Continuing Education Activity
Lateral humeral condyle fractures are the second most commonly encountered elbow fractures after the supracondylar type in the pediatric age group. These injuries are peculiar as they are intraarticular but displacement-prone owing to the forearm extensor muscles' attachment on the lateral epicondyle close to the condylar area. Thus, complications, including elbow deformity, can emerge if this condition is not appropriately treated.
Diagnostic and management challenges may arise in cases of incomplete fractures and when extensive growth plate areas are involved. Understanding the injury mechanisms behind lateral humeral condyle fractures and the treatment nuances is crucial in navigating these challenges and optimizing patient outcomes.
This activity for healthcare workers is designed to enhance learners' competence in evaluating and managing lateral humeral condyle fractures. This course discusses the need to collaborate with an interprofessional team caring for patients with this injury.
Objectives:
Identify the signs and symptoms indicative of a lateral humeral condyle fracture in the pediatric population.
Develop a clinically guided diagnostic plan for a young patient with a possible lateral humeral condyle fracture.
Compare the various treatment options for lateral humeral condyle fractures and create a personalized management plan for a young individual with this injury.
Collaborate and communicate effectively with an interprofessional team in formulating short- and long-term care plans for young patients with lateral humeral condyle fractures.
Introduction
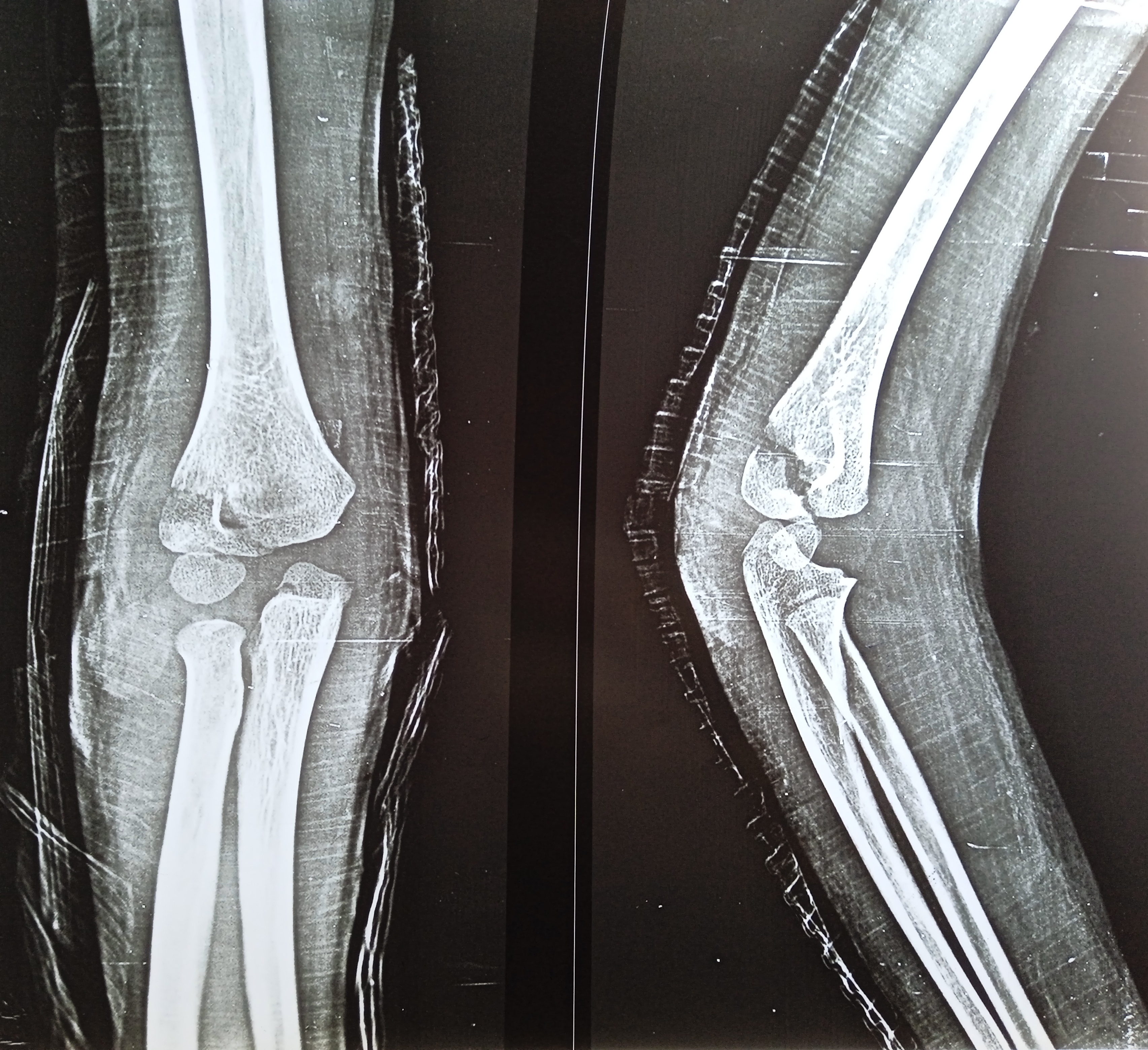
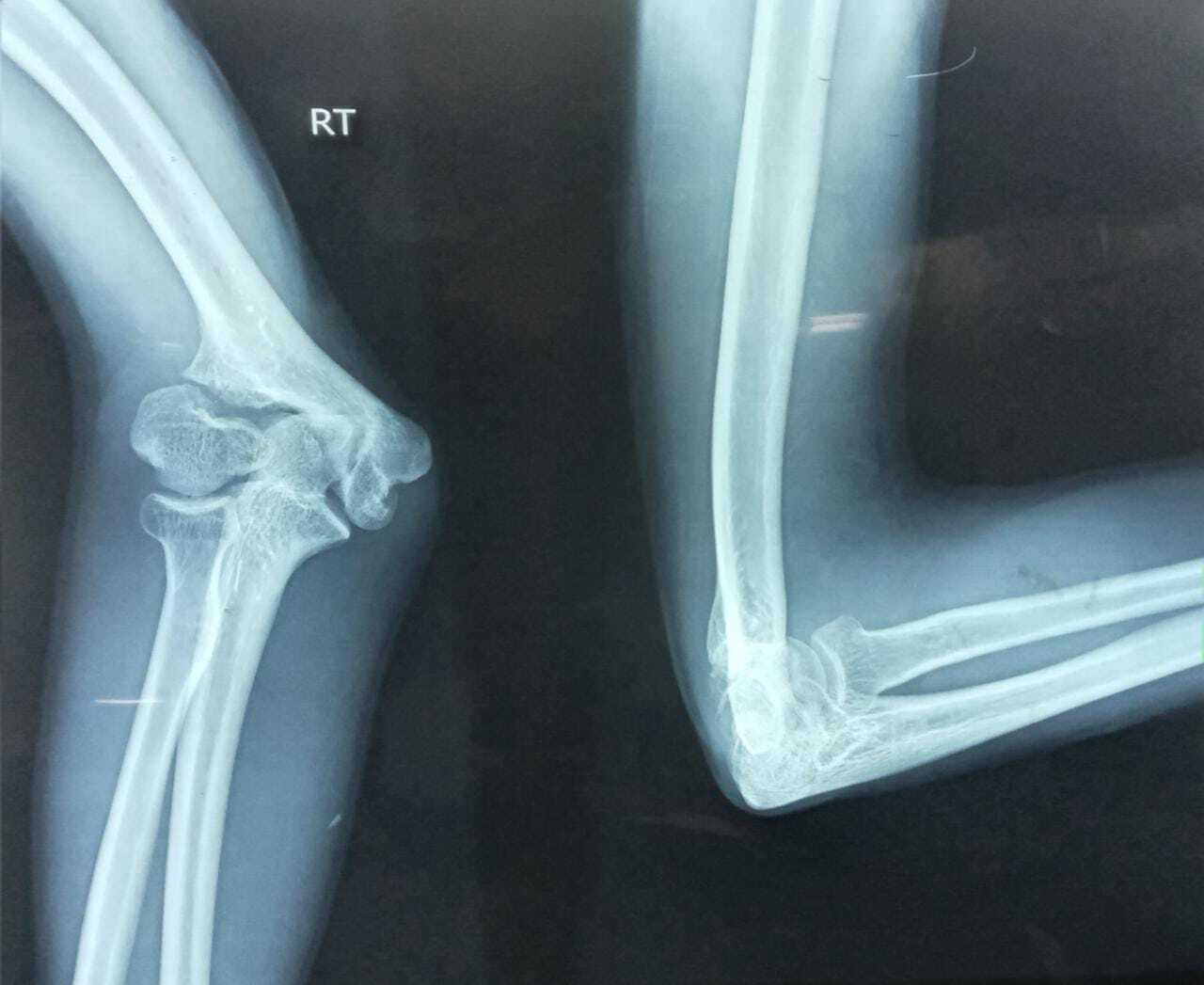
Lateral humeral condyle fractures are the second most commonly encountered pediatric elbow fractures next to supracondylar fractures (see Image. Lateral Humeral Condyle Fracture). These injuries are unique, being intraarticular but vulnerable to displacement and nonunion owing to the forearm extensors' pull on the lateral epicondyle near the condylar area. These fractures can result in complications like elbow deformity if not appropriately managed.[1]
A history of a fall onto an outstretched hand is common. Swelling, pain, restricted range of motion, and localized tenderness of the elbow are the usual presenting features. Lateral elbow ecchymosis