Continuing Education Activity
The pectoral nerve (Pecs) block I and II are a novel technique to block the pectoral nerves, intercostal nerves 3 to 6, intercostobrachial nerves, and the long thoracic nerves. The technique is simple to perform, and the clinician can perform it with little or no sedation in the pre-operative holding area. This activity outlines Pecs block I and II and highlights the role of the healthcare team in improving care for patients undergoing a variety of anterior chest wall surgeries, most commonly breast surgery.
Objectives:
- Summarize the anatomy that needs to be visualized to perform a Pecs block properly.
- Describe the indications for performing a Pecs block.
- Identify the most common adverse events associated with a Pecs block.
- Explain the importance of collaboration and communication amongst the interprofessional team to improve outcomes for patients after anterior chest wall surgery.
Introduction
The pectoral nerve (Pecs) block I and II are a novel technique to block the pectoral nerves, intercostal nerves 3 to 6, intercostobrachial nerves and the long thoracic nerve. These blocks can be used to provide analgesia for a variety of anterior thoracic wall surgeries, most commonly breast surgery. The technique is simple for the clinician to perform and requires little or no sedation in the pre-operative holding area. Blanco et al. first described the Pecs I block in 2011 as a high volume interfascial block between the pectoralis major muscle and pectoralis minor muscle, targeting the lateral pectoral nerves.[1] In 2012, Blanco et al. described a second version of the Pecs block called modified Pecs block or Pecs II block. The Pecs II targets the interfacial plane between the pectoralis major muscle and the pectoralis minor muscle as does the Pecs I but also targets the interfacial plane between the pectoralis minor muscle and the serratus anterior muscle, aiming to block intercostal nerves 3 to 6, intercostobrachial and the long thoracic nerves, all of which are necessary for axillary node dissection.[2] A recent meta-analysis included 14 different randomized trials looking at Pecs II block versus paravertebral blocks and found no differences in opioid utilization or pain scores between the groups in patients undergoing breast cancer surgery. Also, Pecs II blocks were found to be non-inferior to paravertebral blocks when looking at 24-hour morphine utilization and pain intensity following surgery. When compared to systemic analgesia only, both were superior.[3][4][5][6][7]
Anatomy and Physiology
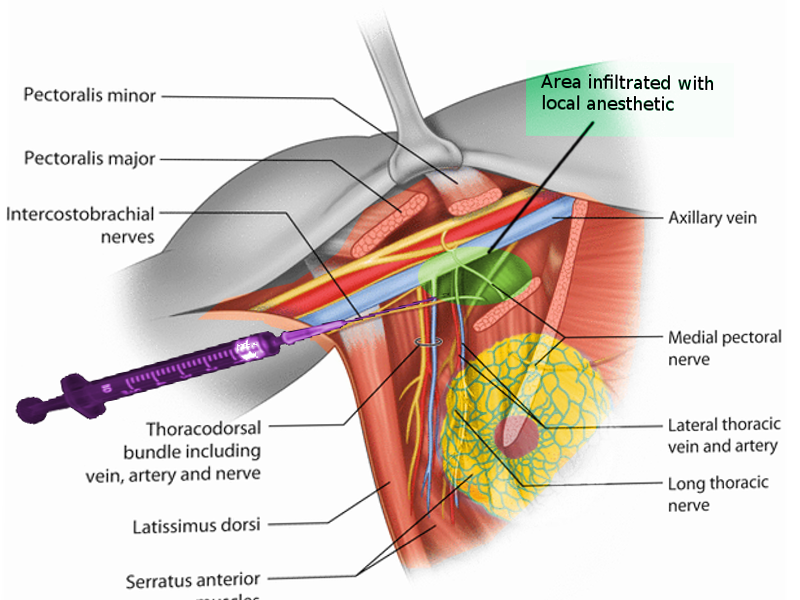
A Pecs I block requires an interfascial injection of local anesthetic between the pectoralis major muscle and pectoralis minor muscle at the level of the third rib to block both the medial pectoral nerve and lateral pectoral nerve. Utilizing ultrasound, the major landmarks visualized are the pectoralis major muscle, pectoralis minor muscle, and the thoracoacromial artery (pectoral branch).
The Pecs II block is a modified Pecs I block and can be achieved using a single needle stick. Local anesthetic placement is between the pectoralis major and pectoralis minor as for a Pecs I block and then between pectoralis minor and serratus anterior. The second portion of the procedure will block the anterior cutaneous branches of intercostal nerves 3 to 6, the intercostobrachial nerves, and the long thoracic nerve. The main landmarks to identify under US guidance are the pectoralis major muscle, pectoralis minor muscle, serratus anterior, and the thoracoacromial artery (pectoral branch).
Indications
The Pecs I and II blocks can be useful in delivering regional analgesia for a wide variety of surgical procedures including insertion of breast expanders and submuscular prostheses, ports, pacemakers, implantable cardiac defibrillators, anterior thoracotomies, anterior shoulder surgery, tumor resection, mastectomies, sentinel node biopsy, and axillary dissection.[8][9][10]
Contraindications
Patient refusal or infection at the site of injection are absolute contraindications to performing a Pecs block.
Anticoagulation may be a relative contraindication to Pecs block I and II, although there are no specific guidelines. The 2018 ASRA consensus statement does not specifically address Pecs blocks and anticoagulation.
Equipment
- Chlorhexidine gluconate
- Sterile gloves
- High-frequency linear ultrasound probe with sterile probe cover and gel
- 22G regional block needle, 50 to 100 mm
- Pecs Block local anesthetic solution (0.25% bupivacaine or 0.5% ropivacaine 20 to 40 ml)
- Epidural catheter (optional)
Personnel
An anesthesiologist with regional anesthesia and ultrasound experience is preferred. An additional assistant, nurse, or physician, should be available to assist.
