Continuing Education Activity
Brow ptosis, the downward migration of periorbital soft tissues, is a common occurrence that steadily increases in persons 50 years and older. This condition may pose functional and cosmetic concerns for the patient. Depending on the severity, those affected may complain of issues such as visual field obstruction or an unappealing resting facial aesthetic. Many surgical and non-surgical techniques have been developed for managing this age-related process. One of these procedures is the direct brow lift. Clinicians specializing in facial rejuvenation techniques should thoroughly understand the medical and surgical management of brow ptosis. These techniques can help avoid complications, optimize the results, and better achieve the patient's goals.
Participants gain an in-depth understanding of brow ptosis, its prevalence, and its impact on patients' functional and cosmetic well-being, especially those older than 50. The focus is on the direct brow lift procedure, exploring its nuances, indications, and potential outcomes. The complexities of patient evaluation, surgical techniques, and postoperative care specific to periorbital aging are discussed. The course emphasizes the collaborative nature of addressing periorbital aging through the direct brow lift. The significance of an interprofessional team, including surgeons, nurses, anesthesiologists, and rehabilitation specialists, is emphasized. Collaborative learning experiences are highlighted to enhance competence in patient assessment, preoperative planning, intraoperative execution, and postoperative care.
Objectives:
Implement precise surgical techniques for direct brow lift procedures, demonstrating proficiency in tissue manipulation, fixation methods, and incision placement to achieve desired aesthetic and functional improvements.
Screen patients for suitability for a direct brow lift, assessing their medical history, expectations, and potential contraindications, ensuring optimal patient selection.
Communicate effectively with patients, addressing their concerns, managing expectations, and providing post-operative care instructions to enhance satisfaction and recovery.
Collaborate with interdisciplinary teams involving ophthalmologists, anesthesiologists, and nursing staff for comprehensive pre-operative assessment, intra-operative support, and post-operative care coordination.
Introduction
The periorbital region, including the eyebrows and upper and lower eyelids, undergoes predictable changes during aging.[1] With advancing age, the brow descends relative to the supraorbital rim, often resulting in dermatochalasis. Commonly, this presents as hooding of the lateral eyelids but, in severe cases, may result in upper visual field obstruction.[2] Other less common causes of brow ptosis include facial paralysis and post-traumatic deformity. Various surgical options to reposition the brow exist, ranging from traditional open techniques to newer endoscopic approaches. Each technique has strengths and weaknesses, but no procedure has been proven superior in all clinical scenarios.[3]
In recent years, the focus of aesthetic surgery has shifted towards minimally invasive techniques, like endoscopic browlifting.[4] However, performing traditional open approaches is still essential for facial surgeons as these techniques offer the highest precision when repositioning the brow. This article discusses the details of one such open approach, the direct brow lift, and its significance in rejuvenating the upper third of the face.
Anatomy and Physiology
The upper third of the face exhibits many characteristic signs of aging, including:
- Horizontal midforehead lines, due to the vertical action of the frontalis muscle
- Fullness of the upper lateral eyelid, caused by the descent of the upper facial soft tissues and brow ptosis
- Vertical and oblique glabellar lines from the action of the corrugator supercilii and the depressor supercilii (ie, superomedial orbicularis oculi) muscles
- Horizontal glabellar and nasal root lines, due to the action of the procerus muscle [5]
Pertinent Anatomic Structures
- Layers of the forehead: The brow's skin is thicker than on the upper eyelid. The thickest part of the brow skin is towards the middle, near the glabella, which is highly sebaceous. Skin with high sebum secretion is more prone to scarring, so most surgeons try to avoid making a direct brow incision in this area whenever feasible. Beneath the skin lies subdermal fat, and beneath that is the muscular layer. The most superficial muscle is the procerus, with the corrugator underneath and the frontalis beneath that. The corrugator is deepest medially, where it originates on the frontal bone, and most superficial laterally, where it inserts into the dermis of the brow. Below the muscle is the periosteum, which adheres to the underlying calvarium.[6]
