Introduction
The external iliac artery is the major artery responsible for blood supply to the lower extremities. At the level of the inguinal ligament, the external iliac artery becomes the common femoral artery. This artery then becomes the superficial femoral artery, which at the adductor canal becomes the popliteal artery. The popliteal artery, found in the popliteal fossa, is the primary supply of blood to the distal lower extremity.
Structure and Function
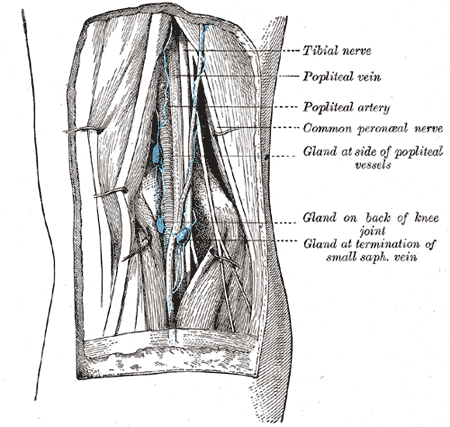
The popliteal fossa is a diamond-shaped space located posterior to the knee joint. It allows for the passage of critical neurovascular structures. These structures, from medial to lateral, are the popliteal artery, popliteal vein, tibial nerve, and common peroneal nerve. The tibial nerve inverts and plantarflexes the foot, while the common peroneal nerve everts and dorsiflexes the foot. The tibial nerve provides sensation to the sole, while the common peroneal nerve provides sensation to the dorsum of the foot. The popliteal fossa has four major borders. The superomedial border is formed by the semimembranosus muscle, the superolateral border is formed by the biceps femoris muscle, the inferomedial border is formed by the medial head of the gastrocnemius muscle, and the inferolateral border is formed by the lateral head of the gastrocnemius muscle and the plantaris muscle.
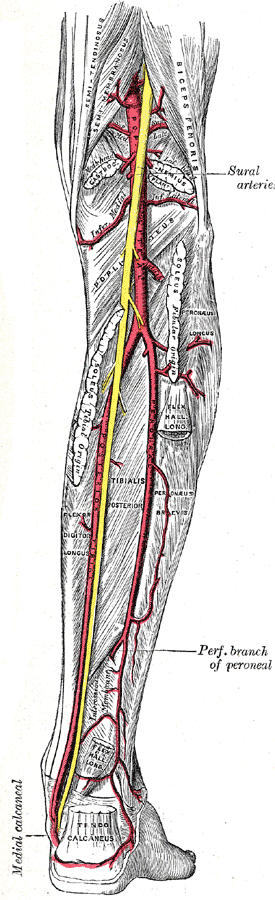
The popliteal artery is a continuation of the superficial femoral artery as it passes through the adductor hiatus of the adductor magnus muscle, traveling posteriorly to the knee and anterior to its accompanying vein, the popliteal vein, until it bifurcates into the anterior tibial artery and the common trunk of the posterior tibial and peroneal arteries. Geniculate arteries branch at multiple levels of the knee to provide blood to the structures of the knee and contribute to collateral blood flow of the lower extremity.
The popliteal artery provides numerous branches of blood supply to the structures of the knee and the lower extremity. Originating from above the knee joint are the superior medial and superior lateral genicular arteries with connections to the deep femoral artery providing collateral blood flow proximal to the knee. At the level of the knee joint is the middle genicular artery and sural arteries. Below the knee joint are the inferior medial and inferior lateral genicular arteries with connections to the tibial arteries, providing additional collateral blood flow distal to the knee. The four geniculate arteries anastomose anteriorly around the knee and patella.
The popliteal artery also provides blood directly to numerous muscles including the soleus, gastrocnemius, plantaris, and distal portions of the hamstring muscles.
Blood Supply
- Superior geniculate arteries - the knee joint, distal femur, and muscles of the medial and lateral knee
- Sural arteries – structures within the popliteal fossa and gastrocnemius, soleus, and plantaris muscles
- Middle genicular artery – cruciate ligaments and synovial membrane of the knee
- Inferior geniculate arteries – knee joint, muscles of the medial and lateral knee, and proximal tibia
Embryology
The vascular system derives from the mesoderm after about 17 days of gestation. The popliteal artery develops in part with the very complicated development of the lower extremity limb bud early in fetal development.
Blood Supply and Lymphatics
The popliteal artery is the primary vascular supply in the region of the knee and lower leg.
The popliteal vein runs posterior to the popliteal artery and receives blood from multiple tributaries.
- Genicular veins
- Sural veins
- Small saphenous vein
- Anterior tibial vein
- Posterior tibial vein
- Peroneal veins
Popliteal lymph nodes can be found throughout the popliteal fossa, closely associated with the popliteal vessels. These nodes drain into the deep inguinal lymph nodes.[1]
Nerves
The regulation of the function of the popliteal artery is via a proper balance between the sympathetic and parasympathetic fibers.
The integration of afferent information from the popliteal artery (shear stress, compression from external tissues, stretching, etc.) undergoes interpretation in the central nervous system, which collaborates the autonomic system to manage the arterial function.
Muscles
Muscle aerobic activity improves the function of the popliteal artery: its endothelium, its ramifications, its elasticity, and its ability to transport oxygen and nutrients useful to the target tissues.
The popliteal artery provides blood supply to the soleus, gastrocnemius, plantaris, and distal portions of the hamstring muscles.