Preparation
An informed consent, including risks and benefits of the procedure, should be performed before the procedure.
A procedure timeout should be performed to confirm procedure type, location, and to confirm there are no contraindications to the procedure.
Standard patient monitoring should be utilized, including continuous ECG, pulse oximetry, and non-invasive blood pressure monitoring. Intravenous access should be established in advance of the procedure. Resuscitation equipment, including medications for treating local anesthetic toxicity and equipment for intubation, should readily available.
The surgical staff should prep the patient with chlorhexidine gluconate, and sterility maintained for the duration of the procedure. All staff should wear a mask, surgical cap, and sterile gloves. A sterile ultrasound probe cover is also necessary during imaging.
Technique or Treatment
The Pecs I block is performed with the patient supine, with the patient's arm next to the body or abducted 90 degrees. The coracoid process is located on ultrasound in the paramedian sagittal plane. The caudal border of the transducer can then be rotated laterally to allow for an in-plane needle trajectory. This rotation also allows for visualization of the pectoral branch of the thoracoacromial artery. The correct interfascial plane is confirmed by the opening of the space between the pectoralis major and pectoralis minor. The recommended volume is 0.2 mL/kg of a 0.25% bupivacaine or 0.5% ropivacaine.
The Pecs II block is performed with the patient in the same position as the Pecs I block. The first injection is identical to a Pecs I block, whereas the second injection is made at the level of the fourth rib. The transducer is placed at the midclavicular line and angled inferolaterally to visualize the axillary artery, axillary vein, and second rib. The transducer is then moved laterally until the pectoralis minor muscle, and serratus anterior muscle are identified. The transducer is then moved further laterally so the third and fourth rib can then be identified. The local anesthetic is then deposited in two separate interfascial places. The first injection of approximately 0.2 mL/kg of 0.25% bupivacaine or 0.5% ropivacaine is deposited between the pectoralis major and pectoralis minor. The needle then gets advanced using ultrasound guidance, and the second injection of 0.2 mL/kg of 0.25% bupivacaine or 0.5% ropivacaine is made between the pectoralis minor and serratus anterior. The depth is usually 1 to 3 cm for the interfascial plane between the pectoralis major and pectoralis minor, and 3 to 6 cm for the interfascial plane between the pectoralis minor and serratus anterior.
The local anesthetic for the blocks should be injected in 5 cc increments, with aspiration after each 5 cc to avoid intravascular injection. Catheters can be placed in the interfascial planes if prolonged postoperative pain is expected. Approximately 10 cm of the catheter should be advanced into the space to avoid inadvertent dislodgement of the catheter. The last 10cc can be injected through the catheter to confirm that the catheter is correctly positioned and not intravascular.
The Pecs II block is also possible by targeting the deeper interfascial plane first, injecting between the pectoralis minor and serratus anterior, then withdrawing the needle to the more superficial interfacial plane, injecting between the pectoralis major and pectoralis minor.
Complications
Complications are rare with the use of ultrasound guidance, as the pleura and major blood vessels are visible throughout the procedure.
The most common complications are pneumothorax, infection, local anesthetic toxicity/allergy, vascular puncture, and failed block.
Clinical Significance
The Pecs block is a newer regional anesthetic that can provide analgesia for chest wall surgery, potentially avoiding more invasive procedures such as paravertebral blockade. Pecs blocks have been used by anesthesiologists to provide analgesia for many procedures ranging from port placement to radical mastectomies.
Enhancing Healthcare Team Outcomes
Pecs blocks are most often performed in the preoperative period but can be placed postoperatively as well. Pecs blocks are placed by anesthesiologists, anesthesiology residents, or nurse anesthetists. A peri-operative nurse should be present throughout the procedure to assist with the procedure timeout, patient positioning, and monitoring. A proper timeout includes verifying the procedure performed, side of procedure, allergies, and any potential contraindications to performing the procedure. During the procedure, sterility is an absolute necessity. Resuscitation equipment and medication must be readily accessible in case of emergency. If using sedation, then a dedicated nurse should monitor the patient for the duration of the procedure.
Post-operatively, nursing should continue to monitor the patients and should be made aware of potential complications post-procedure, including bleeding, local anesthetic toxicity, and pneumothorax. This appraoch exemplifies the interprofessional team paradigm that is most likely to deliver positive patient results. [Level V]
Nursing, Allied Health, and Interprofessional Team Interventions
The nursing staff has a crucial role during the procedure preparation, procedure, and post-procedure monitoring. Before block placement, nursing staff should assist in the procedural timeout, which includes verifying allergies, procedure, laterality, and contraindications to the procedure. During the procedure, nursing staff should monitor the patient’s vital signs along with the level of sedation, if utilized. The nurse can assist with the patient position before and throughout the procedure. After the procedure, the nurse should watch for complications such as local anesthetic toxicity, pneumothorax, and bleeding. Nurses can also monitor the analgesia provided by the block and catheter if utilized.
Nursing, Allied Health, and Interprofessional Team Monitoring
The peri-operative nurse will monitor the patient during placement of the Pecs block. Continuous ECG, pulse oximetry, and blood pressure require monitoring during the entire peri-procedural period. If using sedation for the procedure, the peri-operative nurse can also help to monitor the patient's level of consciousness and breathing. Post-operatively, the peri-operative nurse will monitor the patient with continuous ECG, pulse oximetry, and blood pressure (at 5-minute intervals at least), but will monitor the patient's post-operative pain scores as well. If pain is severe, the anesthesiologist can give local anesthetic solution through the catheter (if catheter placed) with the local anesthetic solution as needed, or the decision can be made to give intravenous medications to manage the patient's post-operative pain.