- Supratrochlear nerve: This nerve provides sensory innervation to the medial upper eyelid, glabella, and a small portion of the conjunctiva. The supratrochlear nerve courses through the corrugator muscle and is usually located 1 cm medial to the exit point of the supraorbital nerve or 1.7 cm lateral to the midline.[7]
- Supraorbital nerve: This nerve exits a notch or foramen roughly 2.7 cm lateral to the midline forehead between the mid pupillary line and the medial limbus. The supraorbital nerve further divides into deep and superficial branches that provide sensory innervation to the frontoparietal and upper eyelid skin, respectively.[7]
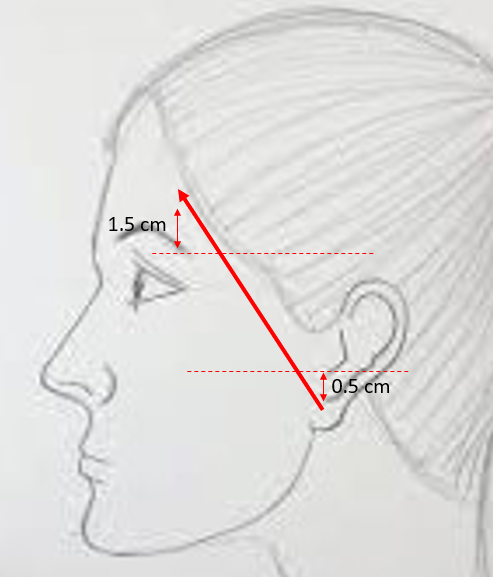
- Frontal branch of cranial nerve VII, facial nerve: This provides motor innervation to the forehead muscles (frontalis, corrugator supercilii, procerus) and the upper orbicularis oculi muscle. The path of this nerve may be approximated by the Pitanguy line, which is drawn from a point 0.5 cm inferior to the tragus to a point 1.5 cm superior to the lateral brow (see Image. Temporal Branch Course).[8]
Ideal Brow Location and Shape
- In women's classical ideal brow position, the brow forms an arch, with its highest point above the supraorbital rim, between the lateral limbus and the lateral canthus. The eyebrow should possess a defined and thicker appearance in the medial region, aligning with or just above the supraorbital rim. The brow should ascend above the rim, moving laterally and gradually tapering for a harmonious aesthetic.
- In men, the ideal brow is relatively flat and lies at the level of the supraorbital rim.
Indications
Indications for any Brow Lift Surgery
- Visual field obstruction
- Pseudo-blepharoptosis (excess upper eyelid skin prolapses over the lash line but no pathology of the eyelid musculature or levator aponeurosis is present—most often due to significant dermatochalasis that is exacerbated by brow ptosis)
- Brow ptosis
- Facial paralysis
- Brow asymmetry (often due to unilateral or asymmetric blepharoptosis)
- Deep forehead rhytids (ie, wrinkles)
- Glabellar lines
- Concerns regarding the perceived resting facial aesthetic (eg, an angry or tired look)[9]
Clinical Situations Favoring a Direct Brow Lift Approach
- Lack of forehead rhytids
- Unilateral facial paralysis (provides precise control of the elevation of each brow individually)
- Convex forehead craniofacial skeleton (limits endoscopic approach)
- Receding hairline or baldness
- Heavy eyebrows
- Prior eyebrow scar
- Patient preference [10]
The direct brow lift is increasingly used as a reconstructive technique and is less commonly performed in the cosmetic setting.[11] In contrast, indications for other brow lift approaches include:[1]
Endoscopic brow lift: multiple small incisions made within the frontal and temporal hairlines to permit the insertion of the endoscope and surgical instruments [4][12]
- Minimally invasive approach with a theoretically decreased risk of injury to neurovascular structures and shorter healing times
- Poorly suited for patients with receding hairlines or convex foreheads, which may restrict endoscopic visualization
- Requires fixation, typically with absorbable materials (eg, bioabsorbable anchors or sutures), to reposition and stabilize the forehead's soft tissues
- Only provides moderate brow elevation (several millimeters)[13]
Hairline brow lift: incision planned either within (trichophytic) or just in front (pretrichial) of the hairline.[14][15]
- Permits bilateral elevation of the periorbital soft tissues
- Useful in patients with elongated foreheads because this technique may be used to lower the patient's hairline
- May be combined with a hairline advancement
Coronal brow lift: incision made several centimeters behind the hairline
- Incision is completely hidden within the hair
- Should be avoided in patients with elongated foreheads because this technique will elevate the patient's existing hairline
- Avoid this procedure in bald patients, as this may leave an unsightly scar
Midforehead brow lift: incision placed in the middle of the forehead within an existing horizontal rhytid [16]
- Permits bilateral brow repositioning with a single incision
- Best suited for men with a receding hairline or baldness and deep forehead rhytids
- May excise multiple rhytids within the planned incision
- Less commonly performed due to visible scarring, even if the scar is aligned appropriately within a forehead rhytid
Contraindications
Contraindications to Brow Lift Surgery
- Body dysmorphic disorder
- History of blepharoplasty, especially recent (because the brow lift is more likely to cause lagophthalmos in these cases)
- Dry eye syndrome or history of decreased tear production (also due to risk of lagophthalmos and worsened xerophthalmia)[17]
Contraindications to the Direct Brow Lift Approach
