Continuing Education Activity
This activity reviews in detail an innovative surgical approach to skin grafting for vitiligo and chronic non-healing ulcers, known as the "Jodhpur technique," and explains the role of the healthcare team in the optimization of outcome in patients with stable vitiligo and non-healing ulcers who undergo this procedure as the preferred surgical approach.
Objectives:
Describe the essentials of the conventional skin grafting techniques highlighting the limitations associated with them, and how the Jodhpur technique offsets many of these problems.
Summarize the basic requirements (devices & consumables) needed for the procedure, highlighting the simplicity of the procedure in terms of minimalistic requisites for infrastructure, and personnel.
Explain the procedure of the Jodhpur technique and its modifications in a step-by-step fashion, walking through the technique for straightforward comprehension.
Review the role of the interprofessional team in the Jodhpur technique in the treatment of vitiligo and chronic non-healing ulcers, and how collaboration and communication can improve patient outcomes.
Introduction
The JODHPUR TECHNIQUE is a very simple, yet very effective and extremely low-cost innovative modification of the standard skin grafting technique. In simplified terms, it refers to an autologous non-cultured, non-trypsinized keratinocyte-melanocyte cellular graft technique developed and perfected by a working group of leading dermatology surgeons of Jodhpur (a heritage city in the state of Rajasthan, India). The long learning curve of mastering tissue grafting techniques, and the lack of expert set-up requiring special cellular culture media, trypsinization, etc. in a majority of public sector hospitals in developing countries were the two main contributing factors that propelled the innovative improvisation of the Jodhpur technique.[1]
Background
Skin grafting is perhaps one of the oldest surgical techniques employed for the closure of a wound or coverage of desquamated/peeling skin resulting from burns, scalds, trauma, chronic non-healing wounds, and surgical removal of large skin growths. The second major application of skin grafting is in replacing a specific cell-deficient skin such as melanocyte-depleted depigmented skin or post-burn leucodermic scar with a normal donor skin with the intent of replenishing the cellular pool of the recipient area, thereby re-pigmenting it.
It is essential to know the essential difference between a skin graft and a flap repair. In contrast to flaps that remain attached to a source of blood supply through a pedicle, skin grafts are completely avascular and replacement is necessary over a prepared recipient bed to restore the nourishment of the donor skin.
In Dermatosurgery, skin grafting is most commonly used in vitiligo surgery and for the induction of healing of chronic non-healing ulcers (CNHL). It may also be needed during scar revisions and in post-burn leucodermic scars.
Different types of skin grafts:
Broadly speaking, skin grafts can fall into three classifications:
(1) Based on the cellular/tissue composition of the graft [2]:
- Split-thickness skin grafts (STSG) - full epidermis and a superficial part of the dermis.
- Full-thickness skin grafts (FTSG) - full epidermis and full dermis, and a small part of the subcutaneous fat
- Composite grafts - these are composed of skin and another type of tissue, usually cartilage.
Split-thickness skin grafts further subclassify into ultra-thin STSG, thin or Thiersch–Ollier (0.125 to 0.275 mm) STSG, intermediate, or Blair–Brown (0.275 to 0.4 mm), and thick or Padgett (0.4 to 0.75 mm) split-thickness grafts.[3]
(2) Based on the technique of harvesting the graft
(2.1) Tissue grafts - These techniques refer to the direct harvesting of sheets of cells from the donor area. They may be procured by:
- Mini/Micro Punch grafts (MPG) - miniature or micro-sized punches of skin are harvested from the donor site and placed in punched out holes in the recipient skin
- STSG - Skin of the desired thickness gets harvested using a dermatome, and it comes out as a thin sheet
- Suction blister Grafts - Ultra-thin skin grafts get harvested by a special protocol of applying suction at the donor site
Although the process of harvesting tissue grafts involves minimal surgical equipment and cost, tissue grafts can be useful for only a limited surface area per treatment session.
(2.2) Cellular grafts -
Cellular grafts include cellular suspensions of pure melanocytes, or keratinocytes, or their admixture, with latest inclusions being that of dermal cells and/or follicular cells. Cellular grafts are prepared from a smaller surgically harvested skin sample, by either culturing it or using it as a non-cultured suspension. The major advantage of these suspension and culturing techniques is that they permit treatment of affected skin manifold larger than the donor area.[4]
- Cultured cell suspension techniques - Although these provide treatment of a much larger surface area of the affected skin, the cultured techniques suffer from the limitations of being time-consuming, expense owing to the need for special culture media and specific laboratory conditions maintained over several weeks and need of highly trained personnel.
