the lateral surface of the esophagus and trachea, coursing posterior to the thyroid lobes.[2][4] They continue their course superiorly, posterior to the cricothyroid joint, to enter the larynx. Once in the larynx, the recurrent laryngeal nerve is referred to as the inferior laryngeal nerve, innervating all the intrinsic musculature of the larynx except for the cricothyroid muscle. This nerve is the principal motor supply to vocal production. Inferior to the vocal cords, sensory innervation is all provided by the recurrent laryngeal nerves. The inferior laryngeal nerves are the endpoint of the recurrent laryngeal nerves, which have an interesting course. See blood supply and lymphatics for more on this topic.[5]
Embryology
The recurrent laryngeal branch of the vagus nerve originates from the 6th pharyngeal arch along with the intrinsic musculature of the larynx, except for the cricothyroid muscle. The superior laryngeal branch of the vagus nerve originates from the 4th pharyngeal arch along with the cricothyroid muscle. This developmental pattern elucidates why the cricothyroid muscle is the only muscle that receives innervation via the superior laryngeal nerve. The 4th and 6th pharyngeal arches contribute to the formation of the cartilages that are both vital to the structure and function of the larynx: thyroid, cricoid, arytenoid, cuneiform, and corniculate cartilages.
Blood Supply and Lymphatics
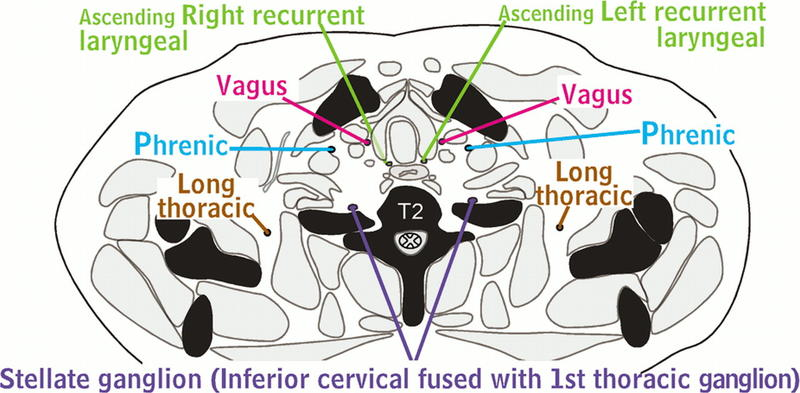
The external branch of the superior laryngeal nerve is immediately deep to the superior thyroid artery and descends on the larynx. The internal branch of the superior laryngeal pierces through the thyrohyoid membrane along with the superior laryngeal artery (a division of the superior thyroid artery). The course of the recurrent laryngeal nerves is interesting due to the lack of symmetry. On the left, the ipsilateral recurrent branches from the vagus nerve and is close to the aorta and wraps around it in an anterior to posterior fashion and ascends in the tracheoesophageal groove on its way to the larynx. On the right, the recurrent laryngeal nerve has a close relation to the right subclavian artery as it wraps around it in an anterior to posterior fashion and, like the left recurrent laryngeal nerve, ascends in the tracheoesophageal groove to the ipsilateral larynx.
Nerves
The vagus nerve is the 10th cranial nerve and is responsible for supplying the entire larynx with its complex innervation through the different nerves and respective branches discussed in this article. See structure and function for more information on this detailed topic.
Muscles
As discussed before, the external branch of the superior laryngeal nerve supplies the cricothyroid muscle. The function of the cricothyroid muscle is to tense the vocal cords, thereby increasing vocal pitch. The external laryngeal nerve also gives branches to the pharyngeal plexus and the superior portion of the inferior pharyngeal constrictor. The recurrent laryngeal nerve innervates the majority of the intrinsic laryngeal musculature, responsible for vocal production. These muscles include the major abductor of the vocal cords, the posterior cricoarytenoid muscle. Adductors innervated by the recurrent laryngeal nerve include the lateral cricoarytenoid muscles, arytenoid muscles (transverse and oblique), and the aryepiglottic muscle; these muscles contribute to the physiologic "cough." The lateral cricothyroid, thyroarytenoid (vocalis), and transverse and oblique arytenoid muscles. All these muscles are involved in vocal production. Other important muscles include the thyroarytenoid muscle in charge of relaxing the vocal folds and also approximate them, the vocalis muscle, which lies lateral to the vocal ligament and is in charge of shortening the vocal cords and finally the thyroepiglottic muscle which depresses the epiglottis and widens the laryngeal inlet.[5]
Physiologic Variants
The laryngeal nerves have various anatomical variants. One crucial known variant is the lack of the recurrent laryngeal nerve being "recurrent" around the subclavian or aorta and instead arising from the vagal truck in the neck and traversing with the inferior thyroid artery to the larynx. It is imperative to be aware of this variation, especially when performing surgical interventions in the neck, particularly thyroid or parathyroid procedures.[4]
Surgical Considerations
As mentioned, during thyroid and parathyroid procedures, surgical injury to these nerves is a feared complication. Intraoperative superior and recurrent nerve monitoring during head and neck procedures is common and is used frequently with thyroid and parathyroid procedures. Monitoring is primarily by the placement of a neural integrity monitoring (NIM) endotracheal tube. The nerve monitor is part of the endotracheal tube and is testable before the procedure begins to ensure proper placement.
Clinical Significance
The laryngeal nerves may suffer damage during surgical procedures, especially with thyroid and parathyroid surgeries. Injury to the recurrent laryngeal nerve during dissection produces vocal cord paralysis and results in reduced protection of the airway due to the lack of ability to medialize the vocal cords. With a unilateral injury, hoarseness would not be an unexpected finding. One rare but feared complication is a bilateral injury to the recurrent laryngeal nerves, which would result in a lack of ability to close the airway with the true vocal folds, significantly increasing the risk of aspiration. Additionally, the external branch of the superior laryngeal nerve, in charge of innervating the cricothyroid muscle, may be damaged during a cricothyrotomy or thyroidectomy and would lead to an inability to tense the vocal cords resulting in a decreased pitch of the voice.