Continuing Education Activity
Often considered a workhorse in facial reconstruction, the paramedian forehead flap is the most common interpolated flap harvested within the face. This flap has proved to be very useful and dependable for the reconstruction of the midface. One of the best applications of the paramedian forehead flap is in the reconstruction of the distal nose, where the sebaceous gland quality and tissue thickness closely resemble that of the forehead. This activity reviews the indications, contraindications, and techniques involved in using the paramedian forehead flap for facial reconstruction. This activity also highlights the role of the interprofessional team in the care of patients undergoing reconstructive surgery.
Objectives:
- Identify the critical anatomical structures involved in the elevation of the paramedian forehead flap.
- Outline the indications for paramedian forehead flap transfer.
- Describe the technique of transferring a paramedian forehead flap for nasal reconstruction.
- Review the complications associated with paramedian forehead flap transfer.
Introduction
Interpolated flaps, along with rotation, transposition, and island flaps, comprise the pivotal flap category of facial reconstruction techniques.[1][2][3] Interpolated flaps differ from other pivotal flaps, though, in that the base, or pedicle, of the flap is not contiguous with the defect and necessarily passes over the intervening tissue between the defect and the harvest site. Many surgeons would classify interpolated flaps as regional flaps rather than local flaps, given that the tissue used to reconstruct the defect when an interpolated flap is transferred is not originally adjacent to the defect.
While there are numerous interpolated flap options that may be employed in facial reconstruction - nasolabial flaps, temporoparietal fascia flaps, pericranial flaps, inferior turbinate flaps, facial artery musculomucosal flaps, and temporalis muscle flaps, among others - the paramedian forehead flap had remained a workhorse technique since World War I, even though its origins stretch back to at least 600 BC, when it was used for repair of nasal defects from punitive mutilation.[4][5] The sebaceous gland quality and thickness of central forehead tissue closely resemble those of the nose, and the flap's vascularity is highly reliable, which is why this technique has been chosen for nasal reconstruction so consistently throughout history.[6][7]
Utilization of the paramedian forehead flap in nasal reconstruction requires at least a two-stage procedure, with operations typically separated by three weeks, and some surgeons prefer to utilize a third stage to permit further refinement of the flap's contour.[8][9][10] Even though flap harvest necessarily leaves a vertical scar on the forehead, it is not always particularly conspicuous, and the ultimate cosmetic and functional outcomes tend to be very acceptable to patients and surgeons alike.
Anatomy and Physiology
When planning reconstructions involving a paramedian forehead flap, conceptualizing the forehead in three distinct regions is helpful. The forehead can be divided into central, lateral, and temporal zones, with differing blood vessels in each one. The central forehead tissue can be transferred as a paramedian forehead flap based upon a unilateral pedicle with enough skin to resurface an entire nose. The flap is perfused entirely by the supratrochlear artery and drained by its corresponding vein, thus giving the flap a specific axial blood supply rather than requiring it to rely upon random perfusion via the subdermal plexus.[11]
Perfusion of the forehead skin comes from the supratrochlear, supraorbital, superficial temporal, and dorsal nasal arteries (from the angular artery). The supratrochlear artery exits the orbit through the orbital septum and passes between the orbicularis oculi (superficially) and the corrugator supercilii (deeply). The supratrochlear artery arises from the internal carotid arterial system, exits the superior medial orbit between 1.7 and 2.2 cm lateral to the midline, and continues vertically, with the glabellar crease at the medial eyebrow approximating where the artery crosses the superior orbital rim. It follows, therefore, that the paramedian forehead flap should be designed to include the supratrochlear blood supply, including deep tissue at the most inferior 2 cm, where the vessels course deep to the frontalis muscle, and more superficial tissue superior to that point because the vessels run in a subdermal plane towards the vertex of the scalp.[12]
Indications