- Non-cultured cellular grafting techniques - To obviate the logistic and cost issues of cultured techniques, the harvested skin gets subjected to cell separation by incubating it with trypsin/trypsin-EDTA at 37 degrees C for 20 to 30 minutes. The resultant suspension is thoroughly rinsed with lactated Ringer's solution, followed by complete manual separation of any dermal tissue. The epidermal fragments are centrifuged for a few minutes to create a homogenous cell pellet, which then gets resuspended in lactated Ringer’s solution. Thus, despite being technically and logistically less demanding than the cultured techniques, the non-cultured techniques, most common being the melanocyte-keratinocyte transplant procedure (MKTP), also involve special chemicals such as trypsin for cell separation and need for a decent laboratory back-up with at least an incubator and centrifuge.[5]
As we learn the intricacies of the Jodhpur technique in subsequent sections, one would realize that it is, in fact, a marriage of the cellular and tissue skin grafting techniques. It provides the advantage of large recipient area coverage with a small donor skin area (typical of cellular techniques), albeit without the need of an expensive infrastructure, chemicals, devices or culture media.
Anatomy and Physiology
Since the two chief indications of Jodhpur technique include repigmenting stable lesions of vitiligo, and induction of healing in CNHUs, few important aspects of the functional anatomy of these conditions should be known to the dermatosurgeons:
1) Vitiligo Surgery - The quintessential criteria to be fulfilled before considering a vitiligo patient as a suitable candidate for surgical intervention pertains to acceptable stability of the lesions and the disease to prevent graft failure, recurrence at recipient site as well as the appearance of vitiligo at the donor site due to Koebner's phenomenon. In the past, arbitrary clinical criteria suggested by many workers were considered to be sufficient for this qualification.[6] But with the advent of discovery and reported publications on dermoscopic predictors of disease stability in vitiligo, recent recommendations are that in addition to those clinical criteria, the dermoscopic criteria of stable vitiligo should also be established before attempting any form of surgical correction of vitiligo, including the use of Jodhpur technique.[7][8]
2) CNHUs - It is important to note that the diverse etiologies leading to non-healing ulcers mandate thorough pre-surgical evaluation, medical correction of any modifiable factors, and assessment of the possibility of the Jodhpur technique or any skin grafting method in healing them. The majority of CNHUs is located on the lower limbs, primarily owing to gravity-associated compromised vascular supply (whether overt or occult) and higher possibility of trauma. Since vascular replenishment of the ulcer bed is an important consideration in CNHUs (in contrast to vitiligo), consideration of flaps, techniques like platelet-rich plasma (PRP) and platelet-rich fibrin matrix (PRFM), injection of growth factors, hyperbaric oxygen, etc. must be considered before being convinced that the Jodhpur technique may suffice and provide healing without the logistic and infrastructural essentials required for the other approaches.
Coverage Ratio with Jodhpur technique
In cases of vitiligo, the Jodhpur technique allows coverage of a recipient area with the harvesting of as low as 20 to 30% of that area from the donor site.
Indications
The Jodhpur technique has been successfully used in two major indications [at present]:
(1) Stable Vitiligo - In one published study conducted in 154 patients, 437 vitiligo patches were treated with the Jodhpur technique followed by PUVA therapy. Researchers observed more than 75% re-pigmentation in 41% of the patches.[9] The regions that showed high (over 75%) levels of repigmentation included the thigh (100%), face (75%) and, trunk (50%). showed maximal excellent improvement, whereas patches on joints and acral areas did not show much improvement.
(2) CNHUs - Recently, researchers attempted repurposing of the Jodhpur technique for chronic non-healing ulcers involving the leg, refractory to multiple ulcer-treatment modalities. Seventeen patients with lower limb CNHU of varied etiology were enrolled. Of these, 7 (41.2%) were of diabetic origin, 4 (23.5%) were secondary to chronic venous stasis (in patients who were either poor candidates for vascular surgery or had failed one), 4 (23.5%) were trophic ulcers secondary to leprosy, and 2 (11.8%) were of vasculitic origin. All (100%) ulcers showed complete healing within 5 to 6 weeks with no complications [data and study under publication].
