Introduction
The middle cerebral artery (MCA) is a critical artery which has an extensive clinical significance. The MCA is part of the circle of Willis anastomotic system within the brain, which forms when the anterior cerebral arteries anastomose anteriorly with each other through the anterior communicating artery and posteriorly with the two posterior communicating arteries bridging the MCA with the posterior cerebral artery on each side. The MCA is the most common pathologically affected blood vessel in the brain.
Structure and Function
The aortic arch gives rise to the brachiocephalic artery, from which subsequently stems the right common carotid artery; the left common carotid artery branches off the aortic arch just downstream the brachiocephalic trunk. The left and right common carotid arteries run along parallel to each other and divide near the angle of the mandible to the external and internal carotid arteries. The external carotid supplies the face and neck branching off immediately, while the internal carotid arteries do not branch until the origin of the ophthalmic artery bilaterally. Subsequently, the internal carotid arteries bifurcate onto the anterior and middle cerebral arteries, on each internal carotid artery. The largest terminal branch of the internal carotid artery, the MCA divides into four main surgical segments, denominated M1 to M4. The M1 segment extends from the ending of the internal carotid artery, perforating the brain up to its division. The M2 segment bifurcates or occasionally trifurcates. It travels laterally to the Sylvian fissure, and its branches end in the cerebral cortex. The M3 segment travels externally through the insula into the cortex. Finally, the M4 segments are thin and extend from the Sylvian fissure to the cortex.
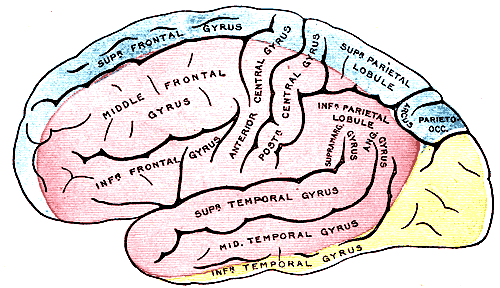
The primary function of the MCA is to supply specific regions of brain parenchyma with oxygenated blood. The cortical branches of the MCA irrigate the brain parenchyma of the primary motor and somatosensory cortical areas of the face, trunk and upper limbs, apart from the insular and auditory cortex. The small central branches give rise to the lenticulostriate vessels, which irrigate the basal ganglia and internal capsule. The superior division irrigates the lateral inferior frontal lobe, which involves the Broca area responsible for speech production, language comprehension, and writing. The inferior division of the MCA irrigates the superior temporal gyrus, which involves Wernicke’s area responsible for speech comprehension and language development.
Embryology
Vasculogenesis is the process of de novo blood vessel formation early in embryonic development. Angiogenesis is a similar process but is not gene dependent and has the primary purpose of repairing damaged vessels. Both vasculogenesis and angiogenesis depend on vascular endothelial growth factor (VEGF). Similar to other blood vessels, the vasculogenesis process of the MCA begins when extraembryonic mesodermal cells differentiate into angioblasts. Angioblasts form angiogenic cell clusters, which later differentiate into the endothelium of blood vessels. The development of the adult arterial pattern depends on the aortic arches. There are 6 embryonic aortic arches, enumerated in a rostral to caudal order from 1 to 6 for their study and development. The fifth aortic arch never develops in humans. The third aortic arch is the origin of the right and left common carotid arteries, and the right and left internal carotid arteries, which further give rise to the middle cerebral arteries bilaterally. As previously mentioned, vasculogenesis is a genetically driven process that allows for physiologic and anatomic variants.