The most common indication for transfer of a paramedian forehead flap is the reconstruction of large nasal defects, although their use has been reported for periocular reconstruction as well.[13] There are many options for the repair of nasal wounds, but the defects best suited to reconstruction with paramedian forehead flaps are those that are larger than 1.5 to 2 cm in diameter with or without periosteal or perichondrial defects because smaller defects than these can often be addressed using single-stage techniques. Paramedian forehead flaps can provide enough skin to replace entire nasal subunits, which is useful when >50% of a subunit has been lost, and the best aesthetic outcome would be achieved by replacing the entire subunit instead of replacing only the missing tissue.[6] These flaps can also provide sufficient tissue to reconstruct rhinectomy defects and constitute a viable alternative to the use of free tissue transfer, such as radial forearm flaps. Some surgeons also perform complex, multi-stage, and multi-layer procedures in which paramedian forehead flaps are folded and/or wrapped around structural elements like bone, cartilage, or titanium plates to reconstruct total nasal defects.[14][15][16]
Contraindications
The paramedian forehead flap, as a workhorse flap, is commonly employed for the reconstruction of nasal defects in patients across the demographic spectrum. Nevertheless, there are a handful of situations in which the use of a paramedian forehead flap may not be ideal, including in patients who smoke (due to resulting small vessel vasculopathy), patients who will not accept a forehead scar, patients who have very low hairlines (and would therefore have substantial hair growth on the end of the flap), patients with wounds or lesions of the forehead (such as patients with multiple skin cancers), and patients with histories of forehead lacerations or prior surgery in the area that may have disrupted the supratrochlear blood supply.
Equipment
Equipment required for the first and second stages of paramedian forehead flap transfer is very similar and should include, at a minimum:
- Surgical marker
- Local anesthetic (1% lidocaine with 1:100,000 epinephrine or similar) and hypodermic syringe with a fine needle (27 or 30 gauge)
- Foil suture packet or similar material for use as a flap template
- Surgical sponges
- Doppler ultrasound probe
- Measuring tape or calipers
- #15 blade scalpel and #3 Bard-Parker handle
- Electrocautery (monopolar or bipolar)
- Dissecting scissors (Kaye blepharoplasty, strabismus, or small Metzenbaum)
- Forceps (Adson-Brown or similar)
- Needle driver (Halsey or similar)
- Suture scissors (Mayo or similar)
- Periosteal elevator (Freer, Cottle, or Joseph)
- Skin hooks
- Sutures for closing the flap harvest site and for insetting the flap
Personnel
Personnel requirements for paramedian forehead flap transfer are minimal, as the procedure can be performed under local anesthesia. In addition to a surgeon, a nurse, and an assistant/surgical technologist should be present. An anesthesia provider may be required for some patients as well.
Preparation
Patient Counseling
Patient education and counseling are key to a successful outcome, particularly because of the inconvenience and potential social consequences of the flap's pedicle between the initial and final stages of the procedure. Bruising, swelling, infection, and the appearance of the anticipated scar should be discussed. More time should be spent, however, attempting to prepare patients for the presence of the flap pedicle between the forehead and the nose, particularly if a delay occurs prior to dividing it. In addition, patients should be educated regarding wound care for the donor site and pedicle, avoidance of cigarette smoking, follow-up appointments, goals of reconstruction, and expectations for the final result.
Preoperative Preparation
Before surgery, measuring the defect and considering the length and width of the flap are of great importance. Determining the height of the anterior hairline and the amount of forehead laxity is also critical. In smokers, the supratrochlear artery should be traced up the entire forehead with a Doppler probe to rule out an obstruction in any segment of the vessel. Local anesthetic is injected, and the patient's face into the hairline is prepped with a surgical solution, usually povidone-iodine.
Technique or Treatment
Lidocaine 1% with 1:100,000 epinephrine is used alone or sometimes mixed with bupivacaine 0.25% in equal parts and injected deeply across the entire forehead. In addition, the dorsum of the nose and the base of the flap are injected. The margins of the nasal defect are debrided as necessary and made perpendicular to the wound bed with a scalpel, removing the remainder of the affected aesthetic subunit, if appropriate.