Contraindications
COMMON TO VITILIGO AND CNHUs
- Known allergy to local anesthetic agents
- Known personal history or the tendency for keloidal/hypertrophic scarring
- Bleeding/clotting disorders
- Chronic uncontrolled severe debilitating diseases such as severe uncontrolled diabetes, renal and/or hepatic failure
- Unreliable and uncooperative patient
- Unrealistic expectations
- Active Infection - bacterial, viral, fungal or herpetic infection at the recipient/donor site
VITILIGO
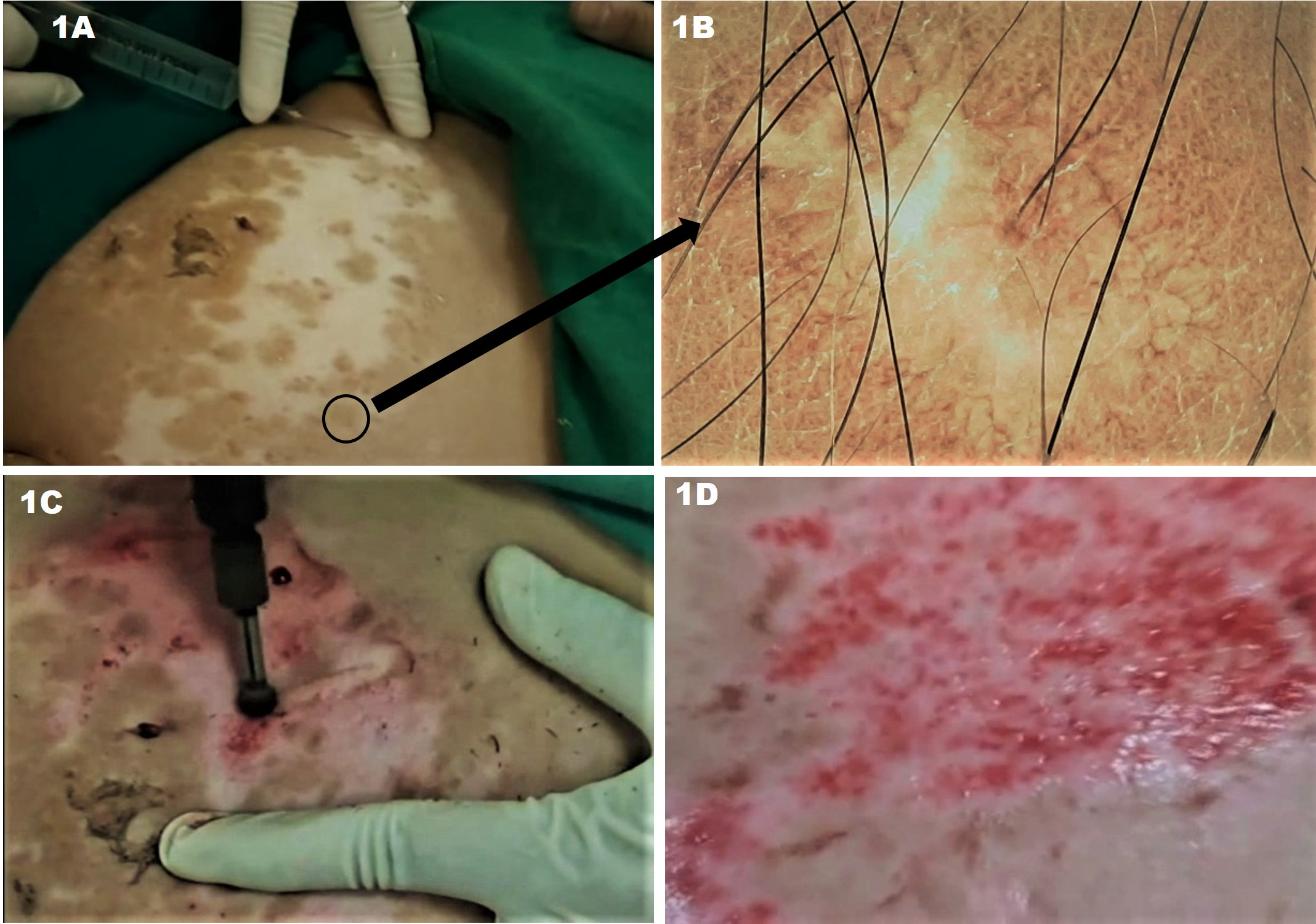
- Unstable vitiligo - The lesional stability of a vitiligo patch is of extreme importance not only for the successful outcome of the surgery but also to prevent the development of vitiligo at the donor site by Koebnerization. Various criteria based on clinical history, and gross lesional examination,[6] Wood's lamp evaluation,[10] test-grafting,[11] biochemical, and immunological parameters,[12] and histological features,[13] have been proposed in older studies to establish the stability of a vitiligo lesion.[14] However, these are being gradually replaced with dermoscopy,[7][8] and other non-invasive techniques for assessment of cutaneous lesions such as in vivo reflectance confocal microscopy (RCM).[15] Given the availability and affordability of a dermoscope, and good reliability in the prediction of vitiligo stability, the Jodhpur technique now considers dermoscopic features as the standard predictor of lesional stability [Figures 1A & 1B].
