Introduction
Introduction
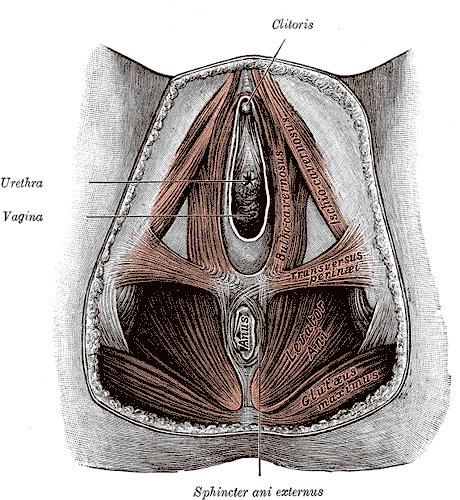
The perineal body (PB), also referred to as the central tendon of the perineum, is a fibro-muscular structure located in the midline of the perineum. Its exact location is the midline of the perineum at the junction of the anus and urogenital triangle in both females and males. In males, it is located between the anus and bulb of the penis, whereas in females it is found between the anus and the posterior limit of the vulvar orifice. The perineal body helps strengthen the pelvic floor. It provides attachments to the following muscles[1]:
- The bulbospongiosus muscle (striated muscle) adheres anterolaterally to the PB.
- Deep transverse perineal muscle (male) adheres laterally to the PB.
- Compressor urethra muscle (female) adheres anteriorly to the PB.
- The external anal sphincter muscle adheres posterolaterally to the PB.
- The internal anal sphincter muscle intermingles with LAM and adheres posteriorly to the PB.
- The external urethral sphincter muscle adheres anteriorly to the PB.
- Levator anis muscle (the internal fibers of the puborectalis muscle) adheres laterally to the PB along its whole vertical length.
- The recto-urethralis muscle (perineal smooth muscle) runs from the LAM laterally to the bulbourethral glands adheres anterolaterally to the puborectalis muscle.
- The longitudinal anis muscle (LAM) strongly adheres anteriorly and anterolaterally to the PB and puborectalis muscle.
Two fascial structures join to the perineal body[2]:
- The superficial perineal fascia, the perineal membrane joins the PB anteriorly.
- The rectovaginal septum (female) joins the PB superiorly.
- The recto prostatic septum (male) joins the PB superiorly.
The perineal body is critical for maintaining the integrity of the pelvic floor, especially in females.
The perineal body may rupture during vaginal delivery. Once this occurs, it leads to a widening of the gap between the free borders of the levator ani muscles on both sides. This widening gap predisposes women to prolapse of the rectum, uterus, and sometimes the urinary bladder. It is also involved in the surgical procedure for anorectal tumors to achieve a tumor-free circumferential resection margin for reducing the risk of local recurrence.