- Unwillingness to accept a potentially visible facial scar
- Thin eyebrows
- Patient anatomy or expectations better suited for another surgical approach
Equipment
Preoperative
- Surgical marker
- Local anesthetic with hypodermic needle and syringe
- Surgical cleansing solution
- Eye protection in the form of a corneal shield or eye-taping
Intraoperative
- #15 blade scalpel
- Caliper
- Forceps (0.5 mm Castroviejo or Adson-Brown)
- Tissue scissors (Kaye blepharoplasty or strabismus scissors)
- Needle driver (Halsey or Castroviejo)
- Suture scissors (Mayo or iris)
- Electrocautery device
- Suture, per surgeon preference (eg, 4-0 poliglecaprone for deep layers, 6-0 polypropylene for skin)
Postoperative
- Antibiotic ointment
- External wound dressing, per surgeon preference
Personnel
The personnel included in the direct brow lift should include the following:
- Surgeon
- Surgical scrub technician
- Operating room nurse (circulator)
- An anesthesiologist or nurse anesthetist
(Note: The procedure may be performed under local anesthesia per surgeon and patient preferences.)
Preparation
The patient should be evaluated preoperatively by a medical professional who may risk-stratify and optimize the patient for general anesthesia if warranted.
A thorough preoperative physical examination should be performed with the patient upright. This includes assessment of brow position, visual fields, rhytids and scars, and facial nerve function. To determine the brow position at rest, take utmost care by having the patient close their eyes and fully relax the forehead. Many patients with significant brow ptosis cannot prevent frontalis muscle contraction when their eyes are open.
Preoperative photographs should be taken. Views include frontal in repose, frontal with eyebrows elevated, and profile in repose. If concurrent blepharoplasty is planned, additional views should be taken.
The patient should be appropriately counseled regarding the procedure's risks, benefits, and alternatives.
- Pertinent to this procedure, it is essential to mention improper brow position or asymmetry, incomplete eye closure, eye dryness, unsightly scarring, need for revisions, alopecia, paresthesias, and facial nerve injury. Other common risks associated with surgery include pain, bleeding, and infection.
- The patient's expectations should be discussed, and realistic goals must be set.
- Patients should be informed that direct brow lifting, like any facial rejuvenation surgery, will make the face appear younger than its stated age in the long term; however, the face will continue to age such that if the operation provides a 10-year rejuvenation to a 60-year-old patient, the patient will appear 50 initially, but will look 60 by the time they turn 70 and look 70 when they turn 80.
Patients may be advised to consider taking the herbal supplement Arnica montana during the perioperative period to minimize ecchymosis and edema.[18]
Patients who require additional simultaneous rejuvenating procedures such as blepharoplasty, fat transfer, and laser resurfacing should be identified and counseled.
Important landmarks must be identified.
- The supraorbital rim, supraorbital/supratrochlear neurovascular bundles, temporal line, sentinel vein, corrugator supercilii, procerus muscles, Pitanguy line, the position of the hairline, and the anticipated eyebrow shape and position [1]
General anesthesia may be used but is not necessary.
- Muscle paralytics are usually avoided to allow for intraoperative facial nerve monitoring if desired.
A single dose of intravenous antibiotics covering skin flora may be given preoperatively.
The supine surgical position is preferable.
Skin marking
- This starts with a fusiform beveled incision within the superior row of eyebrow hair. The upper incision is marked such that the height of the skin excised mirrors the desired brow elevation. The bulk of the elevation occurs laterally to restore the natural brow position.
Technique or Treatment
Successful completion of the direct brow lift requires that the surgeon have excellent soft-tissue handling techniques and a thorough understanding of facial anatomy.
The routine steps are outlined below.
- The patient is prepared for the surgical procedure once the proper preoperative checklist has been completed.
- The patient is positioned and draped in a standard sterile fashion. A safety checklist is followed, and a surgical time-out is observed.
- The planned amount of skin resected is verified and compared to the preoperative marking. Local anesthesia (1% lidocaine with 1 to 100,000 epinephrine with a maximum of 7 mg/kg of lidocaine) is injected into the planned surgical site. Suppose the patient is undergoing the procedure awake. In that case, adding 8.4% bicarbonate to the local anesthetic (10% of the volume of the lidocaine) will buffer the local anesthetic and reduce discomfort during injection.