CNHU
- Uncontrolled primary disease - For example, uncontrolled diabetes with diabetic ulcer
- Poor general and nutritional health, or any factor that may impede the post-operative healing
Equipment
The convenience factor of the requirement of minimal equipment and highly cost-effective consumables are key advantages of the Jodhpur technique:
DEVICES
- Dermabrader - Manekshaw's manual dermabraders, or motorized dermabrader
- Sterile glass slides
CONSUMABLES
- Material for sterilizing the donor and recipient sites - sterile gauge pieces, betadine solution, surgical spirit
- Material for Local Anaesthesia - Syringes and needles, 2% to 4% lignocaine solution (without adrenaline)
- Sterile spatulas
- Normal saline, and saline-soaked sterile gauge pieces
- 2% mupirocin ointment/any other broad-spectrum topical antibacterial ointment
- Collagen dressings - wet/dry
- Sterile cotton pads, micropore tapes, and bandages
Personnel
One of the advantages of this technique is that the requirement of personnel (in terms of the number of surgeon(s) and paramedical staff), as well as the amount of their prior experience to perform a proper skin grafting by Jodhpur technique, are both minimal.
A single dermatology surgeon with exposure to 2 or 3 surgeries and preferably at least one-time assistance as a co-surgeon with a senior dermatology surgeon experienced and conversant with the Jodhpur technique is sufficient as the primary and the only required doctor. And although the availability of a general minor procedure room or minor operating theater staff nurse/technician helps expedite the completion of the surgery, the technique has been undertaken several times by the authors and their students single-handedly. Of course, in the latter scenario, it is expected that the surgical nurse/technician would have ensured the availability of all material and kept them sterile for the surgeon's use.
Preparation
Preparation at recipient site [Figure 1]
Basic Principle - Recipient-site preparation is an essential step of any skin grafting procedure, and is performed to facilitate the access of the donor material to the sub-epidermal structures of the recipient site. The procedure entails removal of the epidermis from the underlying dermis at the dermo-epidermal junction (DEJ) or the upper papillary dermis; necessary for the adherence and nutrition of melanocytes and other supportive cells contained in the donor material. Grafting of the donor material at a adequately prepared recipient site of the necessary for melanocyte adherence and nutrition. After proper bandaging, plasmatic imbibition of the grafted material begins and continues for the first 24 to 48 hours, followed by neoangiogenesis that subsequently maintains the cellular nutrition.[16]
- This area should be prepared first so that the donor material can be promptly overlayed and dressed.
- Local Anesthesia - After taking all aseptic precautions, the area gets anesthetized by infiltrating it with 2% to 4% lignocaine (plain, without adrenaline). It is important to note that adrenaline SHOULD NOT BE USED since the next step of dermabrasion of the skin is dependent on the end-point of pin-point bleeding. Since adrenaline is a vasoconstrictor, it would mask this end-point, leading to deeper dermabrasion leading to graft failure and/or scarring.
