[2]
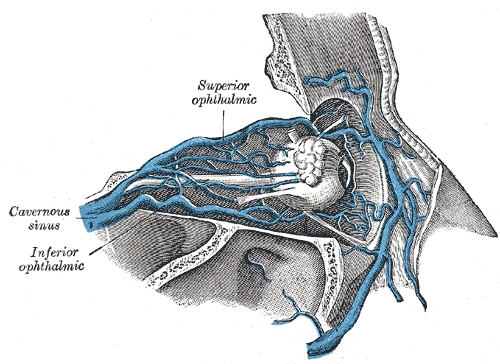
Jo A, Trauzettel H. [Topographic relationships of veins in the orbit]. Verhandlungen der Anatomischen Gesellschaft. 1974:68():539-48
[PubMed PMID: 4467623]
[3]
Brismar J. Orbital phlebography. III. Topography of intraorbital veins. Acta radiologica: diagnosis. 1974 Nov:15(6):577-94
[PubMed PMID: 4463695]
[4]
Cheung N, McNab AA. Venous anatomy of the orbit. Investigative ophthalmology & visual science. 2003 Mar:44(3):988-95
[PubMed PMID: 12601019]
[5]
Bergen MP. A literature review of the vascular system in the human orbit. Acta morphologica Neerlando-Scandinavica. 1981 Dec:19(4):273-305
[PubMed PMID: 7034482]
[6]
Brismar J. Orbital phlebography. II. Anatomy of superior ophthalmic vein and its tributaries. Acta radiologica: diagnosis. 1974 Sep:15(5):481-96
[PubMed PMID: 4451136]
[8]
Raybaud C. Normal and abnormal embryology and development of the intracranial vascular system. Neurosurgery clinics of North America. 2010 Jul:21(3):399-426. doi: 10.1016/j.nec.2010.03.011. Epub
[PubMed PMID: 20561492]
[9]
Mizutani K, Akiyama T, Yoshida K. The remnant of primary head sinus found in the case of dural arteriovenous fistula: A case report. Interventional neuroradiology : journal of peritherapeutic neuroradiology, surgical procedures and related neurosciences. 2016 Aug:22(4):452-6. doi: 10.1177/1591019916641903. Epub 2016 Apr 15
[PubMed PMID: 27084493]
Level 3 (low-level) evidence
[10]
Tanoue S, Kiyosue H, Okahara M, Sagara Y, Hori Y, Kashiwagi J, Mori H. Para-cavernous sinus venous structures: anatomic variations and pathologic conditions evaluated on fat-suppressed 3D fast gradient-echo MR images. AJNR. American journal of neuroradiology. 2006 May:27(5):1083-9
[PubMed PMID: 16687548]
[11]
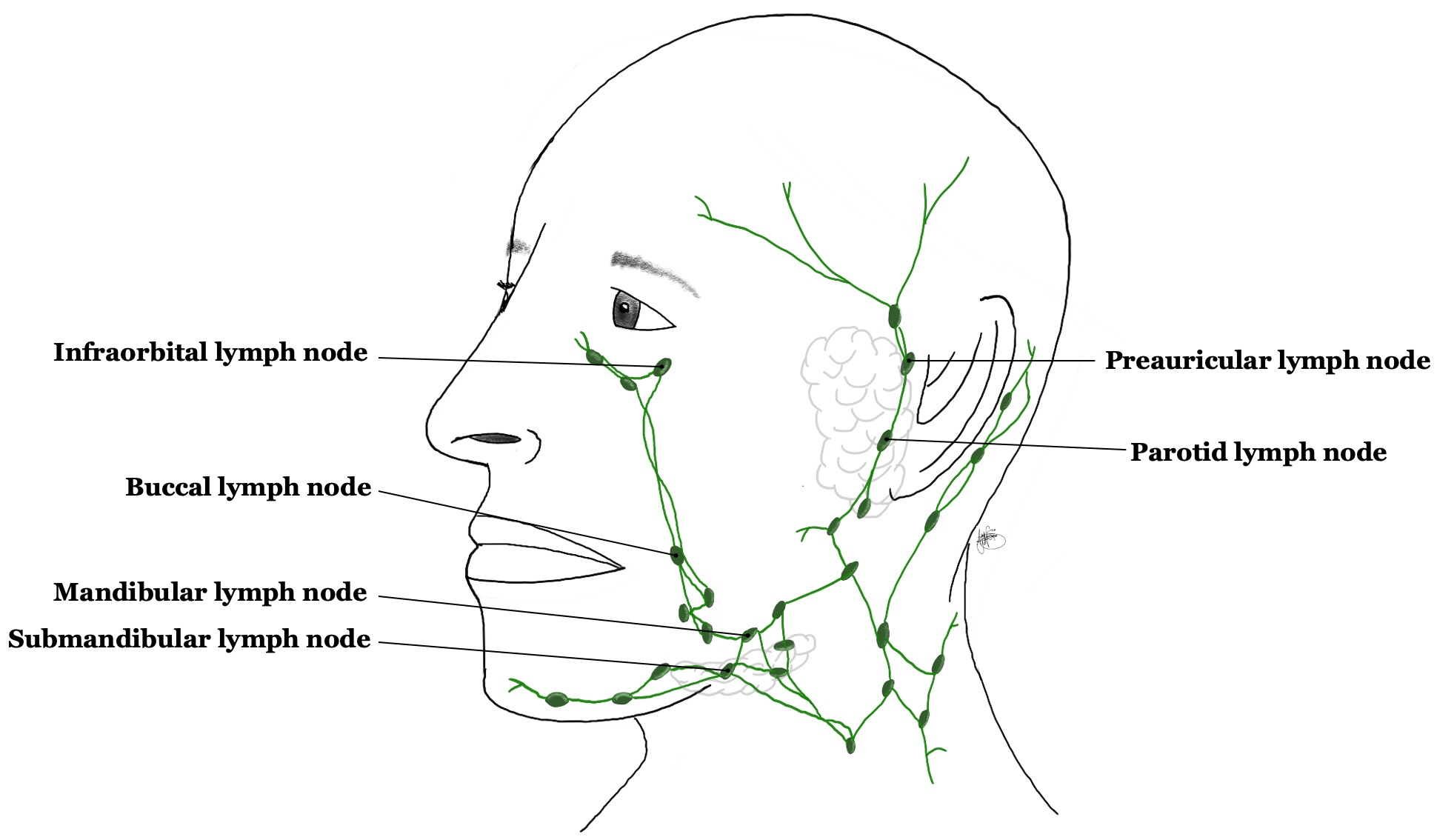
Tart RP, Mukherji SK, Avino AJ, Stringer SP, Mancuso AA. Facial lymph nodes: normal and abnormal CT appearance. Radiology. 1993 Sep:188(3):695-700
[PubMed PMID: 8351335]
[12]
Pan WR, Suami H, Taylor GI. Lymphatic drainage of the superficial tissues of the head and neck: anatomical study and clinical implications. Plastic and reconstructive surgery. 2008 May:121(5):1614-1624. doi: 10.1097/PRS.0b013e31816aa072. Epub
[PubMed PMID: 18453984]
[13]