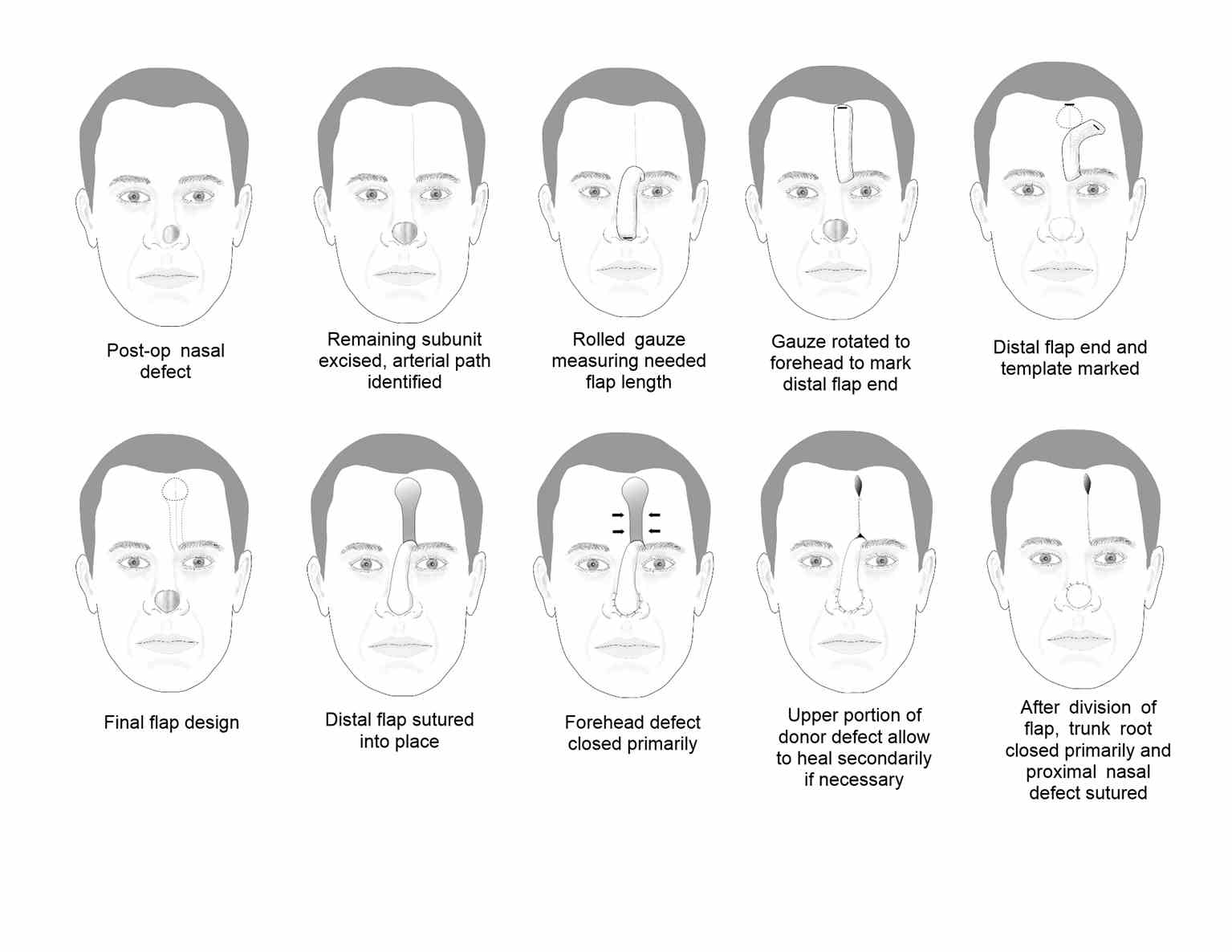
Flap Elevation and Inset
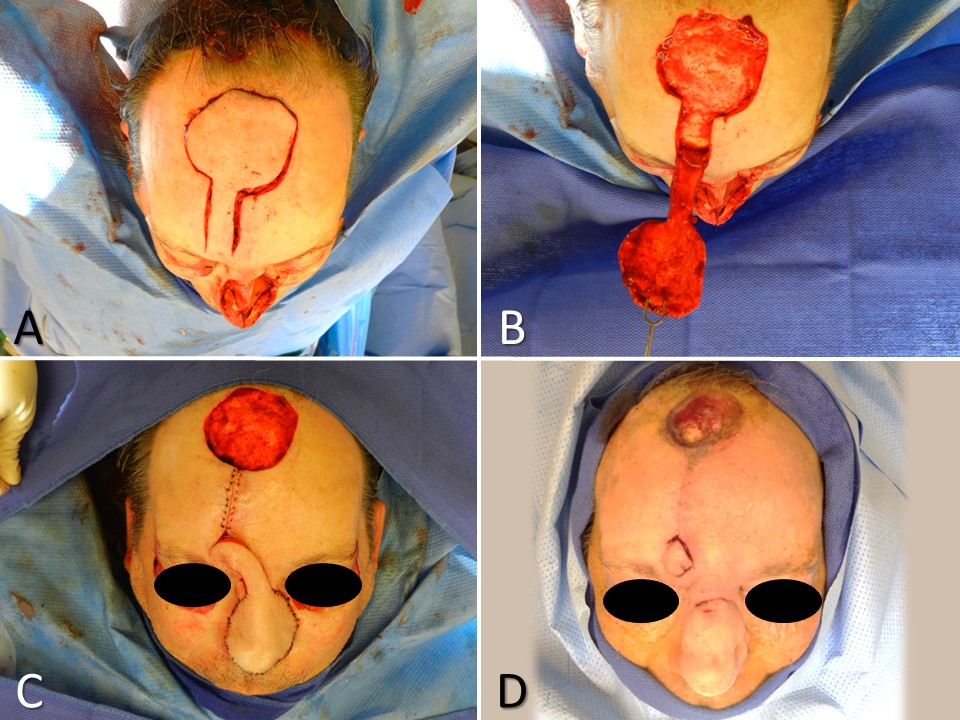
The flap is designed to incorporate the supratrochlear vessels within its base and pedicle using a combination of the surface landmarks described above and Doppler ultrasonography, if necessary. A wound template is made, often using the foil of a suture packet to shape the skin paddle at the distal end of the flap in the superior forehead. For patients with low anterior hairlines or those for whom the flap will be used in columellar reconstruction, the flap may be designed with a lateral curve to avoid the utilization of hair-bearing skin. If the flap extends into the hair-bearing scalp, dissection in a subcutaneous plane is often utilized to expose terminal hair bulbs and remove them. If the defect is large, elevation in a subcutaneous plane can be advantageous as well because it will expedite healing by secondary intention, as compared to a donor site wound that extends down to the galea or periosteum. On the other hand, if the defect is deep, elevating the flap in a submuscular/subgaleal plane will provide more bulk to the reconstruction.
In some cases, the flap may even be raised in continuity with a split-thickness calvarium if structural support is needed. The pedicle is typically elevated in a submuscular/subgaleal plane, in a strip approximately 1.5 to 2 cm wide, centered on the supratrochlear vessels. If the pedicle is too narrow, there is a risk of failing to include the supratrochlear vessels in their entirety, but if the pedicle is too wide, the risk of kinking it during rotation and compromising perfusion or venous drainage increases. For flap design purposes, the length of the pedicle may be estimated using a surgical sponge held fast at the medial eyebrow and rotating it down to the defect, which will give the surgeon an idea of how much length will be lost during the 180-degree flap rotation. In general, basing the flap contralateral to the larger part of the defect (if the defect is not perfectly midline and symmetric) will decrease the likelihood of kinking the pedicle and minimize the chances of flap compromise due to venous congestion or arterial insufficiency.
The plane of elevation deepens to a subperiosteal plane approximately 3 cm above the orbital rim to ensure the supratrochlear vessels, which are running deep to the frontalis muscle at this point, are incorporated into the flap. Careful undermining with direct visualization should take place if dissecting inferiorly beyond the orbital rim to improve flap length or mobility, as the supraorbital artery is also at risk of transection in this location. Once the flap is elevated, the nasal skin is undermined around the periphery of the defect, and the flap is rotated into place. Prior to suturing, the flap's thickness should be evaluated and adjusted as necessary to fit the defect.
