Introduction
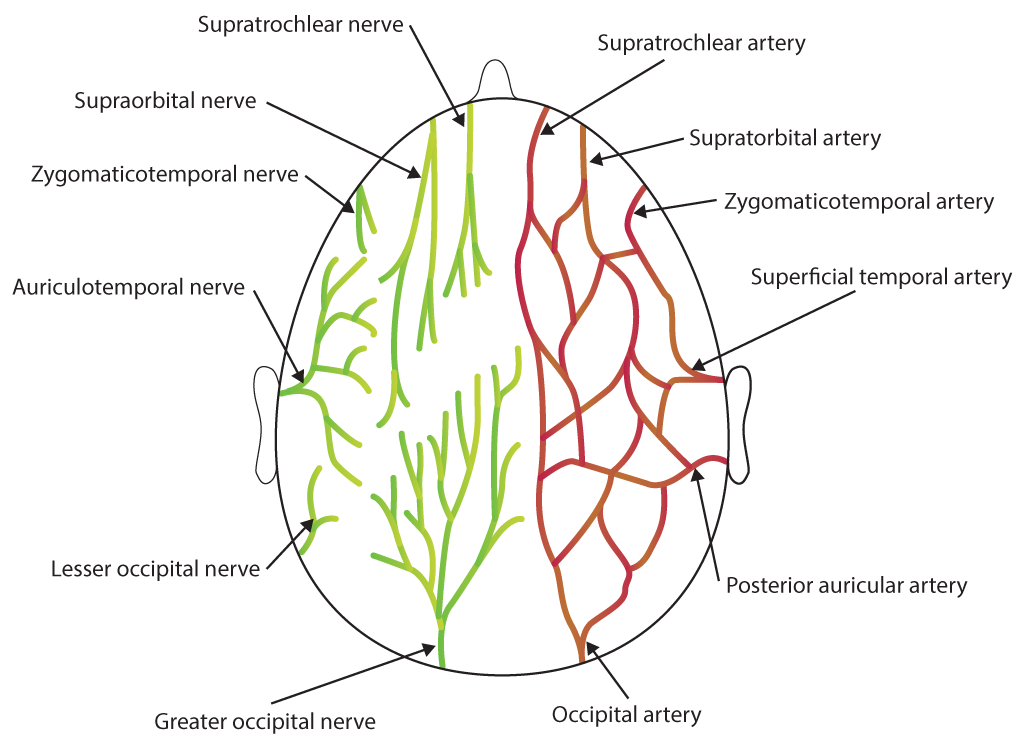
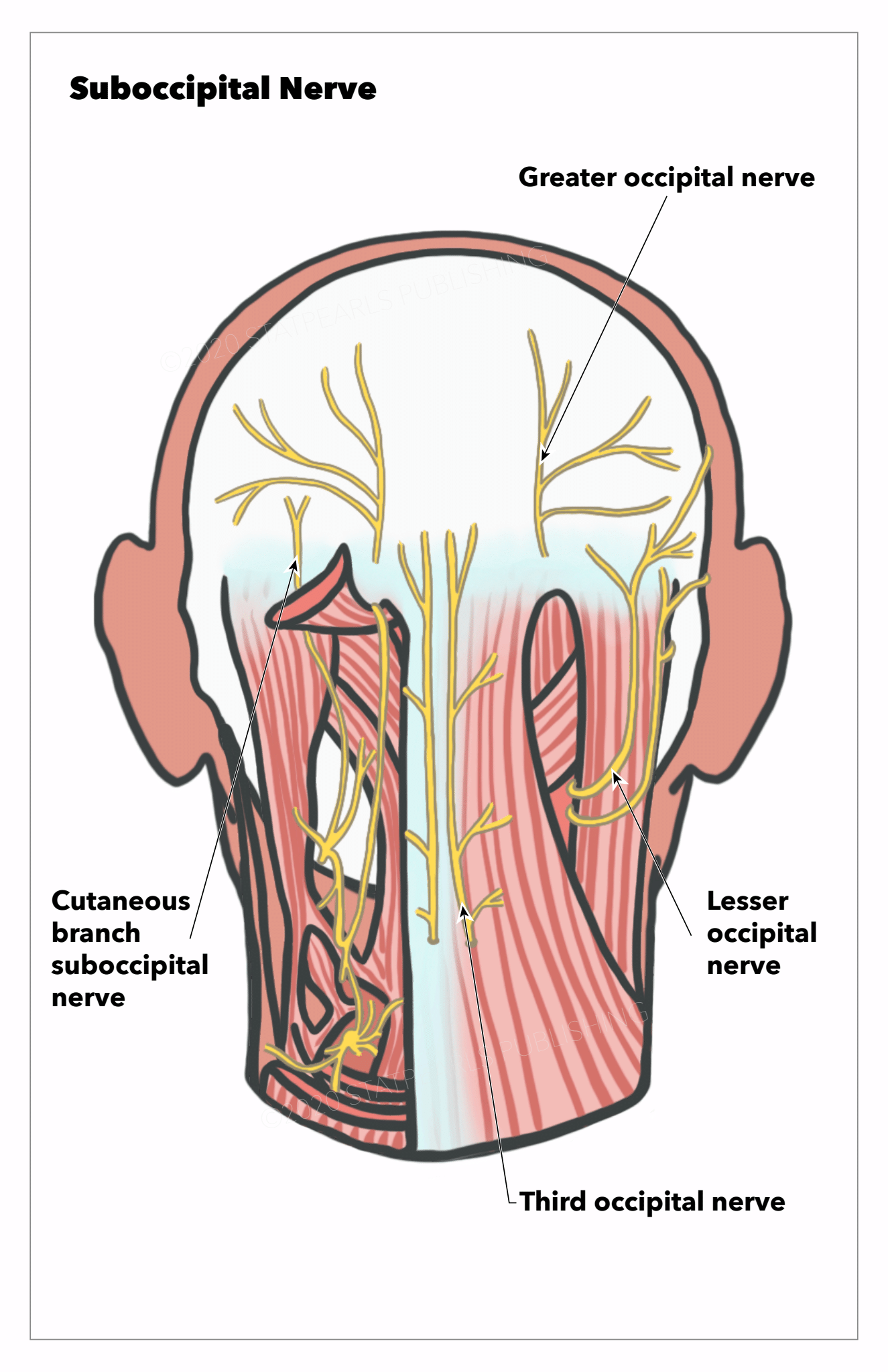
The occipital nerves are a group of nerves that arise from the C2 and C3 spinal nerves.[1][2] They innervate the posterior scalp up as far as the vertex and other structures as well, such as the ear.[2] There are three major occipital nerves in the human body: the greater occipital nerve (GON), the lesser (or small) occipital nerve (LON), and the third (or least) occipital nerve (TON).