may also be observed. Several classification systems have been developed to aid management, with a 2 mm displacement considered the surgical fixation cutoff. Displaced fractures are at a higher risk of nonunion. Malunion, cubitus varus, avascular necrosis, and post-operative infection are recognized complications following surgery.[2]
Anatomy of the Humerus
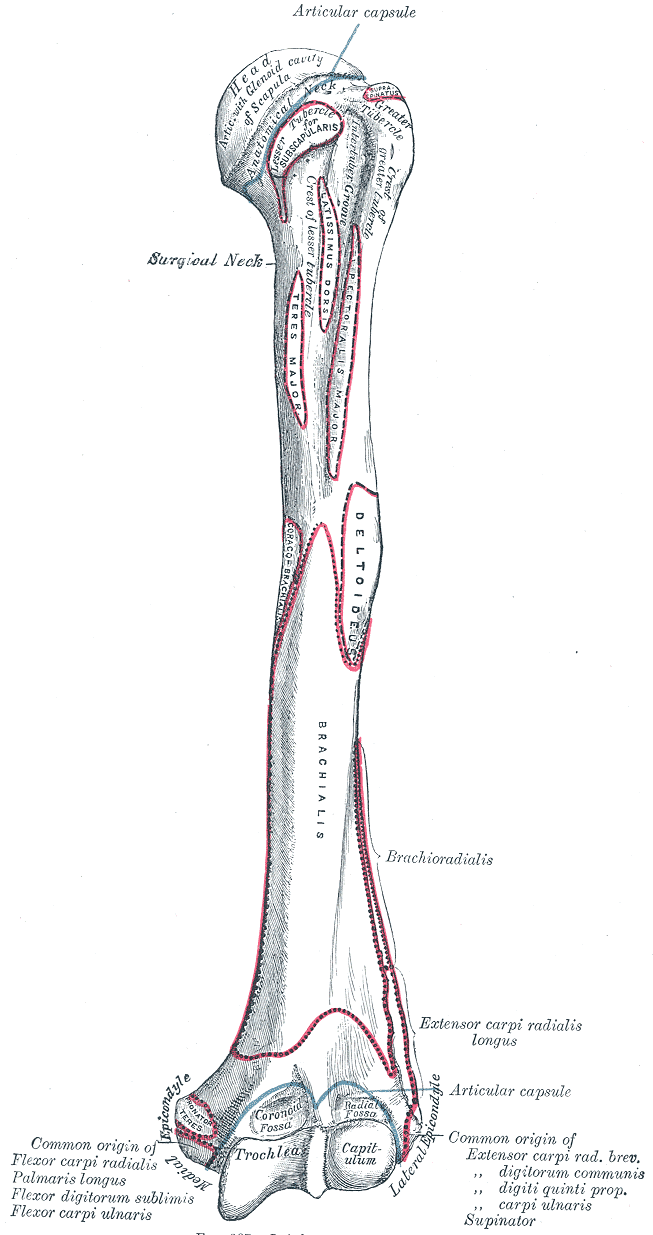
The arm bone or humerus is the largest upper limb bone (see Image. Upper Arm Anatomy). The humerus articulates with the scapula at the glenohumeral joint (shoulder) and the radius and ulna at the elbow joint. The proximal humeral segment comprises the head, greater and lesser tubercles, and surgical and anatomical necks. The humeral shaft has the deltoid tuberosity laterally and radial groove posteriorly. The arm bone widens distally, forming the lateral and medial supracondylar ridges superior to the elbow joint. Further distally are the angular-shaped lateral and medial epicondyles, flanking the condylar area. The humeral condyle forms the elbow joint with the radius and ulna and comprises the trochlea, capitulum, and olecranon, coronoid, and radial fossae.