At this point, if the defect extends close to the margin of the nasal ala, a rim graft of harvested septal or auricular cartilage may be placed to decrease the risk of postoperative alar notching. The flap is then sutured into place within the defect, taking care to evert the wound edges. Abutting the nasal dorsum, the proximal aspect of the flap is not sutured until pedicle division at a later date. Lastly, the donor site of the forehead is closed with submuscular/subgaleal undermining and multilayer suturing. The goal is to decrease tension and avoid forcing the donor site closed in order to prevent a widened scar and/or a postoperative headache. If part of the wound is closed via secondary intention, scar revision may be necessary at a later date.
Optionally, some surgeons place a skin graft on the exposed submuscular/subgaleal surface of the pedicle to promote hemostasis and prevent the patient from enduring three weeks of drainage. If a skin graft is not placed, petrolatum gauze may be wrapped around the pedicle instead.
Intermediate Stage
After three weeks, the skin flap may be gently elevated out of the defect and further thinned to improve contour.[17] Because the flap has already been delayed for three weeks, this recontouring is generally well tolerated. Three weeks after the intermediate stage, the pedicle may be divided.
Pedicle Division
The final stage of reconstruction is performed three weeks later. During this stage, the pedicle of the flap is divided, and unused portions are amputated and discarded, except for a triangle of skin that is used to restore the medial aspect of the eyebrow from which the flap was harvested. Meticulous repositioning of the base of the pedicle into the eyebrow is critical for optimizing the procedure's aesthetic outcome. It is essential to ensure that the triangle of the flap's base should not extend above the level of the eyebrow when it is inset back into the glabella; otherwise, it will look like a peninsula within the forehead. To prevent a trapdoor deformity, the brow is closed after wide-undermining and suturing.
Final Revisions
Further interventions should be deferred for several months to allow for the evolution of scarring, contraction, and maturity of the flap. Dermabrasion, contouring, and depilation may be performed at a later date.
Complications
In a 2019 study of 2,175 patients published by Chen et al., infection was the most common complication, affecting 2.9% of patients. Postoperative bleeding was the second most common complication, occurring in 1.4% of patients.[18] Bleeding is most likely to occur within the first 12 hours after surgery at the raw borders of the pedicle. Typically, careful cauterization intraoperatively will prevent this from happening. Likewise, as described above, placing a skin graft also decreases bleeding. Bleeding may also lead to the formation of hematomas, particularly under the distal portion of the flap; if feasible, these should be evacuated to help prevent infection and reduce pressure on the flap, thereby improving viability. While the robust axial blood supply of the paramedian forehead flap makes it prone to bleeding, it also greatly decreases the risk of flap ischemia and necrosis, which can nevertheless occur in <1% of patients.
Patients who use tobacco, have hypothyroidism or hypertension or also undergo auricular cartilage grafting or additional adjacent tissue transfer are more likely to require overnight admission, and patients with postoperative bleeding, neurological disorders, or alcohol use disorder are more likely to return to the emergency room or be readmitted to the hospital within 48 hours of surgery.[18]
Clinical Significance
The paramedian forehead flap is a staged, interpolated flap most commonly used in the reconstruction of larger defects of the nose. It is widely considered a workhorse in facial reconstruction and may also be employed outside the nose, e.g., in the periocular region.
Enhancing Healthcare Team Outcomes
Paramedian forehead flap transfer is a very versatile and reliable technique, most commonly utilized for nasofacial reconstruction. Primary care clinicians and dermatologists who have patients with nasal or periocular defects should refer these patients promptly to general plastic or facial plastic surgeons for definitive repair. Surgeons with high-volume local/regional facial flap reconstruction practices who are supported by experienced wound care nurses will provide the best care for these patients, with all involved parties keeping open communication lines in the event of any concerns or issues, working as a cohesive interprofessional healthcare team. Optimal outcomes will occur in healthy non-smokers who are well-educated about the perioperative process, postoperative recovery, potential complications, and expected final appearance of the flap.