Introduction
While the term “motor neuron” evokes the idea that there is only one type of neuron that conducts movement, this is far from the truth. In fact, within the classification of a “motor neuron,” there lies both upper and lower motor neurons, which are entirely different in terms of their origins, synapse points, pathways, neurotransmitters, and lesion characteristics. Overall, motor neurons (or motoneurons) comprise various tightly controlled, complex circuits throughout the body that allows for both voluntary and involuntary movements through the innervation of effector muscles and glands. The upper and lower motor neurons form a two-neuron circuit. The upper motor neurons originate in the cerebral cortex and travel down to the brain stem or spinal cord, while the lower motor neurons begin in the spinal cord and go on to innervate muscles and glands throughout the body. Understanding the difference between upper and lower motor neurons, as well as the pathway that they take, is crucial to being able to not only diagnose these neuronal injuries but also localize the lesions efficiently.
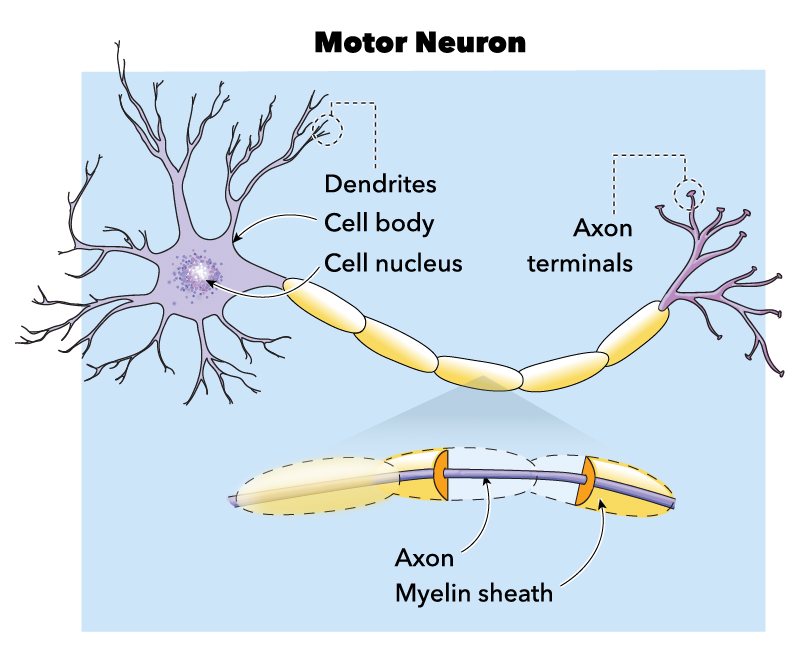
Structure and Function
The upper and lower motor neurons together comprise a two-neuron pathway that is responsible for movement. Upper and lower motor neurons utilize different neurotransmitters to relay their signals. Upper motor neurons use glutamate, while lower motor neurons use acetylcholine.[1]
To perform a movement, a signal must begin in the primary motor cortex of the brain, which is in the precentral gyrus. In the primary motor cortex are the cell bodies of the upper motor neurons, referred to as Betz cells.[2] Specifically, these cells are located in layer 5 of the motor cortex and have long apical dendrites that branch up into layer 1.[3] The upper motor neuron is responsible for integrating all of the excitatory and inhibitory signals from the cortex and translating it into a signal that will initiate or inhibit voluntary movement. Thalamocortical neurons and callosal projection neurons regulate upper motor neurons. While the mechanism of regulation by these entities is not completely understood, it is thought that the majority of the excitatory input to these neurons comes from neurons located in layers 2, 3, and 5 of the motor cortex. The axons of the upper motor neuron travel down through the posterior limb of the internal capsule. From there, they continue through the cerebral peduncles in the midbrain, longitudinal pontine fibers, and eventually the medullary pyramids. It is at this location that the majority (approximately 90%) of the fibers will decussate and continue down the spinal cord on the contralateral side of the body as the lateral corticospinal tract. The lateral corticospinal tract is the largest descending pathway and is located in the lateral funiculus. This tract will synapse directly onto the lower motor neuron in the anterior horn of the spinal cord. The pyramidal tract fibers that did not decussate at the medulla comprise the anterior corticospinal tract, which is much smaller than the lateral corticospinal tract. This tract is located near the anterior median fissure and is responsible for axial and proximal limb movement and control, which helps with posture. Although it does not decussate at in the medulla, this tract does decussate at the spinal level being innervated.[4][5][6]
The lower motor neuron is responsible for transmitting the signal from the upper motor neuron to the effector muscle to perform a movement. There are three broad types of lower motor neurons: somatic motor neurons, special visceral efferent (branchial) motor neurons, and general visceral motor neurons.[1]
Somatic motor neurons are in the brainstem and further divide into three categories: alpha, beta, and gamma. Alpha motor neurons innervate extrafusal muscle fibers and are the primary means of skeletal muscle contraction. The large alpha motor neuron cell body can be either in the brainstem or spinal cord. In the spinal cord, the cell bodies are found in the anterior horn and thus are called anterior horn cells. From the anterior horn cell, a single axon goes on to innervate many muscle fibers within a single muscle. The properties of these muscle fibers are nearly identical, allowing for controlled, synchronous movement of the motor unit upon depolarization of the lower motor neuron. Beta motor neurons are poorly characterized, but it has been established that they innervate both extrafusal and intrafusal fibers. Gamma motor neurons innervate muscle spindles and dictate their sensitivity. These neurons primarily respond to stretch of the muscle spindle. Despite being named a “motor neuron,” these neurons do not directly cause any motor function. It is thought that they get activated along with alpha motor neurons and fine-tune the muscle contraction (alpha-gamma coactivation). A disruption in either alpha or gamma motor neurons will result in a disruption of muscle tone.[7][1]