- Dermabrasion - The anesthetized recipient area is then dermabraded using either Manekshaw's manual dermabraders, or preferably a motorized dermabrader with diamond fraise until reaching the end-point, which is uniform pin-point bleeding. This end-point indicates that we have reached the papillary dermis indicating that the recipient area is now ready to accept the graft. The use of motorized dermabrader is preferable as it provides more uniform abrasion compared to manual dermabraders. The surgeon may also use superficial radiofrequency ablation, pulsed erbium-YAG laser, or even ultra pulse CO2 laser to prepare the recipient site.
- Hydration - After this, the recipient area is kept hydrated with gauze pieces soaked in sterile normal saline placed over it till the donor graft material is ready to be overlayed.
Alternative methods for recipient site preparation:
In the classical Jodhpur technique, dermabrasion remains the preferred way of recipient site preparation owing to its simplicity, easy and cheap availability of both manual and motorized dermabraders, and well-defined endpoint of pinpoint bleeding. One must be aware of other approaches and may use them if machine availability and cost to the patient does not impede the very purpose of preferring the Jodhpur technique.
Various methods exist for recipient-site preparation in skin grafting for vitiligo. These include the cryogenic blister formation with liquid nitrogen, radiofrequency (RF) ablation with the ball probe, creating suction blisters by negative pressure technique, phototoxic ablation with psoralen plus ultraviolet A (PUVA), and ablative lasers such as the erbium: YAG and CO2 lasers.[16][17] Each of these techniques has certain advantages and suffers the limitation of specific complications. It is important to remember that the endpoint of pinpoint bleeding has only become standardized in the context of using mechanical dermabrasion.
- Liquid Nitrogen - Although it is efficacious, the delayed formation of blisters (usually after 24 hours of liquid nitrogen spray), and the possibility of peripheral dyschromia (both hypo as well as hyperpigmentation), and reports exisst of hypertrophic scarring when recipient site preparation used cryotherapy.[18]
- Mechanical Suction blister induction - Inducing blisters using a negative pressure system with a set of syringes and three-way cannulas is considered to be superior to most of the methods in terms of creating the near-ideal recipient site since the separation occurs precisely at the DEJ, and the approach provides a more favorable microenvironment by ensuring adequate serous drainage in the prepared areas.[19] The demerits of this approach include the time required for the formation of blisters (at least 3 to 4 hours), the discomfort experienced by the patients during the induction of blister formation, and limited yield of the prepared skin rendering it inferior to other methods for large areas of vitiligo lesions.
- PUVA - The use of PUVA for phototoxic blister formation at the recipient site is a time-efficient method for the preparation of large areas, with the additional advantage of minimal to no risk of scarring. However, the concern regarding PUVA triggered carcinogenesis makes it a non-preferred approach, especially in lighter skin types.[20]
- CO2 laser - has been used both in the ablative mode (with intermittent instead of continuous beams) as well as in the fractional mode. The use of pulsed, ultra pulsed, or fractional CO2 laser offers the advantages of high speed (rapid coverage of large areas), uniformity of epidermal ablation, and precise depth control over sites with delicate and irregularly shaped skin such as the perioral, periocular, and perinasal areas.[21] However, this approach increases the cost and is known to often result in uneven repigmentation and transient hyperpigmentation.[16]
- Erbium: YAG laser - In contrast to the CO2 laser, the Erbium: YAG laser ablation attained through 3 to 6 passes provides all the benefits of the former such as efficient and controlled tissue ablation, and time-efficiency in preparing skin over large areas and irregularly-contoured regions. Since the depth of penetration with the 2940 mm erbium: YAG laser is only one-sixth that of CO2 lasers, its use preempts the possibility of thermal necrosis and allows for more precise tissue ablation.[22] One unique advantage of using this laser is the lack of requirement for recipient site anesthesia owing to minimal pain associated with the shots of Er: YAG laser.[23] Thus, this laser offers the convenience of operator-use, and also provides a relatively bloodless field for easier surgery by the specialist.[16]
- Radiofrequency ablation combined with mechanical dermabrasion - This approach involves the application of the ball-shaped loop of an RF device, set on low power cut/coagulation mode. The resulting superficial blistering is followed by using gauze to wipe off the ablated epidermis. The preparation then completes by using a manual dermabrader to induce pinpoint bleeding. The advantage of combining RF with manual dermabrasion is a reduction in preparation time, and efficacy similar to that attained with CO2 laser, albeit without the substantial cost incurred when the later is used.[17]
Technique or Treatment
Harvesting the graft material from the Donor site [Figure 2]
- Donor Site - As with other conventional skin grafting methods, the usual donor sites are the lateral/anterolateral part of the thighs, buttocks, and outer aspect of the arms. However, since the Jodhpur technique depends on the successful procurement of a good cellular pool of keratinocytes-melanocytes, any site with apparently healthy skin may be used. In fact, in the Jodhpur technique, a previous surgically repigmented site may also be used as a donor area.
