[1]
Tarabishy AB, Alexandrou TJ, Traboulsi EI. Syndrome of myelinated retinal nerve fibers, myopia, and amblyopia: a review. Survey of ophthalmology. 2007 Nov-Dec:52(6):588-96
[PubMed PMID: 18029268]
Level 3 (low-level) evidence
[2]
Lam BL, Morais CG Jr, Pasol J. Drusen of the optic disc. Current neurology and neuroscience reports. 2008 Sep:8(5):404-8
[PubMed PMID: 18713576]
[3]
Spencer TS, Katz BJ, Weber SW, Digre KB. Progression from anomalous optic discs to visible optic disc drusen. Journal of neuro-ophthalmology : the official journal of the North American Neuro-Ophthalmology Society. 2004 Dec:24(4):297-8
[PubMed PMID: 15662245]
[4]
Simonett JM, Winges KM. Vitreopapillary Traction Detected by Optical Coherence Tomography. JAMA ophthalmology. 2018 May 10:136(5):e180727. doi: 10.1001/jamaophthalmol.2018.0727. Epub 2018 May 10
[PubMed PMID: 29800255]
[5]
Loukianou E, Kisma N, Pal B. Evolution of an Astrocytic Hamartoma of the Optic Nerve Head in a Patient with Retinitis Pigmentosa - Photographic Documentation over 2 Years of Follow-Up. Case reports in ophthalmology. 2011 Feb 2:2(1):45-9. doi: 10.1159/000324037. Epub 2011 Feb 2
[PubMed PMID: 21347192]
Level 3 (low-level) evidence
[6]
Iovino C, Casini G, Peiretti E. Bilateral noncalcified astrocytic hamartomas in retinitis pigmentosa: Multimodal imaging evaluation over 8 years of follow-up. European journal of ophthalmology. 2019 Sep:29(5):NP18-NP21. doi: 10.1177/1120672118804386. Epub 2018 Oct 3
[PubMed PMID: 30280590]
[7]
Malmqvist L, Li XQ, Eckmann CL, Skovgaard AM, Olsen EM, Larsen M, Munch IC, Hamann S. Optic Disc Drusen in Children: The Copenhagen Child Cohort 2000 Eye Study. Journal of neuro-ophthalmology : the official journal of the North American Neuro-Ophthalmology Society. 2018 Jun:38(2):140-146. doi: 10.1097/WNO.0000000000000567. Epub
[PubMed PMID: 28841585]
[8]
Friedman AH, Gartner S, Modi SS. Drusen of the optic disc. A retrospective study in cadaver eyes. The British journal of ophthalmology. 1975 Aug:59(8):413-21
[PubMed PMID: 1203227]
Level 2 (mid-level) evidence
[10]
Grover S, Fishman GA, Brown J Jr. Frequency of optic disc or parapapillary nerve fiber layer drusen in retinitis pigmentosa. Ophthalmology. 1997 Feb:104(2):295-8
[PubMed PMID: 9052635]
[11]
Kim BJ, Fulton AB. The genetics and ocular findings of Alagille syndrome. Seminars in ophthalmology. 2007 Oct-Dec:22(4):205-10
[PubMed PMID: 18097983]
[12]
Georgalas I, Tservakis I, Papaconstaninou D, Kardara M, Koutsandrea C, Ladas I. Pseudoxanthoma elasticum, ocular manifestations, complications and treatment. Clinical & experimental optometry. 2011 Mar:94(2):169-80. doi: 10.1111/j.1444-0938.2010.00559.x. Epub 2010 Dec 29
[PubMed PMID: 21198842]
[13]
Tso MO. Pathology and pathogenesis of drusen of the optic nervehead. Ophthalmology. 1981 Oct:88(10):1066-80
[PubMed PMID: 7335311]
[15]
Harder B, Jonas JB. Frequency of spontaneous pulsations of the central retinal vein. The British journal of ophthalmology. 2007 Mar:91(3):401-2