Lower motor neurons also play a role in the somatic reflex arc. When muscle spindles detect a sudden stretch, a signal travels down the afferent nerve fibers. These nerve fibers synapse either directly onto the alpha motor neuron (monosynaptic reflex arc), or onto interneurons, which then synapse onto the alpha motor neuron (polysynaptic reflex arc). The lower motor neuron innervates the effector muscle, allowing for a quick muscle response. A reflex arc allows for interpretation of and reaction on the stimulus immediately through the spinal cord, bypassing the brain, resulting in a faster effector response.[1][8]
Branchial motor neurons innervate the muscles of the head and neck that derive from the branchial arches. They are in the brainstem. The branchial motor neurons and sensory neurons together form the nuclei of cranial nerves V, VII, IX, X, and XI.[1]
Visceral motor neurons contribute to both the sympathetic and parasympathetic functions of the autonomic nervous system. In the sympathetic nervous system, central motor neurons are present in the spinal cord from T1-L2. They appear in the intermediolateral (IML) nucleus. Motor neurons from this nucleus have three different pathways. The first two pathways are to the prevertebral and paravertebral ganglia, from which peripheral neurons go on to innervate the heart, colon, intestines, kidneys, and lungs. The third possible pathway in this system is to the catecholamine-producing chromaffin cells of the adrenal medulla. By targeting these three pathways, the visceral motor neurons in the sympathetic division contribute to the “fight-or-flight” response. On the other hand, in the parasympathetic system, the visceral motor neurons help give rise to cranial nerves III, VII, IX, and X. Besides in the brainstem, these visceral motor neurons contribute to the parasympathetic system in the spinal cord at levels S2-S4. Similarly to the sympathetic division, these motor neurons directly innervate ganglia in the heart, pancreas, lungs, and kidneys. Thus, in both divisions of the autonomic system, these lower motor neurons take on a different role than somatic motor neurons in that they do not directly innervate an effector muscle, and instead innervate ganglia.[1]
Blood Supply and Lymphatics
The primary motor cortex is supplied primarily by the middle cerebral artery (MCA), along with the anterior cerebral artery (ACA). The MCA supplies the area of the primary motor cortex that is responsible for the upper limbs and face, while the ACA supplies blood to the area that controls the lower limbs. As previously discussed, the upper motor neurons continue down as the pyramidal tract, which receives vascular supply from the lenticulostriate arteries. Once this tract reaches the brainstem, the paramedian branches of the basilar artery become the primary source of blood. At the caudal medulla level, the anterior spinal artery supplies most of the blood. This artery continues to provide blood to the lateral and anterior corticospinal tracts and anterior horn cells in the spinal cord.[9]
Surgical Considerations
Because there are numerous causes of upper and lower motor neuron dysfunction and injury, surgical consideration requires individualization for each patient. The overall goal of any form of treatment, surgical or not, should be focused on reducing pain and preserving or enhancing day-to-day functionality.[10]
Surgical intervention may also help prevent upper extremity deformity due to contractures or spasticity that may present with an upper motor neuron injury. Examples of surgical procedures that are options for a patient with severe upper motor neuron disease include tendon lengthening, muscle origin release, myotomy, tenotomy, neurectomy, arthrodesis, and joint osteocapsular release. Surgical interventions are chosen based on an individual patient’s level of functioning.[10]
Clinical Significance
Upper and lower motor neuron lesions cause very different clinical findings. An upper motor neuron lesion is a lesion anywhere from the cortex to the corticospinal tract. This lesion causes hyperreflexia, spasticity, and a positive Babinski reflex, presenting as an upward response of the big toe when the plantar surface of the foot is stroked, with other toes fanning out. On the other hand, lower motor neuron lesions are lesions anywhere from the anterior horn of the spinal cord, peripheral nerve, neuromuscular junction, or muscle. This type of lesion causes hyporeflexia, flaccid paralysis, and atrophy.
