Introduction
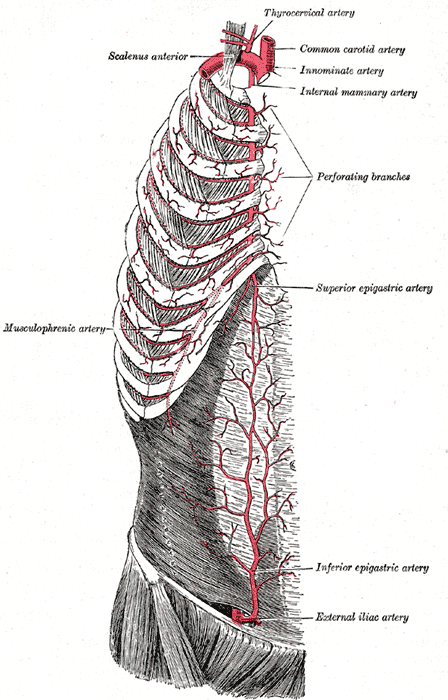
The internal thoracic artery, aka the internal mammary artery, supplies the breast and the anterior chest wall. The internal thoracic artery travels along the inner surface of the anterior chest wall on both sides. When it reaches the sixth or seventh intercostal cartilage, it divides into two branches: the musculophrenic and the superior epigastric arteries. The internal thoracic artery arises a few centimeters away from the origin of the subclavian artery. The artery then descends along the inner wall of the anterior rib cage. It is located about two to three centimeters on either side of the sternum and is slightly medial to the nipple. It is almost always accompanied by the large internal thoracic veins that also follow the same course. The internal thoracic artery runs under the fascia and deep to the intercostal muscles. In the proximal part, the internal thoracic artery also gives off other vessels which supply the breast, thymus, mediastinum, and sternum. At each intercostal rib, it gives off an anterior and posterior branch. The internal thoracic artery can be seen pulsating in some cases. It continues its downward course until it reaches the seventh intercostal space and then gives off the superior epigastric and musculophrenic arteries. The superior epigastric artery continues inferiorly along the abdominal wall until it travels just below the umbilicus, where it connects with the inferior epigastric artery. The musculophrenic artery follows the costal margin and supplies the diaphragm.
Structure and Function
The left subclavian artery directly originates as a branch of the arch of the aorta. The right subclavian artery arises as the brachiocephalic artery, also known as the innominate artery, splits into two arteries: the right common carotid artery and the right subclavian artery. On both the right and left side of the body, the subclavian artery gives rise to the vertebral artery, internal thoracic artery, thyrocervical trunk, costocervical trunk, and dorsal scapular artery before becoming the axillary artery when it crosses the lateral border of the first rib.
The internal thoracic artery branches off the proximal portion of the subclavian artery and begins its descent along the inner surface of the anterior chest wall. The internal thoracic arteries travel inferiorly and are located approximately 1-2 centimeters lateral to the sternal margin on either side. It travels in between the transversus thoracis muscle posteriorly and the internal intercostal muscles and costal cartilages anteriorly. It continues to descend inferiorly, giving off anterior intercostal arteries at each intercostal space and perforating cutaneous branches along the thorax. Once it reaches the sixth to seventh costal cartilage, the internal thoracic artery bifurcates into its terminal branches, the musculophrenic artery, and the superior epigastric artery.
To recap, the internal thoracic artery originates off of the subclavian artery, giving off several branches as it descends along the inner surface of the anterior thorax:
- Anterior intercostal arteries at each intercostal space
- Perforating cutaneous branches
- Pericardiophrenic artery
- Musculophrenic artery (terminal branch)
- Superior epigastric artery (terminal branch)
Blood Supply and Lymphatics
The internal thoracic artery supplies the anterior chest wall from the clavicle to the umbilicus, including the sternum and breasts. The thoracic artery also gives off the pericardiophrenic artery, which travels along the length of the pericardium towards the diaphragm, where it anastomoses with the musculophrenic and superior phrenic arteries. It functions to supply the mediastinum, thymus, and pericardium.
There have been cases reported of malignancy of these internal thoracic lymph nodes as an incidental finding during mobilization of the internal thoracic artery for coronary artery bypass grafting.[1][2]
Physiologic Variants
There are several anatomic variants of the internal thoracic artery. It becomes crucial to be aware of these variations in the surgical setting, most often during coronary artery bypass grafting, as the left internal thoracic artery is the conduit of choice for coronary bypass. In cadaveric studies, the internal thoracic artery has been reported to arise from the distal subclavian artery rather than the proximal portion.[3] Another variation identified was the common origin of the internal thoracic artery with the branches of the thyrocervical trunk. Reports also document a third terminal branch, a xiphoid branch, with trifurcation occurring in 20-30% of cadavers studied.[4]
Surgical Considerations
Coronary Artery Bypass Grafting
Coronary arteries are the vessels that provide oxygenated blood to the myocardium. These vessels are often affected by atherosclerotic plaques, resulting in stenosis of the vessel. This stenosis results in a decrease in perfusion to the myocardium, often presenting in a patient as angina. The decrease or complete lack of perfusion may result in myocardial infarction. Coronary artery bypass grafting is a surgical procedure used to restore blood flow to the myocardium through the use of a conduit to bypass a stenotic segment of the coronary artery. The left anterior descending (LAD) artery is a branch of the left coronary artery that supplies approximately 50% of the left ventricle and is considered the most significant vessel in myocardial blood supply. In coronary artery bypass grafting, the left internal thoracic artery is often used to bypass a stenotic segment of the left anterior descending artery. The left internal thoracic artery’s anatomic vicinity to the heart, long-term patency, long-term survivability, and post-operative quality of life render it the superior vessel for coronary artery bypass grafting compared to alternatives.[5] Coronary surgeons often reserve the left internal thoracic artery for left anterior descending artery occlusions. The great saphenous vein, right internal thoracic artery, and radial arteries are often seen as alternatives and used for other coronary artery vessels that require grafting.
Clinical Significance
Coarctation of the aorta is a congenital anomaly in which there is a narrowing of the aorta, resulting in increased pressure proximal to the narrowing and decreased perfusion distal to it. There are three varieties of aortic coarctations: preductal, ductal, and postductal. Each of these classifications is named relative to the ductus arteriosus, which connects the main pulmonary artery to the proximal descending aorta. The ductus arteriosus closes at birth and becomes the ligamentum arteriosum within three weeks of closure. In the postductal form of coarctation of the aorta, the narrowing occurs distal to the ductus arteriosus. This variant is the most common form in adults, often presenting as upper extremity hypertension and weak pulses in the lower extremities. The internal thoracic artery plays a significant role in providing collateral circulation to the lower extremities in postductal coarctation. The increased blood pressure and flow through vessels proximal to the coarctation results in increased flow through the subclavian artery and into the internal thoracic artery, anterior intercostal artery, posterior intercostal artery, and then into the descending thoracic aorta. The intercostal collateral vessels become dilated and tortuous, eroding the inferior margins of the ribs. This erosive process shows up as rib notching on chest x-ray, a classic sign seen in postductal coarctation of the aorta.