[PubMed PMID: 17322474]
[16]
Ekdawi NS, Brodsky MC. Absence of spontaneous venous pulsations in children with pseudopapilloedema. The British journal of ophthalmology. 2011 Nov:95(11):1615-6. doi: 10.1136/bjophthalmol-2011-300363. Epub 2011 Jun 30
[PubMed PMID: 21719565]
[17]
Chang MY, Velez FG, Demer JL, Bonelli L, Quiros PA, Arnold AC, Sadun AA, Pineles SL. Accuracy of Diagnostic Imaging Modalities for Classifying Pediatric Eyes as Papilledema Versus Pseudopapilledema. Ophthalmology. 2017 Dec:124(12):1839-1848. doi: 10.1016/j.ophtha.2017.06.016. Epub 2017 Jul 18
[PubMed PMID: 28732589]
[18]
McNicholas MM, Power WJ, Griffin JF. Sonography in optic disk drusen: imaging findings and role in diagnosis when funduscopic findings are normal. AJR. American journal of roentgenology. 1994 Jan:162(1):161-3
[PubMed PMID: 8273656]
[19]
Almog Y, Nemet A, Nemet AY. Optic disc drusen demonstrate a hyperechogenic artifact in B mode ultrasound. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2016 Jan:23():111-119. doi: 10.1016/j.jocn.2015.08.005. Epub 2015 Sep 26
[PubMed PMID: 26412252]
[20]
Saenz R, Cheng H, Prager TC, Frishman LJ, Tang RA. Use of A-scan Ultrasound and Optical Coherence Tomography to Differentiate Papilledema From Pseudopapilledema. Optometry and vision science : official publication of the American Academy of Optometry. 2017 Dec:94(12):1081-1089. doi: 10.1097/OPX.0000000000001148. Epub
[PubMed PMID: 29120977]
[21]
Merchant KY, Su D, Park SC, Qayum S, Banik R, Liebmann JM, Ritch R. Enhanced depth imaging optical coherence tomography of optic nerve head drusen. Ophthalmology. 2013 Jul:120(7):1409-14. doi: 10.1016/j.ophtha.2012.12.035. Epub 2013 Mar 24
[PubMed PMID: 23531353]
[22]
Malmqvist L, Bursztyn L, Costello F, Digre K, Fraser JA, Fraser C, Katz B, Lawlor M, Petzold A, Sibony P, Warner J, Wegener M, Wong S, Hamann S. The Optic Disc Drusen Studies Consortium Recommendations for Diagnosis of Optic Disc Drusen Using Optical Coherence Tomography. Journal of neuro-ophthalmology : the official journal of the North American Neuro-Ophthalmology Society. 2018 Sep:38(3):299-307. doi: 10.1097/WNO.0000000000000585. Epub
[PubMed PMID: 29095768]
[23]
Malmqvist L, Sibony PA, Fraser CL, Wegener M, Heegaard S, Skougaard M, Hamann S, Optic Disc Drusen Studies Consortium. Peripapillary Ovoid Hyperreflectivity in Optic Disc Edema and Pseudopapilledema. Ophthalmology. 2018 Oct:125(10):1662-1664. doi: 10.1016/j.ophtha.2018.04.036. Epub 2018 Jun 8
[PubMed PMID: 29891127]
[24]
Traber GL, Weber KP, Sabah M, Keane PA, Plant GT. Enhanced Depth Imaging Optical Coherence Tomography of Optic Nerve Head Drusen: A Comparison of Cases with and without Visual Field Loss. Ophthalmology. 2017 Jan:124(1):66-73. doi: 10.1016/j.ophtha.2016.09.022. Epub 2016 Nov 3
[PubMed PMID: 27817914]
Level 3 (low-level) evidence
[25]