The head is the part of the arm bone that articulates with the scapula's glenoid cavity. The anatomical humeral neck marks the attachment site of the glenohumeral joint capsule. The surgical neck is a slightly narrowed arm bone section distal to the humeral head and tubercles. The greater tubercle is a bony prominence at the lateral side of the humerus, while its anterior counterpart is the lesser tubercle. The intertubercular sulcus (bicipital groove) lies between the tubercles and houses the tendon of the long head of the biceps.
The deltoid tuberosity is the deltoid muscle's attachment site on the humeral shaft. The radial groove houses the radial nerve and profunda brachii artery. The lateral epicondyle lies lateral to the humeral condyle and provides an attachment site for the forearm extensors. Meanwhile, the medial epicondyle is a forearm flexor attachment site located medial to the humeral condyle.
Etiology
Trauma is invariably associated with lateral humeral condyle fractures. Falls account for most of the presentations. The most common mechanism is a fall on an outstretched hand with an extended elbow and the forearm supine.[3]
Epidemiology
This injury is the second most common pediatric elbow fracture, constituting 12% to 20% of all upper extremity fractures in children. The most commonly affected age group is between 4 and 10 years, with peak incidence at 6 years. Notably, left-side injury is more common. About 67.4% of these injuries occur in boys.[4][5][6] Frequently associated injuries include ipsilateral elbow dislocations (11.4%, posterolateral and posteromedial) and ipsilateral upper limb fractures (olecranon 2.8%, forearm 1.5%, and medial epicondyle 1.2%).[7]
Pathophysiology
Several theories have tried to elucidate the injury mechanisms behind lateral condyle fractures. Milch first proposed a push-off theory, where an upward and outward force applied through the radius creates the fracture. Meanwhile, Jakob defends a pull-off mechanism, where the extensor carpi radialis and brachioradialis avulse the lateral condyle during adduction of the supinated forearm.[8] Currently, a combination of both processes is accepted as the mechanism responsible for this injury. Direct elbow trauma and valgus impaction can also cause such fractures.[9] Most lateral condylar fractures are classified as Salter-Harris type IV or one transecting the metaphysis, physis, and epiphysis.
History and Physical
History of a fall onto an outstretched hand is common. Elbow swelling, pain, and movement difficulty are the usually reported symptoms. Lateral elbow ecchymosis may indicate an unstable fracture tearing the brachioradialis aponeurosis.
A thorough evaluation of the entire upper limb is warranted. Lateral elbow tenderness is usually present. The elbow's range of motion is generally restricted.
Neurovascular assessment during the initial presentation is crucial. The peripheral pulses, digital sensation, and finger movements must be examined in detail to rule out compartment syndrome. Skin laceration may indicate an open fracture, while skin tenting may signify an impending open fracture. Compartment syndrome and open fractures are orthopedic emergencies warranting immediate surgery.