Structure and Function
Greater Occipital Nerve
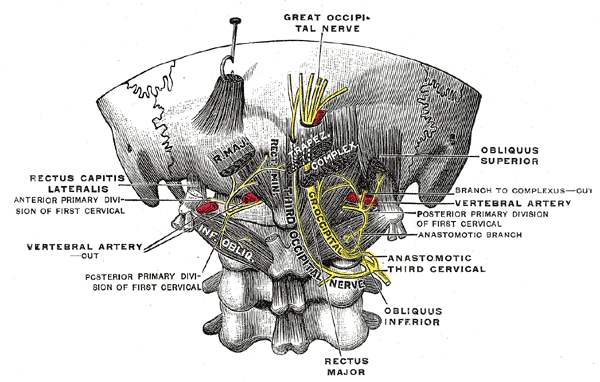
The GON is the biggest purely afferent nerve that arises from the medial division of the dorsal ramus of the C2 spinal nerve. It runs backward between the C1 and C2 vertebrae and traverses between the inferior capitis oblique and semispinalis capitis muscles from underneath the suboccipital triangle.[2] Rarely does the GON travel within the inferior oblique. While traveling to the subcutaneous layer, the GON is found to pierce the semispinalis capitis muscle in most cases, and in some cases, the trapezius and the inferior oblique.[1] This complex involvement with the nearby musculature may make the GON a potential source of nerve compression, entrapment, or irritation. The GON then perforates the aponeurotic fibrous layer of the trapezius and the sternocleidomastoid to travel to the scalp and the superior nuchal line.[2] The GON also traverses along the occipital artery after passing through the semispinalis capitis. The GON innervates the skin of the back of the scalp up to the vertex of the skull, the ear, and the skin just above the parotid gland.[2]
Lesser Occipital Nerve
The LON originates from the ventral rami of the C2 and C3 spinal nerves and goes to the occipital region along the posterior margin of the sternocleidomastoid muscle.[2] It pierces the deep cervical fascia close to the cranium and travels upward. Near the cranium, it penetrates the deep cervical fascia and goes superiorly above the occiput to innervate the skin and communicate with the GON. [1] The LON has three branches: the auricular, mastoid, and occipital branches. The LON divides into medial and lateral segments between the inion and intermastoid line.[3] The LON innervates the scalp in the lateral region of the head behind the ear and the cranial surface of the ear.[1]
Third Occipital Nerve
The TON is a superficial medial branch of the dorsal ramus of the C3 spinal nerve and is thicker compared to other medial branches.[1] The dorsal ramus of the C3 spinal nerve divides into lateral and medial branches. The medial division further divides into superficial and deep branches, of which the superficial division is named the TON. The TON travels through the dorsolateral surface of the C2-C3 facet joint.[1] Based on a study by Tubbs et al., the TON was found to send out small branches that travel across the midline and interact with the contralateral TON in 66.7% of patients.[4] The TON also perforates the splenius capitis, trapezius, and semispinalis capitis. It then communicates with the GON and innervates the region of the skin below the superior nuchal line after innervating the semispinalis capitis. The TON also innervates the facet joint between the C2 and C3 spinal nerves and a portion of the semispinalis capitis.[2]
Blood Supply and Lymphatics
The scalp is highly vascularized and is characterized by having many arterial anastomoses. Most of the blood supply comes from the external carotid arteries.[2] Regarding the occipital region of the scalp, the vascularization is via the occipital artery and the posterior auricular arteries.[5] Within the auriculomastoid sulcus, the posterior auricular artery travels superficially and separates into three branches: the mastoid, auricular, and transverse nuchal arteries.[5] The LON is found to be close to the occipital artery. According to Kemp et al., the LON was found to be situated 2.5cm lateral to the occipital artery above the occiput.[2] Also, according to Lee et al., who studied the topography of the LON in 20 sides of 10 heads from fresh cadavers, branches from the occipital artery communicated with the LON in 55% of samples.[6] Among these samples, 45% of samples had the occipital artery crossing the LON at a single location while 10% of samples had the occipital artery communicating with the LON via a helical intertwining relationship. The researchers also found a fascial band as a compression point in 20% of samples.[6]
The GON is also closely associated with the occipital artery. After the GON perforates the semispinalis capitis, it travels with the occipital artery that is medial to the nerve.[2] The GON may have a much more intimate relationship than previously thought. According to a study conducted by Janis et al., in which the researchers analyzed the topographic relationship between the GON and occipital artery in fifty samples of 25 posterior necks and scalps from cadavers, the GON, and occipital artery were found to cross each other in 54% of samples.[7] Among samples where there was an intersection between the GON and the occipital artery, these crossings could differ from intersecting each other at a single point (29.6%) to intertwining in a helical fashion (70.4%). These crossings were usually discovered in the tunnel of the trapezius caudal to the occipital protuberance but were also present above the occipitalis.[7] These findings may be useful for migraine patients, as many of these patients report having pulsatile symptoms, and their headaches may contain a vascular component. Many researchers have proposed that the intersections between the GON and occipital artery may be responsible for these symptoms.[7] Furthermore, another study by Shimizu et al. discovered the occipital artery and GON intersected in the nuchal subcutaneous layer, and the GON was always more superficial to the occipital artery at the point of intersection.[8] They postulated the intimate relationship between the GON and occipital artery might be a contributing factor for occipital neuralgia (ON).[8]