Physiologic Variants
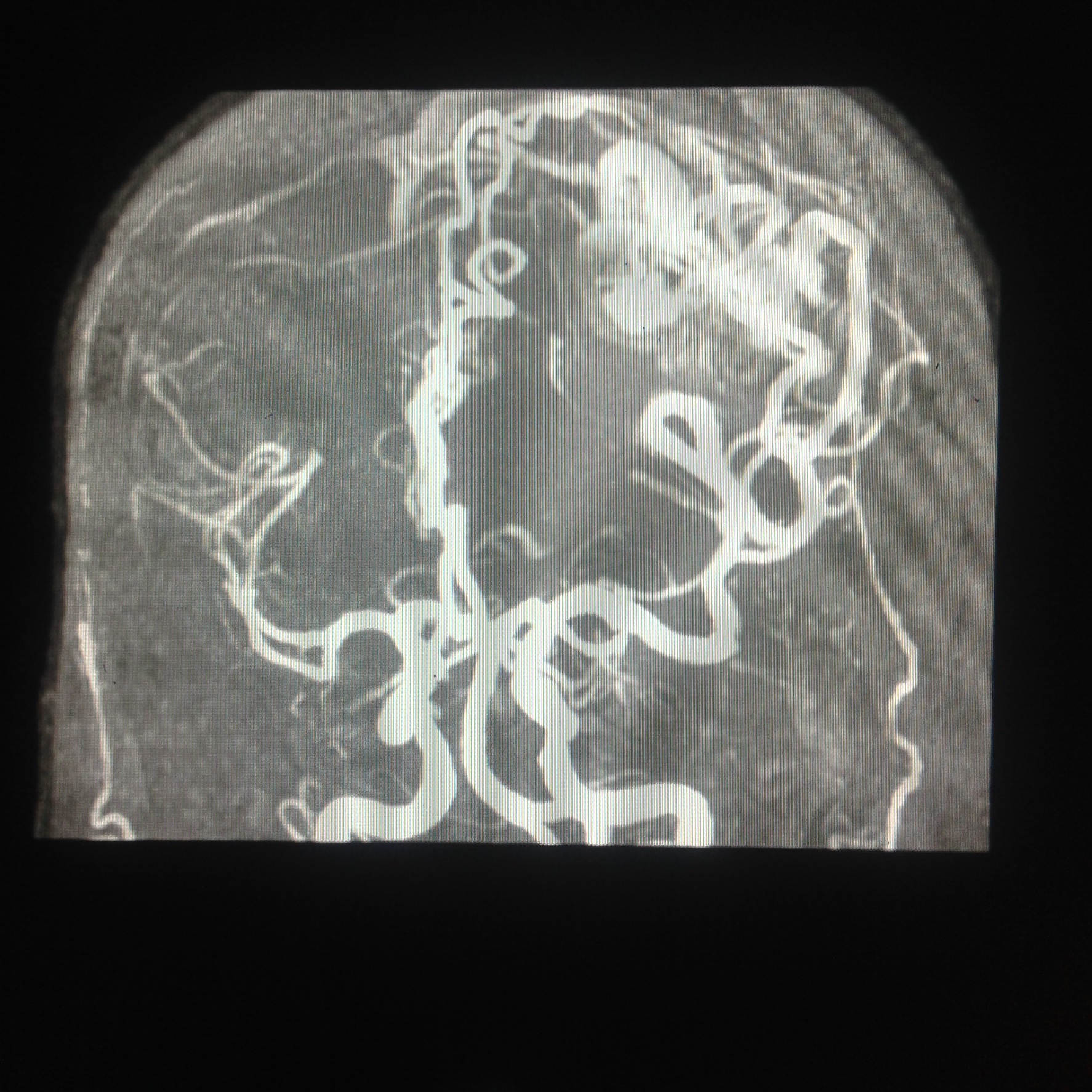
Physiologic and anatomic variants are important for guidance during vascular surgery. Some studies related a higher risk of aneurysm formation in the MCA with certain MCA variants. A retrospective study of 350 patients used computed tomography angiography (CTA). Bifurcation of the MCA before the genu without a dominating post-division trunk was the most common variant; however, variants include bifurcation and trifurcations before and after the genu. Also, the study observed upper, lower, middle, and no branch domination. Aneurysms appeared predominantly in the M1 surgical segment. However, they also appeared in the M2 segment, lenticulostriate vessels, and near cortical branches. A study suggested that domination of upper post-division trunk of the MCA have a higher risk of MCA aneurysm formation. The anatomic variants can partly explain the aneurysm formation and stroke incidence. A deeper insight into the implication of these variants warrants further studies.[1]
Surgical Considerations
Vascular surgeons are familiar with the most common anatomic variants, which help them decide on the best surgical approach. CTA is an iodine-rich contrast-enhanced visualization, which surgeons often uses to detail the vasculature and visualization of the morphology and location of the lesion. Vascular surgeons have the challenge of deciding whether to intervene surgically and the right tempo and approach to take. They typically prefer early intervention (within 2 weeks of stroke onset). A retrospective analysis contrasted early (less than 2 weeks) with delayed (2 to 8 weeks) carotid endarterectomy intervention results for minor and moderate strokes of the MCA. Both early and delayed interventions had satisfactory outcomes, although early endarterectomy seemed to avoid recurrent strokes best.[2] Studies compared stent-assisted embolization with surgical clipping of MCA bifurcation, wide-necked aneurysms for Hunt-Hess grade 0 to III subarachnoid hemorrhage. Both approaches yielded beneficial results with no statistically significant advantage of one method over the other.[3] Studies compare long-term patency of extracranial to intracranial and intracranial to intracranial bypass procedures. Intracranial reconstructive techniques have globally better results although both have a high likelihood of revascularization. Bypass procedures that remain patent for 1 week have a higher probability of remaining patent long-term.[4] The variables described prompt decision making to be a complex process that depends highly on the vascular surgeon’s experience and judgment. All the approaches mentioned above have an overall favorable outcome.