- Modification of the donor site for JODHPUR TECHNIQUE - A new modification of the donor site selection in the Jodhpur Technique for vitiligo is to take the perilesional skin of the lesion, or even a previous surgically-repigmented site [Figure 2A]. Advantages of the former approach being: (1) reduced morbidity of patients undergoing surgery as single site is being traumatized; and (2) graft material would be rich in melanocytes and keratinocytes of the same topographical region, which may hypothetically be more physiologically matched to the pigment deficient lesion and provide better color match and overall cosmetic acceptance.
- Local Anesthesia - After taking all aseptic precautions, the donor area is also anesthetized by infiltrating it with 2% lignocaine (plain, without adrenaline). Adrenaline is avoided for the same reason, as explained for the recipient site preparation.
- Dermabrasion - Similar to the procedure followed at the recipient site, the anesthetized donor area is dermabraded using either Manekshaw's manual dermabraders, or preferably a motorized dermabrader with diamond fraise until reaching the end-point, which is uniform pin-point bleeding. The modification in the Jodhpur technique is that a thick layer of an antibiotic ointment, preferably a 2% mupirocin ointment, gets smeared over the donor area before dermabrasion [Figures 2B-2D]. This ointment serves to entrap the epidermal cells that would separate doing dermabrasion. Upon reaching the end-point, a thick paste is obtained consisting of epidermal cells, both keratinocytes, and melanocytes, few dermal fibroblasts, free melanin, etc. entrapped in the ointment [Figure 2E]. This cellular graft in the form of this paste is collected with a spatula [Figure 2F] and is ready to be overlayed on the already prepared recipient site.
Placing the graft over the Recipient site [Figure 3]
- The donor graft mucilage/paste is transferred to a slide and mixed with saline to form a homogenous paste [Figures 3A-3B].
- This homogenized paste then gets overlayed over the prepared recipient site taking care that a thin layer is applied using the spatula [Figure 3C].
- This grafted recipient area is covered with wet/ dry collagen dressing, followed by dressing with antibiotic ointment soaked gauge [Figure 3D].
- The third layer consists of a cotton pad which requires secure anchoring with a bandage.
Post-procedure Instructions
- The dressing should be allowed to remain for at least seven days, with avoidance of wetting. However, readers must note that the expected transfer of the cells from the donor paste harvested during Jodhpur Technique onto the recipient site finishes within 48-72 hours of firm anchoring of the donor material over the recipient site. However, it is preferable to keep the dressing in place for seven days to ensure maximum probability of cellular transfer.
- A short course of oral antibiotics and nonsteroidal anti-inflammatory drugs [NSAIDS]
- Review for follow-up on the seventh day or earlier if any issue arises.
Post-procedure Follow-up
- The dressing gets opened on the seventh day, and the recipient area checked for any infection, which is very rare.
- The area is then left open, although a small dressing may be done in extremities, to prevent traumatic insult to the healing area
- In cases of vitiligo, phototherapy with nb-UVB or PUVASol is started around the 14th day onwards and continued till the maximum repigmentation is achieved (usually 4 to 6 weeks with 2 to 3 sessions/week)
The expected time-period for the outcome
- Vitiligo - Pigmentation usually begins at 8 to 12 weeks, and complete and uniform pigmentation is generally attainable in 16 to 20 weeks.
- CNHU - Although the experience of the Jodhpur technique for this indication is lesser, in our experience, around 5 to 6 weeks after a single session of Jodhpur technique induces over 95% healing of the ulcer.