Physiologic Variants
Physiological variants of the popliteal artery are a common phenomenon. Studies have shown seven major branching variants using digital subtraction angiography. A particular study from 2004 to 2006 on 621 patients (1242 limbs) revealed 89.2% of participants with traditional branching patterns of the popliteal artery and the following variations:[2]
- Aplastic/hypoplastic posterior tibial artery-5.1%
- Hypoplastic/aplastic anterior tibial artery-1.7%
- Trifurcation-1.5%
- High origin of the anterior tibial artery-1.2%
- Hypoplastic/aplastic posterior tibial and anterior tibial arteries-0.8%
- High origin of the posterior tibial branch-0.4%
- Anterior tibioperoneal trunk-0.1%
Research found that when one limb had a variant, there was a 28% chance the other limb would also be a variant. When one limb displayed traditional anatomy, there was a 13% chance the other limb would contain a variation. These variations carry significance in surgical situations.[2]
Surgical Considerations
A posterior surgical approach to the knee is utilized in several situations. Knowledge of anatomy and the possible variations of the popliteal artery and its branches is vital in preserving blood flow to the knee and lower leg.[1]
A recent meta-analysis study (14 research studies) demonstrated how endovascular popliteal artery aneurysm repair is a procedure without significant complications and with a relatively short length of hospital stay.[3]
Another recent 5-year study showed that popliteal artery surgery in case of entrapment is satisfactory from a clinical and functional point of view.
Clinical Significance
Popliteal pulse – the popliteal pulse is palpable in the popliteal fossa with the knee in moderate flexion. It is important for the evaluation of perfusion to the lower leg in the event the dorsalis pedis and posterior tibial arteries are non-palpable, such as in a person with advanced peripheral artery disease.[1]
Popliteal aneurysms – May occur in isolation, bilaterally (50% of cases), or in conjunction with other large vessel aneurysms (abdominal aortic aneurysm seen in 30-50% of cases). Popliteal aneurysms are almost always true aneurysms involving all three layers of the vessel (intima, media, and adventitia) and are fusiform. Risk factors for developing aneurysms of the popliteal artery include smoking, hypertension, male sex, age, and arteriomegaly. Patients will often present with leg pain or a palpable pulsatile mass at the level of or above the knee posteriorly. Thrombus formation can result in reduced blood flow.[4] Symptoms of popliteal aneurysms include:
- Chronic ischemia with varying degrees of lower extremity claudication.
- Acute ischemia secondary to the formation of a thrombus occluding blood flow to the distal lower extremity, this is a vascular emergency.
- Local compression of nerves resulting in motor and sensory deficits. Compression of the popliteal vein leading to swelling of the distal lower extremity secondary to compromised blood return.
- Rupture of a popliteal artery aneurysm is rare and typically confines itself to the popliteal fossa resulting in severe pain behind the knee. Rupture into the popliteal vein has been described resulting in an arteriovenous fistula. This is a vascular emergency.
Diagnostic confirmation is with noninvasive radiographic imaging using duplex ultrasound, CT angiography, or MR angiography. CT and MR angiography are the most accurate tools in the diagnosis and confirm an aneurysm with a measured lumen = 1.5 cm. Conservative management may be a consideration for aneurysms that are asymptomatic and less than 2 cm. Intervention is typically the recommendation when an aneurysm is greater than 2 cm or when symptoms indicating thrombus formation or ischemia are present.[1] Placement of a stent may prevent further dilation.[5] In some cases, a venous graft may be used to replace the damaged artery.[6]
Hemorrhage/trauma – As the popliteal artery descends below the knee it is held tightly against the bone by the arch of the soleus muscle. The tight hold distally does not allow for much movement in the event of trauma involving the knee. Reports are that between 4% and 20% of knee dislocations result in a rupture of the popliteal artery; the vascular compromise is a surgical emergency. When addressing a knee dislocation ischemia should always be suspected. Distal pulses should be evaluated before and immediately after the reduction of the knee. The absence of a pulse should warrant angiography. A ruptured vessel requires a bypass of the disrupted segment using an inverted portion of the saphenous vein.[7]
Popliteal artery entrapment syndrome (PAES) - A rare vascular disease that compromises blood flow to the distal lower extremity of young athletes, particularly women. Hypertrophy of the gastrocnemius muscle or popliteus muscle results in compressive forces that reduce blood flow through the artery. Patients will present with pain, numbness, and cramping of the calf and lower extremity with exercise. Pain typically resolves with a few minutes of rest.[8] Surgical intervention and the use of botulinum toxin injections have sparked a discussion for the treatment of more severe cases.[9][10]
Cystic adventitial disease – A rare vascular condition that typically presents with claudication in healthy individuals that do not have significant risk factors of peripheral artery disease. Cystic adventitial disease is a result of cyst formation within the artery that narrows the lumen and restricts blood flow. Cyst formation is not limited to the popliteal artery but is the most common site to form and produce symptoms. Early treatment reduces the risk of thrombosis. Treatment is the removal of the cyst and replacing the affected segment with venous graft.[11]
Popliteal cyst - Also known as Baker's cyst. This is a fluid-filled swelling that forms on the posterior aspect of the knee. It is common in patients with osteoarthritis or rheumatoid arthritis. It presents with a bulge behind the knee joint that causes stiffness and resistance to flexion of the knee. It can occasionally lead to compression of the popliteal artery.
Other Issues
Entrapment of the popliteal artery could present itself subtly, for example, as a Raynaud phenomenon.