Nerves
As mentioned previously, the GON arises from the medial branch of the dorsal ramus of the C2 spinal nerve and innervates the skin of the back of the scalp up to the vertex of the skull, the ear, and the skin just above the parotid gland.[2] When the GON is over the occiput, it communicates with the LON laterally and the TON. The LON comes from the ventral rami of the C2 and C3 spinal nerves and provides innervation to the scalp in the lateral region of the head behind the ear.[2] The LON also transmits a branch to the GON as it goes above the occiput near the cranium.[2] It also communicates with the mastoid division of the greater auricular nerve. The TON originates from the medial branch of the dorsal ramus of the C3 spinal nerve and innervates the facet joint between the C2 and C3 spinal nerves and a portion of the semispinalis capitis.[2] Its cutaneous division also innervates the skin below the occiput. The TON also communicates with the GON and innervates the region of the skin below the superior nuchal line.[2]
Muscles
Greater Occipital Nerve
As stated previously, the GON traverses between the inferior capitis oblique and semispinalis capitis muscles from underneath the suboccipital triangle.[2] Rarely does the GON travel within the inferior oblique. While traveling to the subcutaneous layer, the GON is found to pierce the semispinalis capitis muscle in most cases, and in some cases, the trapezius and the inferior oblique.[1] For the treatment of GON entrapment neuropathy, the regions where the GON traverses between the atlas and the axis, the GON courses between the obliquus capitis inferior and semispinalis capitis, or the GON perforates the semispinalis capitis and the trapezius, which are potential areas of GON irritation and entrapment.[9] These zones could be affected by other medical issues, such as whiplash injuries and posture imbalances, and could serve as possible origins of ON.[9] However, the GON has many physiological variants, which will be a topic in the following section.
Lesser Occipital Nerve
Regarding the LON, the area where the LON traverses from behind the sternocleidomastoid, the area where the LON ascends along the posterior margin of the sternocleidomastoid, and the area where the LON intersects with the nuchal line have been found to serve as potential compression points.[10] This article will cover the physiological variants of the LON in the following section.
Physiologic Variants
Greater Occipital Nerve
As stated previously, for the GON, the region where it traverses between the atlas and the axis, the area where it courses between the obliquus capitis inferior and semispinalis capitis, or the area where it perforates the semispinalis capitis and the trapezius are potential areas of GON irritation and entrapment and could likely lead to occipital neuralgia.[9] However, many studies had different results regarding the prevalence and descriptions of these locations. For instance, in 20 autopsy cases, Bovim et al. discovered the GON perforated the trapezius in 45% of samples, the semispinalis capitis in 90% of samples, and the inferior oblique in 7.5% of samples.[11] They also stated the GON did not pass through the trapezius in all cases but appeared from an opening above the aponeurotic fibrous layer of the trapezius and the sternocleidomastoid.[11] In another study by Ducic et al., among 125 individuals, the GON passed through the semispinalis capitis muscle in 98.5% of cases.[12] The rest of the cases were divided by semispinalis capitis fibers or were within the trapezius. The nerves were also found to be asymmetric on both sides in 43.9% of individuals.[12]
In another study by Tubbs et al., among samples from 12 adult cadavers, the GON perforated the trapezius in 16.7% of cases and the aponeurosis in 83.3% of cases. In another study by Junewicz et al., among 272 patients who had GON decompression surgery, the GON was discovered to perforate the semispinalis in all patients bilaterally.[3] About 7.4% of patients had multiple branches of the GON, and 3.7% of subjects had blood vessels or muscles within these branches.[3] Finally, in a study by Won et al., among 56 specimens from cadavers, 62.5% of the samples had the GON perforating the fascia between the trapezius and the sternocleidomastoid while 37.5% of the samples had the GON passing through the trapezius.[9] These anatomic variations should be noted by physicians to understand better the topography of the GON and the nearby vasculature.