Supracondylar fractures may also present with the same history and physical findings. However, this condition is more commonly associated with more severe elbow deformity and neurovascular deficits than lateral condyle injuries.[10]
Evaluation
Radiography is the initial imaging modality of choice for patients presenting with elbow pain, especially with a traumatic history. Plain radiographs must include anteroposterior, lateral, and internal oblique views of the affected elbow. An internal oblique view is useful in detecting minimally displaced fractures (less than 2 mm), as often happens when the fractured lateral condylar fragment lies posterolaterally.[11][12] The fracture displacement is defined as the maximum distance between the proximal and distal fragments in any of the radiographic views.[13]
An elbow arthrogram also helps arrive at the correct diagnosis and confirm the reduction intraoperatively. This modality is especially useful in evaluating minimally displaced fractures treated with closed reduction and percutaneous fixation.[14]
Computed tomography (CT) has proven helpful in characterizing fracture patterns and comminution.[15] However, conventional CT allows only limited articular cartilage evaluation.[10] Multidetector CT can provide more detailed, high-resolution images than conventional CT and may be more useful in treatment decision-making.[16]
Magnetic resonance imaging (MRI) can help assess articular cartilage integrity.[17] An intact elbow articular cartilage indicates fracture stability and a low late displacement risk.[18][19] However, MRI is infrequently ordered as it requires child sedation and additional costs. Ultrasonography may be used instead of MRI to look for fracture displacement in younger children.[20] Arthroscopy of the elbow may also aid in diagnosis and fracture reduction.[21]
Multiple classifications have been suggested for pediatric lateral humeral condyle fractures. The classification by Milch et al distinguishes between type I and II patterns. Type I is characterized by a fracture line lateral to the trochlear groove. This injury is considered stable as it does not extend to the trochlear groove. In contrast, a type II fracture extends medially into the trochlear groove, thus creating a potentially unstable elbow.[4] The Milch classification tried to predict elbow displacement but did not correlate with intraoperative findings. Additionally, the Milch system presented limited recommendations on treatment.[22]
A second classification by Jakob and Weiss divides fracture patterns into 3 types according to displacement and articular cartilage congruency. Type I has less than 2 mm displacement. Type II has a 2 mm displacement or greater, but the articular cartilage is intact. Type III also has a 2 mm displacement or greater, but articular disruption is evident.[23]
Later, Song et al also described a classification scheme based on fracture pattern, displacement, and stability. According to this system, stage 1 fractures have less than 2 mm displacement, are stable, and have a small metaphyseal fracture line. Stage 2 fractures have less than 2 mm displacement, may or may not be stable, and have a lateral fracture gap. Stage 3 fractures have less than 2 mm displacement, are unstable, and have lateral and medial fracture gaps. Stage 4 fractures have displacement greater than 2 mm, are unstable and do not have fracture fragment rotation. Stage 5 fractures have displacement greater than 2 mm, are unstable, and have fracture fragment rotation.[13]
Treatment / Management
Nonoperative Management of Pediatric Lateral Condyle Fractures
Conservative treatment with an above-elbow cast is generally indicated in less displaced fractures, i.e., with less than 2 mm displacement. The union rate is 98% when meeting this criterion.[24] Immobilization is advised for a minimum of 4 weeks. Further immobilization for another 2 weeks may be indicated, depending on the extent of fracture healing at this stage.[25]
Repeat radiographs are recommended at 1 week posttreatment to rule out fracture displacement. Aggravation of mildly displaced lateral condyle fractures may occur until the 7th day, regardless of the splint angle, absence of the fat pad sign, age, or gender.[26]
Surgical Interventions for Pediatric Lateral Condyle Fractures
Surgical management aims to reduce the articular surface anatomically. Surgical indications for these injuries include fracture displacement greater than 2 mm, articular surface incongruency, and loss of reduction on serial radiographs. A retrospective study reported that surgical delay more than 24 hours postinjury did not influence the clinical and functional results for pediatric lateral humeral condylar fractures with displacement greater than 2 mm. However, delayed open reduction and Kirschner-wire fixation may increase the incision length, probably due to increased edema.[27] Closed reduction with percutaneous fixation is a minimally invasive option, mainly for Weiss type 2 and Song stages 2 to 4 fractures.
Using 2 instead of 3 Kirschner wires during percutaneous fixation is recommended to achieve stability. This technique can improve the elbow's range of motion and reduce bone spur formation. The wire may be removed when clinical and radiological evidence of fracture healing has been obtained. Removal typically occurs around 4 to 6 weeks.[28] A finite element analysis demonstrated that an angle of -60° between the 2 pins in the sagittal plane provided the greatest stability in pediatric lateral humeral condyle fractures. Divergent configurations were also shown to be superior to parallel pinning at this angle.[29]
A comparative study revealed that in Kirschner-wire fixation of Jakob type 2 pediatric lateral humeral condylar fractures, ultrasound guidance was more helpful than arthrography guidance in avoiding open reduction and decreasing the number of intraoperative fluoroscopies, with good effectiveness.[30] Another comparative investigation found that both biodegradable pins and Kirschner wires were safe and effective for pediatric lateral humeral condylar fracture fixation. Both also produced satisfactory and comparable clinical outcomes. However, biodegradable pins had the advantages of having fewer long-term complications, showing less hardware prominence, and not requiring hardware removal.[31]