Gausas RE, Gonnering RS, Lemke BN, Dortzbach RK, Sherman DD. Identification of human orbital lymphatics. Ophthalmic plastic and reconstructive surgery. 1999 Jul:15(4):252-9
[PubMed PMID: 10432521]
[15]
Shah A, Patel BC. Superior Ophthalmic Vein Cannulation for Carotid Cavernous Fistula. StatPearls. 2023 Jan:():
[PubMed PMID: 30725862]
[16]
Miller NR, Monsein LH, Debrun GM, Tamargo RJ, Nauta HJ. Treatment of carotid-cavernous sinus fistulas using a superior ophthalmic vein approach. Journal of neurosurgery. 1995 Nov:83(5):838-42
[PubMed PMID: 7472552]
[17]
Chalouhi N, Dumont AS, Tjoumakaris S, Gonzalez LF, Bilyk JR, Randazzo C, Hasan D, Dalyai RT, Rosenwasser R, Jabbour P. The superior ophthalmic vein approach for the treatment of carotid-cavernous fistulas: a novel technique using Onyx. Neurosurgical focus. 2012 May:32(5):E13. doi: 10.3171/2012.1.FOCUS123. Epub
[PubMed PMID: 22537122]
[18]
Cecchini MM, Levitt MR, Taneja M, Hallam DK, Ghodke BV. Embolization of carotid-cavernous fistula via direct percutaneous puncture of the inferior ophthalmic vein. Journal of neuroradiology = Journal de neuroradiologie. 2012 Jul:39(3):181-5. doi: 10.1016/j.neurad.2011.05.007. Epub 2011 Jul 23
[PubMed PMID: 21783255]
[19]
Morton RP, Tariq F, Levitt MR, Nerva JD, Mossa-Basha M, Sekhar LN, Kim LJ, Hallam DK, Ghodke BV. Radiographic and clinical outcomes in cavernous carotid fistula with special focus on alternative transvenous access techniques. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2015 May:22(5):859-64. doi: 10.1016/j.jocn.2014.11.006. Epub 2015 Feb 11
[PubMed PMID: 25682541]
Level 2 (mid-level) evidence
[20]
Matsubara S, Kazekawa K, Aikawa H, Onizuka M, Tsutsumi M, Ikou M, Kodama T, Nii K, Nagata S, Tanaka A. Direct superficial temporal vein approach for dural carotid cavernous fistula. Interventional neuroradiology : journal of peritherapeutic neuroradiology, surgical procedures and related neurosciences. 2007 Mar 15:13 Suppl 1(Suppl 1):64-7
[PubMed PMID: 20566079]
[21]
Kurata A, Suzuki S, Iwamoto K, Nakahara K, Inukai M, Niki J, Satou K, Yamada M, Fujii K, Kan S, Katsuta T. A new transvenous approach to the carotid-cavernous sinus via the inferior petrooccipital vein. Journal of neurosurgery. 2012 Mar:116(3):581-7. doi: 10.3171/2011.4.JNS102155. Epub 2011 Jun 17