Knowledge of the anatomy of the motor neurons is critical to the ability to localize the lesion when faced with a patient who presents with a weakness that is likely due to a motor neuron injury. Focusing mainly on the lateral corticospinal tract, it is essential to keep in mind that this neuronal pathway decussates at the level of the pyramids in the medulla. This crossing means that an upper motor neuron lesion above the medulla will cause symptoms on the contralateral side of the body. However, a lesion to the lateral corticospinal tract after it decussates will present on the ipsilateral side of the body.
Upper motor neuron syndrome occurs when there is injury anywhere to the descending tract before the anterior horn of the spinal cord (cortex, internal capsule, pyramidal tract, lateral corticospinal tract). Examples of pathology that cause upper motor neuron symptoms are strokes, traumatic brain injury, spinal cord injury, amyotrophic lateral sclerosis (ALS), primary lateral sclerosis (PLS), multiple sclerosis (MS), or anoxic brain injury. There are both positive and negative features of the upper motor neuron syndrome. Positive features include hyperreflexia (abnormally brisk reflexes), spasticity (a brisk stretch of muscles causes a sudden increase in tone followed by decreased muscle resistance), and a positive Babinski reflex. Negative features include impaired motor control, easy fatiguability, weakness, and loss of dexterity.[11][5][10]
Lower motor neuron syndrome occurs when there is an injury to the anterior horn cells or the peripheral nerve. Diseases of the neuromuscular junction or muscle itself may mimic a lower motor neuron lesion and are important to consider in the differential diagnosis. Similarly to an upper motor neuron lesion, the patient with a lower motor neuron lesion will present with weakness; however, distinct lower motor neuron lesion findings will include hyporeflexia, flaccid paralysis, fasciculations, and atrophy.
There are many forms of motor neuron disease, the most common of which is amyotrophic lateral sclerosis (ALS). This disease is unique in that it presents with both upper and motor neuron signs. The patient will typically present with weakness, along with spastic paralysis and hyperreflexia in the lower limbs and flaccid paralysis and hyporeflexia in the upper limbs. The patient may also present with fasciculations in both the tongue and extremities. Of note, there is no sensory loss. ALS is a progressive neurogenerative disease, and eventually, the patient will have serious dysarthria, dysphagia, extreme weakness, and dyspnea. The estimated median survival is 2 to 4 years, with the most common cause of death being respiratory failure.[12]
One group of genetic disorders that causes lower motor neuron disease is spinal muscular atrophy (SMA). There are many different forms of SMA, but all of them are characterized by degeneration of the motor nuclei in the brainstem, in addition to the anterior horn cells found in the spinal cord. One specific type of SMA is spinobulbar muscular atrophy (Kennedy disease). This x-linked disease usually presents in adulthood (age 30 to 50). First presenting signs typically include tremor, lower extremity weakness, and orolingual fasciculations. This pathology is a progressive disease that is later characterized by the above symptoms in addition to atrophy of limb, bulbar, and facial muscles.[13]
Poliomyelitis is another lower motor neuron disease. This disease results from poliovirus and results in the destruction of the anterior horn cells. Subsequently, the affected patient will experience weakness and lower motor neuron symptoms, including flaccid paralysis in the lower limbs. Usually, this presents asymmetrically. The patient may also provide a history of muscle aches or muscle spasm that occurred in the recent past. Unfortunately, this weakness and paralysis may extend up to involve the respiratory muscles. Many patients will recover some strength, but may later decompensate into “postpolio syndrome,” which is characterized by the onset of additional weakness, pain, and/or atrophy. Among other viral causes of anterior horn cell destruction are coxsackievirus, West Nile virus, and echovirus.[13]
While most cranial nerves are innervated by upper motor neurons bilaterally, cranial nerves VII and XII are the exceptions, as they receive only unilateral input from the contralateral side of the brain. Specifically, damage to the corticobulbar tract and/or facial nerve causes a unique presentation depending on whether the damage occurred in the upper vs. lower motor neuron. The forehead region is dually innervated by corticobulbar tracts from each side of the brain, while the rest of the face below the forehead is innervated primarily by the lower motor neuron of CN VII. An upper motor neuron lesion of the facial nerve can occur anywhere in the corticobulbar tract rostral to the facial motor nucleus on the pons. If an upper motor neuron lesion occurs, the forehead will be spared due to its dual innervation. However, a lower motor neuron lesion of CN VII results in flaccid paralysis of the entire ipsilateral side of the face.[14]
Overall, clinicians should consider motor neuron disease whenever a patient presents with weakness and any of the previously described motor neuron lesion signs without significant sensory loss. Referral to a neurologist for subsequent testing is warranted in these cases.