Complications
The Jodhpur technique is by and large free of any significant complications. Still, one must be aware of the expected peri- and post-operative events, sometimes construed as 'adverse-effects' or complications by the patients, as well as potential complications that may arise in an odd case:
PERIOPERATIVE
- Pain at the recipient and/or donor site - It rarely causes discomfort, and any troubling painis rare, usually the case of a patient who received local anesthetic agent from a technically dysfunctional batch. But awareness of rare cases of true resistance to local anesthetics, which may be genetic [24], or acquired. There are only rare reports of actual acquired resistance in patients with specific spinal neuropathy. There are reports of delayed onset of analgesics and some local anesthetics in chronic smokers.[25]
- Surgical site infection - this is uncommon, and the use of broad-spectrum antibiotics can further minimize the possibility started immediately after the procedure.
DELAYED
- Keloid/Hypertrophic scar formation - Keloid formation is most common in patients who have a keloidal tendency (which may be known or unknown to them), and despite pre-operative work-up, this information does not come to the attention of the dermatology surgeon. Hypertrophic scarring, on the other hand, may occur in rare cases, especially if the healing delays for any reason and if the surgical sites involve the areas around the joints such as the knee or elbow. In either case, 2 to 4 shots of intralesional scar suppressive therapy three times weekly, using triamcinolone, and/or verapamil or 5-fluorouracil with/without silicone sheet compression therapy is often sufficient to resolve this complication.
- Failure of repigmentation of the recipient site OR healing of CNHU - This has been observed in only 10 to 15% of the patients only. Partial repigmentation or complete failure of repigmentation after any surgical grafting technique depends on predictable factors like inappropriately/inadequately performed procedure (e.g., superficial or very deep dermabrasion, delay in starting or delivery of suboptimal phototherapy energy) as well as the unpredictable factor of individual skin response. A second session may be curative, but needs further investigation for confirmation.
- Koebnerization at the donor site in vitiligo patients - This is also extremely rare, and is expected to happen only if the pre-operative evaluation regarding patient's fitness for surgery (irrespective of the technique used) has occurred in haste or inadequately (vide supra).
Clinical Significance
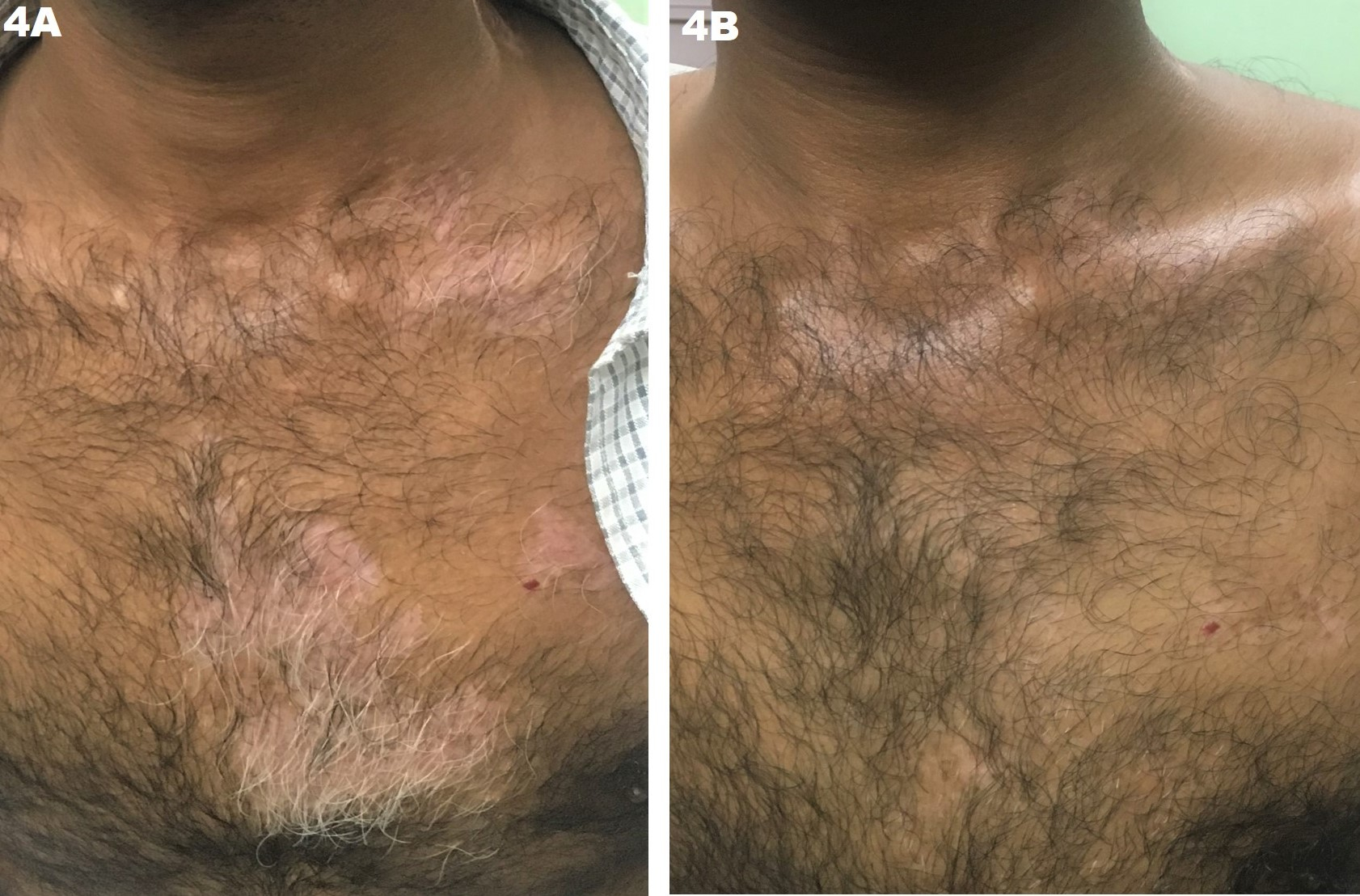
The Jodhpur technique not only bridges the tissue and cellular grafting approaches, its overall efficacy outcome in vitiligo [Figure 4], and CNHU's are very encouraging.
The advantages of this approach include:
1) Need for minimum infrastructural and monetary support in terms of laboratory, specialized equipment, special media, etc.
2) A broad spectrum of donor sites that may be available in this technique, compared to the relatively limited options in other skin grafting techniques.
3) A relatively high coverage ratio: In cases of vitiligo, the Jodhpur technique allows coverage of a recipient area with the harvesting of as low as 20 to 30% of that area from the donor site.
4) An easy learning curve for the dermatologist or dermatology surgeon, and need for minimal personnel for conducting the procedure.
5) High efficacy and minimal complications (such as textural abnormalities, uneven pigment matching, etc., usually encountered with STSG and MPG).
Enhancing Healthcare Team Outcomes
Although this technique can be quickly learned and mastered by any surgeon (dermatologist, general surgeon, plastic surgeon, burn specialist) who is conversant with the basic principles of skin grafting, at present, it is probably best for dermatologists who have observed and assisted in few procedures under the apprenticeship of a dermatology surgeon experienced in this technique.
However, the primary objective of developing this technique, i.e., empowering all medical professionals involved in the care of patients with vitiligo and/or CNHU's with this straightforward and cost-effective technique, is not difficult to achieve. Inter-specialty exchange of knowledge and skills during focused conferences and/or workshops on skin grafting, vitiligo surgery, management of CNHU's, etc. are already becoming popular globally. Inclusion of JODHPUR TECHNIQUE in the program of such inter-specialty CMEs, preferably with video demonstration, may serve the purpose of realizing the objective as mentioned earlier.
Similarly, training of surgical nurses/technicians as proficient assistants to the surgeon is also relatively straightforward and easy. It must be undertaken at individual centers to improve therapeutic outcomes and prevent complications.
This procedure requires coordination from the entire interprofessional healthcare team.
CURRENT EVIDENCE LEVEL OF JODHPUR TECHNIQUE[9][1]:
- For vitiligo - LEVEL 5 [two published case series involving a total of 455 vitiligo lesions treated with Jodhpur technique]
- For CNHUs - LEVEL 5 [one published case report, one large case series under publication process & expert opinion]
Nursing, Allied Health, and Interprofessional Team Interventions
- Ensure consent is obtained
- Educate the patient about the procedure
- Prepare the sterile instruments and tray for the procedure
- Prep the patient
- Assist the surgeon during the procedure
Nursing, Allied Health, and Interprofessional Team Monitoring
- Monitor vital signs
- Assess wound in the post-operative period
- Provide instructions for wound care in the post-operative period