[PubMed PMID: 21682561]
[22]
Zhu L, Liu B, Zhong J. Post-traumatic right carotid-cavernous fistula resulting in symptoms in the contralateral eye: a case report and literature review. BMC ophthalmology. 2018 Jul 25:18(1):183. doi: 10.1186/s12886-018-0863-6. Epub 2018 Jul 25
[PubMed PMID: 30045703]
Level 3 (low-level) evidence
[23]
Pappas A, Araque JM, Sarup V. Orbital Venous Varices: A Rare Bilateral Asymptomatic Presentation. Cureus. 2018 Sep 14:10(9):e3302. doi: 10.7759/cureus.3302. Epub 2018 Sep 14
[PubMed PMID: 30705795]
[24]
Lirng JF, Fuh JL, Wu ZA, Lu SR, Wang SJ. Diameter of the superior ophthalmic vein in relation to intracranial pressure. AJNR. American journal of neuroradiology. 2003 Apr:24(4):700-3
[PubMed PMID: 12695206]
[25]
Sorrentino D, Taubenslag KJ, Bodily LM, Duncan K, Stefko T, Yu JY. Superior ophthalmic vein thrombosis: A rare complication of Graves' orbitopathy. Orbit (Amsterdam, Netherlands). 2018 Jun:37(3):175-178. doi: 10.1080/01676830.2017.1383467. Epub 2017 Oct 20
[PubMed PMID: 29053044]
[26]
Monteiro ML, Moritz RB, Angotti Neto H, Benabou JE. Color Doppler imaging of the superior ophthalmic vein in patients with Graves' orbitopathy before and after treatment of congestive disease. Clinics (Sao Paulo, Brazil). 2011:66(8):1329-34
[PubMed PMID: 21915479]
[28]
Wilner HI, Gupta KL, Kelly JK. Orbital pseudotumor: association of orbital vein deformities and myositis. AJNR. American journal of neuroradiology. 1980 Jul-Aug:1(4):305-9
[PubMed PMID: 6779606]
[29]
Kwon JM, Lee SJ. Kissing Choroidal Detachment in a Patient with Idiopathic Orbital Inflammatory Syndrome. Korean journal of ophthalmology : KJO. 2019 Aug:33(4):386-388. doi: 10.3341/kjo.2018.0090. Epub
[PubMed PMID: 31389216]
[30]
Adam CR, Shields CL, Gutman J, Kim HJ, Hayek B, Shore JW, Braunstein A, Levin F, Winn BJ, Vrcek I, Mancini R, Linden C, Choe C, Gonzalez M, Altschul D, Ortega-Gutierrez S, Paramasivam S, Fifi JT, Berenstein A, Durairaj V, Shinder R. Dilated Superior Ophthalmic Vein: Clinical and Radiographic Features of 113 Cases. Ophthalmic plastic and reconstructive surgery. 2018 Jan/Feb:34(1):68-73. doi: 10.1097/IOP.0000000000000872. Epub
[PubMed PMID: 28141624]
Level 3 (low-level) evidence