Lesser Occipital Nerve
Concerning the LON, it was mainly found to be at the posterior margin of the sternocleidomastoid muscle. However, reports exist showing some anatomic variations of the LON. For instance, Madhavi et al. reported a case of bilateral triplication of the LON in an adult cadaver.[13] One of the LONs originated from a nerve close to the trapezius that came from the supraclavicular nerve. Another LON traversed through the posterior triangle and the trapezius and innervated the neck, auricle, and posterior area of the scalp.[13] The authors concluded these findings might be relevant to patients with cervicogenic headaches because some of these patients may experience pain from neck movement.[13] Previous studies also reported duplication of the LON. There are also reports of the LON passing through the occipital region of the posterior triangle, even though this phenomenon was rare.[14] Also, as mentioned previously, Lee et al. reported, among samples where branches from the occipital artery contacted the LON, 45% of samples had the occipital artery crossing the LON at a single location while 10% of samples had the occipital artery communicating with the LON via a helical intertwining relationship.[6] A fascial band also appeared as a compression point in 20% of samples.[6] Peled et al. also reported similar results. However, they also noted a lot of variation regarding the branching of the LON.[10] Physicians should consider these results to ensure patients who receive surgical treatment of the LON receive maximum benefit.
Surgical Considerations
The GON, LON, and TON are commonly associated with occipital neuralgia, cervicogenic headaches, and migraine headaches.[1] Occipital neuralgia is a type of headache characterized by a paroxysmal stabbing pain in the posterior area of the scalp.[1] Although there is a wide range of treatment options for occipital neuralgia, there is currently no consensus among medical practitioners about which method is superior. Occipital nerve block, pulsed or thermal radiofrequency ablation, and transcutaneous electrical nerve stimulation are minimally invasive treatments used to treat occipital neuralgia, migraines, cluster headache, and associated features cervicogenic headaches.[2] Other surgical treatments used to treat this disease include dorsal rhizotomy, occipital neurectomy, and microvascular decompression.[2] A review of these treatments follows.
Occipital Nerve Block
GON blocks are frequently used to treat migraine headaches and occipital neuralgia. A small dose of local anesthetic combined with corticosteroids is injected halfway on the nuchal line between the occipital protuberance and the mastoid process and above the occipital ridge.[1] The occipital artery is the most reliable anatomical landmark because the nerve appears to be in line with this artery. To increase the chances that the surgery will be successful, the potential areas for GON, LON, and TON entrapment and compression, as previously mentioned, must be considered.[2] For GON blocks, among 562 patients with migraines who had GON blocks, Allen et al. reported 58% of patients had reduced their baseline pain scores by more than 50%, and these results were consistent regardless of age, prior treatments, or sex.[15] In another study conducted by Juskys et al., among 44 patients with occipital neuralgia who received treatment with an occipital nerve block, 95.45% of patients were comfortable with the pain for at least six months, and only 16.67% of patients needed analgesics to cope with the pain after six months.[16] Although controlled, blinded studies are limited, and there is currently no standardization of the procedure, nerve blocks, particularly GON blocks, have demonstrated effectiveness in treating migraines and ON.