Clinical Significance
The middle cerebral artery is the most common, pathologically affected blood vessel overall. We describe some of the most common pathologies below.
Embolism of the MCA
An embolism is a detached mass, typically a dislodged thrombus, gas, or fat, which is transported through the blood vessels until it is lodged in the MCA. The arterial occlusion impedes perfusion of oxygenated blood to the brain parenchyma, resulting in an ischemic stroke causing cerebral edema and brain parenchyma tissue necrosis. As a general rule, a proximal occlusion will cause damage to a large surface area and be devastating. In contrast, a distal occlusion will cause damage to a small surface area, resulting in a less severe clinical presentation. Thrombus formation commonly is associated with sites proximal to the MCA, such as internal carotid plaques, common carotid plaques, and atrial fibrillation, resulting in thrombus formation and embolism. Furthermore, it is worth noting that cardiac defects such as atrial septal and ventral septal defects may result in a paradoxical embolism. This subtype is denoted as such because the thrombus being transported through the superior or inferior vena cava bypasses the respiratory circulation through the cardiac defects and potentially result in an MCA embolism.
As previously mentioned, an embolism of the MCA results in an ischemic stroke. A stroke of the MCA is denoted as middle artery syndrome. Middle artery syndrome presents with contralateral sensory loss of the legs, arms, and lower two-thirds of the face due to tissue necrosis of the primary somatosensory cortex. Contralateral paralysis of the arms, legs, and face may be observed due to necrosis of the primary motor cortex, which is observed clinically as muscle weakness, spasticity, hyperreflexia, and resistance to movement (upper motor neuron signs). Ipsilateral eye deviation is observed due to frontal cortex Brodmann area 8 becoming ischemic, impairing planning of eye movement, symptoms that are exacerbated by contralateral homonymous hemianopsia. A dominant, most commonly left-sided, hemisphere stroke results in Broca aphasia if the superior division of the MCA is affected. In contrast, Wernicke’s or conduction aphasia may be seen if the inferior division of the MCA is affected. A non-dominant, most commonly right-sided, hemisphere stroke results in hemineglect syndrome, presenting with anosognosia, apraxia, and hemispatial neglect.
Lenticulostriate Infarct
Infarction of the deep, perforating lenticulostriate branches of the MCA also is most likely caused by an embolism of cardiac origin. Lenticulostriate vessels tend to result in lacunar infarcts, which may be differentiated from those above due to lack of cortical involvement. The most common clinical presentation of lacunar infarcts of the lenticulostriate branches is one of pure motor involvement. This presentation is due to the posterior limb of the internal capsule commonly being affected. It is stipulated that lipohyalinosis may have a large role in the development of lenticulostriate infarcts; however, additional evidence to support this claim is needed.[5]
Charcot-Bouchard Microaneurysms
Charcot-Bouchard microaneurysms are stipulated to be caused by chronic hypertension in small terminal lenticulostriate vessels. The rupture of the Charcot-Bouchard aneurysms is associated with intracerebral hemorrhages, which tend to cause tissue necrosis due to lack of anastomosing blood vessels. Common sites affected by Charcot-Bouchard microaneurysms include the thalami, basal ganglia, cerebellum, and pons.[6]
Arteriovenous Malformations
Arteriovenous malformations (AVMs) are congenital arteriovenous connections which can be found anywhere in the brain. Clinically, they most commonly are seen in young patients ranging from 20 to 40 years of age and carries a yearly hemorrhage risk between 1% to 4%. Conventional surgery, radiosurgery, and endovascular embolization are commonly used to treat AVMs.[7]
Saccular Aneurysms (Berry aneurysms)
Saccular aneurysms are the most common subtype of an aneurysm. These usually present in areas of bifurcation/trifurcation due to blood vessel weakness and outpouching. Saccular aneurysms present about a third of the time in the MCA. They are associated with risk factors such as autosomal dominant polycystic kidney disease (ADKPKD), Ehlers-Danlos syndrome, cigarette smoking, hypertension, and age. Risk factors increase the probability of rupture and intracerebral hemorrhage. As previously discussed in the surgical considerations section, surgical resection and endovascular embolization are commonly used to treat saccular aneurysms in high-risk patients.