Fixation with cannulated screws may be an option with similar outcomes. This approach can prevent skin infections commonly associated with Kirschner wires, although these devices require another surgery for removal.[32]
Open reduction and internal fixation (ORIF) is recommended if minimally invasive procedures fail. A comparative study demonstrated that an anterolateral approach for open reduction of pediatric lateral humeral condylar fractures had better radiographic and clinical outcomes than a posterolateral approach and was thus suggested as the optimal technique.[33] ORIF is indicated for Weiss type 3 and Song stage 5 fractures. Lag screw osteosynthesis is recommended when performing an ORIF due to its lower rates of malreduction and subsequent complications.[34]
Kirschner-wire fixation remains a valid alternative in these situations. An observational cross-sectional study reported that both closed reduction with percutaneous pinning and ORIF can achieve satisfactory clinical outcomes in pediatric lateral humeral condyle fractures with displacement greater than 4 mm. The study found no differences in complications or prognoses between the 2 groups. However, closed reduction with percutaneous pinning had the advantages of less invasiveness, less scarring, and not needing a second surgery under anesthesia for pin removal.[35]
A meta-analysis found that closed reduction with pinning had efficacy and safety similar to ORIF with pinning in managing pediatric humeral lateral condylar fractures. However, closed reduction with percutaneous pinning had the benefit of eliminating unaesthetic scars.[36]
Differential Diagnosis
The following conditions must be ruled out when evaluating pediatric lateral condylar fractures:
- Other ipsilateral upper limb fractures
- Supracondylar fractures
- Ipsilateral posterolateral or posteromedial elbow dislocation
These conditions require different management approaches and may be distinguished from pediatric lateral condylar fractures after a thorough evaluation.
Prognosis
The prognosis of pediatric lateral condyle fractures is favorable when promptly diagnosed and managed. The overall reported union rates for these injuries are 91%. Delayed presentation is associated with future range-of-motion limitation and avascular necrosis. The prognosis largely depends on accurate fracture classification and intervention appropriateness. Fracture displacement is also a significant factor in clinical outcomes. A displacement of 2 mm appears to be a recommendable cutoff for conservative management due to fewer complications.[37]
Complications
The complication rate is less with the less severe fracture types. For example, surgically managed Weiss type II fractures (11%) seem to have lower complication rates associated with Weiss type III injuries (34%). A prominent lateral condyle is the most frequent complication found in 27% of cases, but this condition does not appear to influence clinical outcomes.
Fracture malunion can occur if the fragments join in a nonanatomical position. Malunion can lead to posttraumatic elbow arthritis if articular surface malreduction occurs. Deformities like cubitus varus or cubitus valgus may also result from malunion.[38] A delayed union can occur in 1% of cases and is commonly managed conservatively.
Lateral condyle fractures are generally intraarticular (Salter-Harris IV). Growth arrest can occur when the ossific nucleus is involved. Fishtail deformities and avascular necrosis can develop in 14% and 1.7% of cases, respectively. A fishtail deformity is a characteristic distal humeral deformity arising from a lack of communication between the lateral trochlear ossification centers. Medial instability between epiphyseal plates can arise from this condition. Lag screw osteosynthesis seems to reduce the risk of fishtail deformities or avascular necrosis. Thus, the technique is favored when open reduction is required.
Nonunion seems more common with lateral condyle fractures than other elbow fractures (see Image. Complications of a Lateral Humeral Condyle Fracture). Prior studies have placed the risk between 1% and 5%, depending on the definition. Pace et al reported that the risk of nonunion in these injuries was 1.4%, with nonunion defined as the absence of callus 8 weeks after definitive treatment with fracture migration. All cases that underwent nonunion surgery achieved union.[39]
Several osteotomy techniques have been reported to correct cubitus valgus deformity associated with ununited lateral condyle fractures. Each technique has advantages. Recently, medial trapezoidal osteotomy was described as an effective method for treating pediatric lateral humeral condyle fracture nonunion with cubitus valgus deformity.[40] Another study described ORIF with screws and combined autologous tricortical iliac bone graft reconstruction as an effective technique for managing cubitus valgus from neglected ununited pediatric lateral humeral condyle fractures.[41]
Lateral condyle fracture healing often leads to a wider distal humerus. Cubitus varus develops in more than 20% of patients, while a valgus deformity can occur in more than 10%. These deformities alter the normal physiological carrying angle (5° to 15°). Healing in a slightly displaced fashion compared to the initial position seems responsible for a varus deformity. A bony prominence can sometimes be felt clinically or seen radiologically with little significance.[42]
However, pseudo-cubitus varus has been reported to be more prevalent than true cubitus varus. A 3.7 mm increase in interepicondylar width can predict true cubitus varus. The risk of cubitus varus increases in Song classification stages 3, 4, and 5.[43]
Tardy ulnar nerve palsy is usually a consequence of lateral condyle fracture nonunion. Continued skeletal development causes a cubitus valgus deformity, leading to ulnar nerve stretching and classic neuropathic symptoms. Paraesthesia is usually late-onset, and examination may reveal intrinsic hand muscle atrophy.[10]
Postoperative and Rehabilitation Care
Kirschner wires are removed after 4 to 6 weeks. Additional casting for 2 to 4 weeks is recommended after Kirschner-wire removal. Immobilization in an above-elbow long-arm cast is indicated until clinical and radiographic healing are achieved. Range-of-motion exercises are initiated following cast removal. However, contact sports and heavy weightlifting should be avoided for 1 to 2 months after cast removal.