Pulsed Radiofrequency (PRF) or Thermal Radiofrequency Ablation (TRFA)
Regarding the GON, LON, and TON, PRF may decrease pain by generating a low-intensity electrical field around sensory nerves that hinder the operation of the A-delta and C fibers in the long run.[1] However, the reports published concerning PRF treatment of occipital neuralgia were small, observational cohort studies or case reports. For instance, Kim et al. reported their successful attempts at performing ultrasound-guided PRF on two male patients with headaches in the occipital region.[17] In another study conducted by Cohen et al., among 81 patients with occipital neuralgia who either received PRF or local anesthetic, the PRF group had, on average, a greater decrease in occipital pain within six weeks, which lasted through the follow-up at six months.[18] TRFA can render long-term analgesia but introduces several potential risks, including dysesthesia, anesthesia dolorosa, hypesthesia, and the development of a neuroma. According to a study by Hoffman et al., among 50 patients with ON who received GON and LON TRFA, patients report, on average, a 76.3% pain relief that lasted for 6.5 months.[19] More studies regarding the efficacy of PRF or TRFA should are necessary for patients with occipital neuralgia.
Occipital Nerve Stimulation/Neuromodulation
Occipital nerve stimulation has been used to relieve severe pain caused by occipital neuralgia when conservative medical treatments and block procedures are ineffective. It involves placing nerve stimulator leads obliquely or horizontally near the bottom of the skull across from the GON location.[20] Some risks of this procedure include surgical infection and movement of the lead or generator after the operation. Based on a study by Johnstone et al., among eight patients with occipital neuralgia who received ON stimulation, seven of them were implanted a permanent lead once they had a 50% reduction in pain.[21] This type of procedure has been used for patients with primary headaches, such as migraines and cluster headaches, and patients with secondary headaches, such as occipital neuralgia and cervicogenic headaches.[22]
Ultrasound-guided Cryoneurolysis of the GON
Cryoneurolysis of the GON has been used to manage the symptoms of patients with ON. Even though there is limited evidence on this technique's efficacy, a previous study by Kastler et al., who performed seven cryoneurolysis procedures of the GON in six patients with occipital neuralgia, demonstrated the technique helped alleviate pain for three months in five of the patients.[23]
Dorsal Rhizotomy
Another possible treatment option for occipital neuralgia is dorsal rhizotomy of the C1 to C3 spinal nerves, in which the ventrolateral margin of the C1 to C3 rootlets become separated at the entry points.[2] Although there is little risk for patients to have complications, a complete upper cervical rhizotomy will lead to a loss of sensation in the scalp, and the procedure may not always relieve the pain. Also, the amount of pain that is alleviated may reduce over time. [2] According to a study by Gande et al., among 75 patients with occipital neuralgia who had dorsal rhizotomy, 35 patients reported having full relief of pain while 11 patients had partial pain relief, and seven patients had no pain relief at all. Twenty-one patients stated their activity levels were enhanced, while five patients had decreased activity levels after surgery.[24] In another study by Dubuisson, among 11 patients with occipital neuralgia who had 14 partial dorsal rhizotomies, pain near the GON decreased, and pain relief was regarded as good or excellent among 10 of the procedures performed.[25] More studies regarding the efficacy of dorsal rhizotomy are necessary for patients with occipital neuralgia.
Peripheral Neurectomy
Peripheral neurectomy has been suggested to be an effective surgical technique for patients with occipital neuralgia that provides effective pain relief in most patients. However, few studies have evaluated the efficacy of this treatment. Thus, more studies are required to fully assess the efficacy and possible complications for performing peripheral neurectomies among patients with ON.
