[2]
Matarese A, Sardu C, Shu J, Santulli G. Why is chronic obstructive pulmonary disease linked to atrial fibrillation? A systematic overview of the underlying mechanisms. International journal of cardiology. 2019 Feb 1:276():149-151. doi: 10.1016/j.ijcard.2018.10.075. Epub 2018 Oct 25
[PubMed PMID: 30446289]
Level 3 (low-level) evidence
[3]
Pan MM, Zhang HS, Sun TY. [Value of forced expiratory volume in 6 seconds (FEV(6)) in the evaluation of pulmonary function in Chinese elderly males]. Zhonghua yi xue za zhi. 2017 May 30:97(20):1556-1561. doi: 10.3760/cma.j.issn.0376-2491.2017.20.011. Epub
[PubMed PMID: 28592061]
[4]
Zakaria R, Harif N, Al-Rahbi B, Aziz CBA, Ahmad AH. Gender Differences and Obesity Influence on Pulmonary Function Parameters. Oman medical journal. 2019 Jan:34(1):44-48. doi: 10.5001/omj.2019.07. Epub
[PubMed PMID: 30671183]
[5]
Gao C, Zhang X, Wang D, Wang Z, Li J, Li Z. Reference values for lung function screening in 10- to 81-year-old, healthy, never-smoking residents of Southeast China. Medicine. 2018 Aug:97(34):e11904. doi: 10.1097/MD.0000000000011904. Epub
[PubMed PMID: 30142794]
[6]
Shapira U, Krubiner M, Ehrenwald M, Shapira I, Zeltser D, Berliner S, Rogowski O, Shenhar-Tsarfaty S, Bar-Shai A. Eosinophil levels predict lung function deterioration in apparently healthy individuals. International journal of chronic obstructive pulmonary disease. 2019:14():597-603. doi: 10.2147/COPD.S192594. Epub 2019 Mar 7
[PubMed PMID: 30880949]
[7]
Derom E, van Weel C, Liistro G, Buffels J, Schermer T, Lammers E, Wouters E, Decramer M. Primary care spirometry. The European respiratory journal. 2008 Jan:31(1):197-203. doi: 10.1183/09031936.00066607. Epub
[PubMed PMID: 18166597]
[8]
Gallucci M, Carbonara P, Pacilli AMG, di Palmo E, Ricci G, Nava S. Use of Symptoms Scores, Spirometry, and Other Pulmonary Function Testing for Asthma Monitoring. Frontiers in pediatrics. 2019:7():54. doi: 10.3389/fped.2019.00054. Epub 2019 Mar 5
[PubMed PMID: 30891435]
[11]
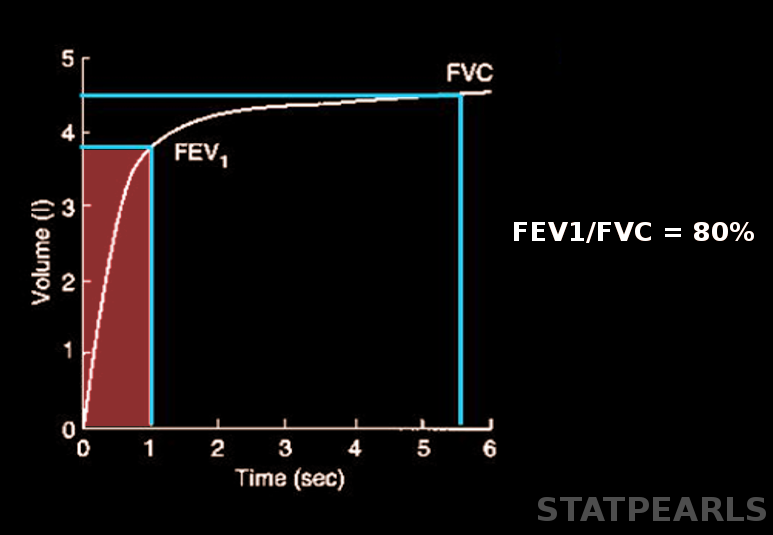
Fortis S, Comellas A, Make BJ, Hersh CP, Bodduluri S, Georgopoulos D, Kim V, Criner GJ, Dransfield MT, Bhatt SP, COPDGene Investigators–Core Units: <italic>Administrative Center</italic>, COPDGene Investigators–Clinical Centers: <italic>Ann Arbor VA</italic>. Combined Forced Expiratory Volume in 1 Second and Forced Vital Capacity Bronchodilator Response, Exacerbations, and Mortality in Chronic Obstructive Pulmonary Disease. Annals of the American Thoracic Society. 2019 Jul:16(7):826-835. doi: 10.1513/AnnalsATS.201809-601OC. Epub
[PubMed PMID: 30908927]
[12]
Carsin AE, Fuertes E, Schaffner E, Jarvis D, Antó JM, Heinrich J, Bellisario V, Svanes C, Keidel D, Imboden M, Weyler J, Nowak D, Martinez-Moratalla J, Gullón JA, Sanchez Ramos JL, Caviezel S, Beckmeyer-Borowko A, Raherison C, Pin I, Demoly P, Cerveri I, Accordini S, Gislason T, Toren K, Forsberg B, Janson C, Jogi R, Emtner M, Gómez Real F, Raza W, Leynaert B, Pascual S, Guerra S, Dharmage SC, Probst-Hensch N, Garcia-Aymerich J. Restrictive spirometry pattern is associated with low physical activity levels. A population based international study. Respiratory medicine. 2019 Jan:146():116-123. doi: 10.1016/j.rmed.2018.11.017. Epub 2018 Dec 15
[PubMed PMID: 30665509]
[13]
Chen G, Jiang L, Wang L, Zhang W, Castillo C, Fang X. The accuracy of a handheld "disposable pneumotachograph device" in the spirometric diagnosis of airway obstruction in a Chinese population. International journal of chronic obstructive pulmonary disease. 2018:13():2351-2360. doi: 10.2147/COPD.S168583. Epub 2018 Aug 2
[PubMed PMID: 30122915]
[14]
Reyes-García A, Torre-Bouscoulet L, Pérez-Padilla R. CONTROVERSIES AND LIMITATIONS IN THE DIAGNOSIS OF CHRONIC OBSTRUCTIVE PULMONARY DISEASE. Revista de investigacion clinica; organo del Hospital de Enfermedades de la Nutricion. 2019:71(1):28-35. doi: 10.24875/RIC.18002626. Epub
[PubMed PMID: 30810541]