Bernthal et al found that the mean motion arc at the time of cast removal after percutaneous pinning was 64°. Patients treated surgically had a slower recovery, but no significant differences were observed beyond week 18. Older age, longer immobilization, and more severe injuries are also associated with slower recoveries.[44]
Deterrence and Patient Education
Primary prevention of pediatric lateral condyle fractures aims to minimize the risk of falls and trauma and promote a safe environment for children. Here are some preventive measures:
- Ensuring proper adult supervision during playtime
- Choosing play areas with soft surfaces and age-appropriate equipment
- Childproofing the home environment, eg, by covering sharp corners and installing safety gates at the top and bottom of the stairs
- Ensuring that children wear helmets, appropriate footwear, and proper sports attire during sports activities
- Enrolling children in organized sports programs with qualified coaches who emphasize proper techniques and safety measures
- Encouraging activities that improve balance and coordination
- Counseling parents and caregivers about the importance of injury prevention measures
- Addressing any underlying conditions that may affect children's bone health
- Collaborating with school authorities to implement educational programs regarding injury prevention, safety rules, and the importance of reporting any incidents to adults
These preventive measures can minimize the likelihood of pediatric lateral condyle fractures, though not all are avoidable. Secondary prevention following such injuries entails clear communication between clinicians, patients, and patients' guardians. Prognostication about the management course and outcomes and potential complications must be discussed. Families must be enlightened about the correlation between injury severity and the likelihood of complications, even after surgery. The importance of physiotherapy and rehabilitation to elbow and overall functional recovery must be emphasized. Rehabilitation and elbow motion arc recovery after a pediatric lateral condyle fracture can take up to a year.
Pearls and Other Issues
Lateral humeral condyle fractures are common pediatric injuries. Due to the condition's traumatic etiology, thorough assessment and imaging are crucial to management decision-making. The Weiss and Song classification schemes may be used to categorize these fractures and help in treatment planning. A cutoff of 2 mm displacement is generally acceptable when deciding between conservative or surgical management.
For conservative management, immobilization for 4 to 6 weeks is the general approach. For surgical interventions, closed reduction and pinning with 2 Kirschner wires is the first option for less severe injuries and cases unresponsive to nonoperative treatment. This minimally invasive procedure has comparable results to ORIF for low-level injuries and is associated with better cosmetic outcomes. ORIF may be recommended for Weiss type 3 and Song stage 5 fractures.
Recovery of the elbow arc of motion will occur up to a year postinjury. Nonunion, avascular necrosis, and fishtail deformity are some complications that can occur.[33]
Enhancing Healthcare Team Outcomes
Pediatric lateral humeral condyle fractures are complex elbow injuries requiring an interprofessional approach. Initial assessment with neurovascular documentation is the first crucial step for the emergency medicine physician or primary care pediatrician. Radiologists can recommend the appropriate imaging modalities and share their findings with the team to guide treatment planning. Orthopedic surgeons' expertise is crucial in deciding between conservative and operative management and performing the necessary procedures.
Nurses are paramount in spotting neurovascular compromise during the initial assessment or postoperative period. Rehabilitation is also key to ensuring good outcomes following this injury. Thus, physiotherapists' efforts are crucial to restoring as much elbow function for the patient as possible.
Communication and collaboration are vital components of an effective interprofessional approach. Each team member's unique expertise and skills can address various aspects of care, ensuring a holistic approach to managing pediatric lateral condyle fractures.