Surgical Decompression
Botulinum toxin could potentially offer pain relief to patients with ON. Within presynaptic cholinergic nerve terminals, the toxin attaches to high-affinity recognition sites and blocks acetylcholine delivery.[2] Surgical decompression is another option, and a previous study stated GON decompression was 62% effective in reducing pain from occipital neuralgia.[2] However, a large number of patients may be refractory to surgical intervention. Jose et al. also reported that among eleven patients with refractory occipital neuralgia, who had GON surgical decompression, the average number of pain episodes decreased from 17.1 to 4.1 episodes every month. The average pain intensity also decreased significantly.[26] Three patients also had complete removal of pain, and only two patients did not experience significant improvement.[26] For GON microsurgical decompression, in a previous study investigating the efficacy of performing the procedure among 76 patients with headache symptoms, 89.5% of patients had their symptoms resolved while 3.9% of patients had a recurrence of their symptoms.[27] Even though all of the patients had GON hypoesthesia, they recuperated one to six months after the surgery. These results demonstrated microsurgical decompression might be an effective way to treat patients with occipital neuralgia.[27]
In addition to the surgical considerations above, physicians should take into account any anatomic details or variations for the GON, LON, and TON that were mentioned previously to reduce the risk of undesirable postoperative outcomes and help maximize the benefits for patients who are receiving treatment with regards to these occipital nerves.
Clinical Significance
Because the GON, LON, and TON play significant roles in the innervation of the scalp, they are often associated with occipital neuralgia. Based on the International Headache Society, patients with occipital neuralgia have a stabbing pain in the GON and LON dermatomes that originates from GON or LON compression and spans from the suboccipital area to the upper portion of the neck, the area behind the eyes, and the posterior region of the head.[1] Patients may also experience tenderness, hypoesthesia, or dysesthesia in the same locations. Tenderness in the affected areas and temporary relief of pain with local anesthetic nerve blocks confirm the diagnosis.[1] Because occipital neuralgia is associated with cranial nerves 8, 9, and 10, patients may experience nausea, dizziness, vision impairment, and congestion in the nose.[1] However, it is common to confuse occipital neuralgia with other diseases unless physicians notice other distinguishing factors. For instance, physicians must distinguish occipital neuralgia from infections, tumors, and congenital abnormalities, such as Arnold-Chiari malformation. They may confuse occipital neuralgia with migraines, cluster headaches, tension headaches, or hemicranial continua.[1] Physicians must also distinguish occipital neuralgia from cervicogenic headaches because occipital neuralgia is defined as neuralgia in the occipital nerves. In contrast, cervicogenic headaches arise from referred pain within atlantoaxial or upper zygapophyseal joints or trigger points inside the neck muscles.[1] Anticonvulsants, massage, physical therapy, nonsteroidal anti-inflammatory drugs, and muscle relaxants are usually first-line treatments.[28] If patients do not respond clinically to these treatments or minimally invasive procedures, such as PRF, other invasive treatments, such as nerve blocks, may be considered. Some conservative treatment options consist of correction of posture and reducing muscle pain.[1] However, many studies have yielded variable results regarding the efficacy of these treatments. There is a limited number of well-designed, randomized, case-control studies regarding the efficacies of these invasive treatments.[1]
Additionally, GON blocks have been used to treat other forms of headaches, such as migraines, cluster headaches, and cervicogenic headaches.[29] GON blocks appear to alleviate pain for a variable, short period. For instance, Lambru et al. reported, among 83 patients with cluster headaches, GON blocks resulted in an average pain alleviation period of 21 days.[30] In another study by Afridi et al., among 26 out of 57 nerve blocks in 54 patients with migraines, GON blocks led to an average pain alleviation period of 30 days. For patients with cluster headaches, GON blocks led to an average pain alleviation period of 21 days.[31] RFA has also been used to provide long-term relief; however, RFA may cause certain complications, such as post-denervation neuralgia.[29] For cervicogenic headaches, GON and LON nerve blocks are some conventional treatments.
Patients with whiplash injuries may also suffer from third occipital headaches. Whiplash injuries are often associated with motor vehicle accidents, and patients with these injuries may have stiffness and pain in the neck, paresthesias, memory problems, and psychological pain.[32] Previous studies have demonstrated radiofrequency neurotomy may provide complete pain relief for patients with TON headaches. However, the procedure has some side effects, such as temporary ataxia, dysesthesia, and numbness.[33] Moreover, the process has to be repeated once the coagulated nerve recovers.[33]