Nentwich MM, Remy M, Haritoglou C, Kampik A. Radial optic neurotomy to treat patients with visual field defects associated with optic nerve drusen. Retina (Philadelphia, Pa.). 2011 Mar:31(3):612-5. doi: 10.1097/IAE.0b013e318209b748. Epub
[PubMed PMID: 21336072]
[26]
Kapur R, Pulido JS, Abraham JL, Sharma M, Buerk B, Edward DP. Histologic findings after surgical excision of optic nerve head drusen. Retina (Philadelphia, Pa.). 2008 Jan:28(1):143-6. doi: 10.1097/IAE.0b013e31815e98d8. Epub
[PubMed PMID: 18185151]
[27]
Pfriem M, Hoerauf H. Unsuccessful surgical excision of optic nerve drusen. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2011 Oct:249(10):1583-5. doi: 10.1007/s00417-011-1693-x. Epub 2011 Jun 3
[PubMed PMID: 21638031]
[28]
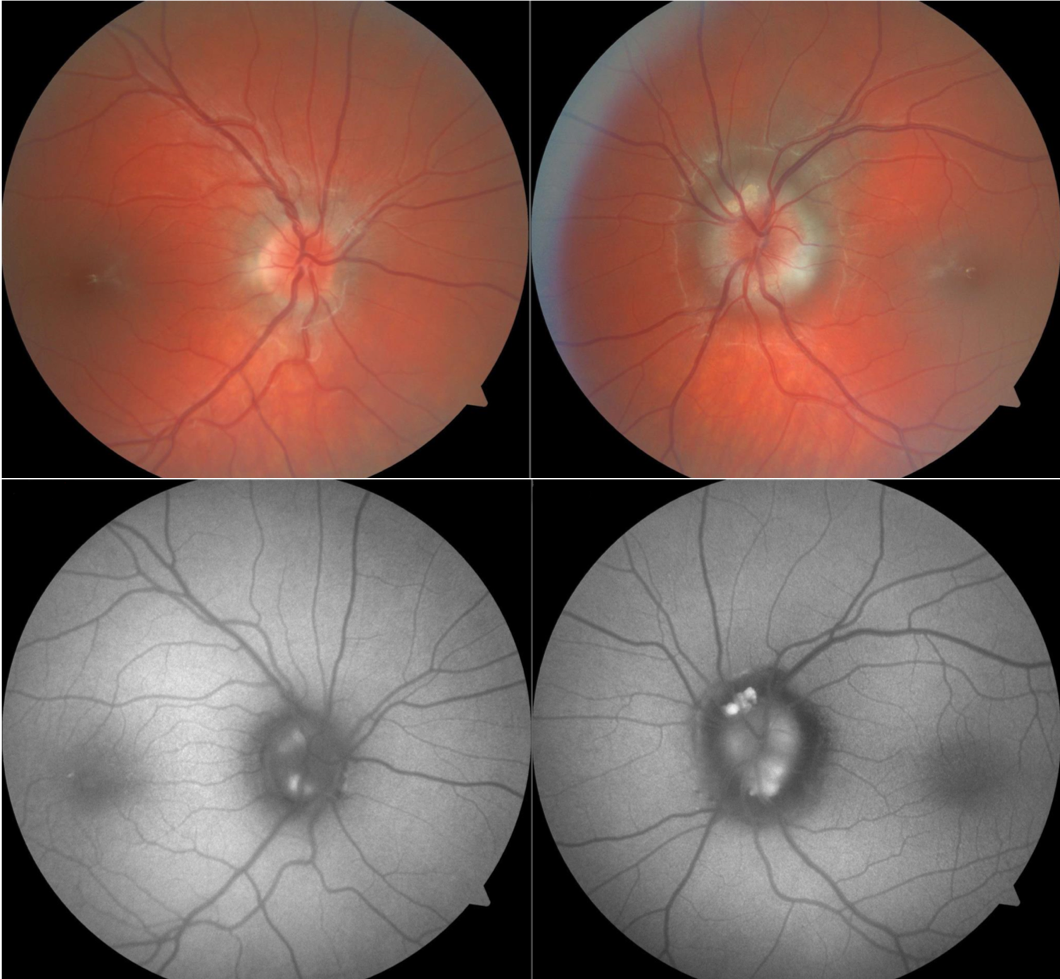
Pineles SL, Arnold AC. Fluorescein angiographic identification of optic disc drusen with and without optic disc edema. Journal of neuro-ophthalmology : the official journal of the North American Neuro-Ophthalmology Society. 2012 Mar:32(1):17-22. doi: 10.1097/WNO.0b013e31823010b8. Epub
[PubMed PMID: 21926917]
[29]
Hamann S, Malmqvist L, Costello F. Optic disc drusen: understanding an old problem from a new perspective. Acta ophthalmologica. 2018 Nov:96(7):673-684. doi: 10.1111/aos.13748. Epub 2018 Apr 16
[PubMed PMID: 29659172]
Level 3 (low-level) evidence
[30]
Lee AG, Zimmerman MB. The rate of visual field loss in optic nerve head drusen. American journal of ophthalmology. 2005 Jun:139(6):1062-6
[PubMed PMID: 15953437]
[31]
Skaat A, Muylaert S, Mogil RS, Furlanetto RL, Netto CF, Banik R, Liebmann JM, Ritch R, Park SC. Relationship Between Optic Nerve Head Drusen Volume and Structural and Functional Optic Nerve Damage. Journal of glaucoma. 2017 Dec:26(12):1095-1100. doi: 10.1097/IJG.0000000000000783. Epub
[PubMed PMID: 29045333]
[32]
Chang MY, Keltner JL. Risk Factors for Fellow Eye Involvement in Nonarteritic Anterior Ischemic Optic Neuropathy. Journal of neuro-ophthalmology : the official journal of the North American Neuro-Ophthalmology Society. 2019 Jun:39(2):147-152. doi: 10.1097/WNO.0000000000000715. Epub
[PubMed PMID: 30300257]
[33]
Farah SG, Mansour AM. Central retinal artery occlusion and optic disc drusen. Eye (London, England). 1998:12 ( Pt 3a)():480-2
[PubMed PMID: 9775256]
[34]
Chern S, Magargal LE, Annesley WH. Central retinal vein occlusion associated with drusen of the optic disc. Annals of ophthalmology. 1991 Feb:23(2):66-9
[PubMed PMID: 2029117]
[35]
Silva R, Torrent T, Loureiro R, Travassos A, de Abreu JR. Bilateral CNV associated with optic nerve drusen treated with photodynamic therapy with verteporfin. European journal of ophthalmology. 2004 Sep-Oct:14(5):434-7
[PubMed PMID: 15506607]
[36]
Berry S, Lin WV, Sadaka A, Lee AG. Nonarteritic anterior ischemic optic neuropathy: cause, effect, and management. Eye and brain. 2017:9():23-28. doi: 10.2147/EB.S125311. Epub 2017 Sep 27
[PubMed PMID: 29033621]