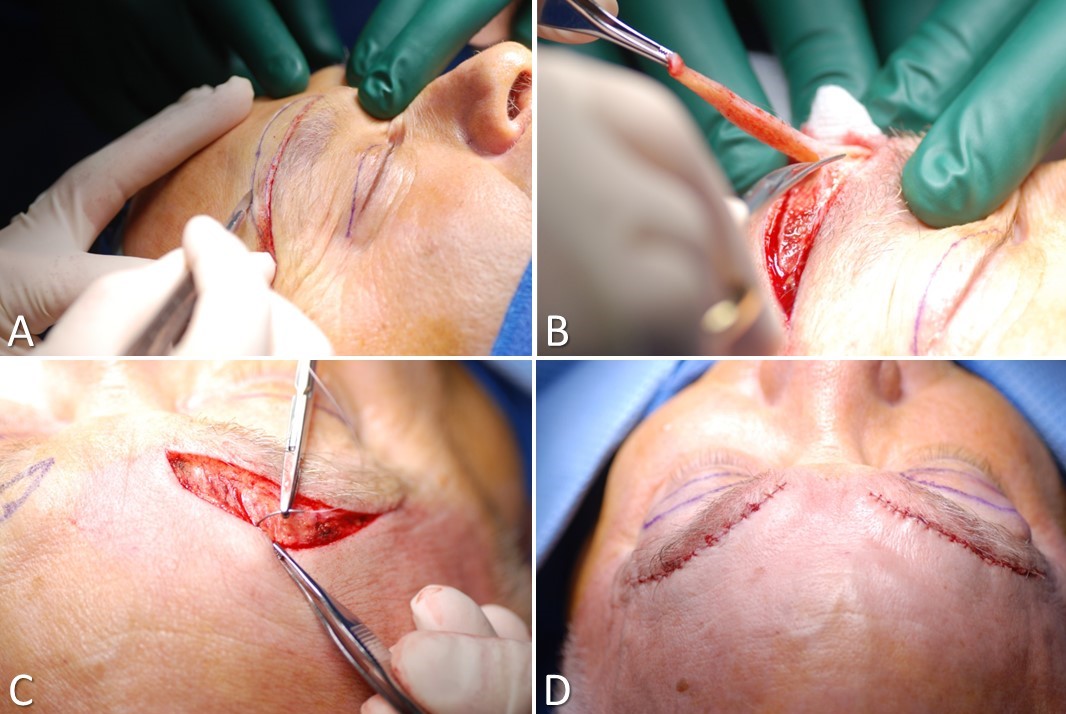
- A #15 blade scalpel creates a slightly beveled incision, so the final closure will naturally evert the skin edges (see Image. Direct Brow Lift). One should bevel the blade toward the hair follicle near the eyebrow to preserve the brow hairline.
- The skin and underlying soft tissue are resected while avoiding injury to underlying neurovascular structures and muscles (frontal and orbicularis oculi).
- The ptotic frontalis and orbicularis oculi muscles may be suspended to a more youthful position by superiorly anchoring them to the forehead periosteum. If prominent rhytids of the corrugator and procerus muscles need to be addressed, medial dissection may allow for sectioning these muscles.
- Hemostasis is achieved using pressure and limited electrocautery to avoid injury to the supraorbital and supratrochlear nerves.
- The deep layer of the wound is closed using absorbable sutures, commonly 4-0 or 5-0 poliglecaprone. The skin may then be closed using a 5-0 subcuticular or a running 6-0 cutaneous stitch using plain gut or polypropylene sutures.
- A dressing is placed per the surgeon's preference.
Complications
Although rare, complications may include:
- Wound infections
- Hematoma
- Brow asymmetry
- Forehead paresthesias
- Injury to the frontal branch of the facial nerve
- Unsightly scar formation
- Alopecia of the eyebrow
- Need for revision
- Overcorrection
- Eye dryness [19]
The meticulous surgical technique will minimize the appearance of the inevitable postoperative scar, particularly if the excision does not extend into the sebaceous skin of the glabella.
Clinical Significance
The direct brow lift represents an essential tool in the armamentarium of the aesthetic and reconstructive facial surgeon. Direct brow lifting provides precise repositioning of an asymmetric or ptotic brow, making it applicable in facial aging and facial paralysis.[20] The surgeon offering this technique should also be well-versed in the other approaches to brow lifting to advise and select the best plan for the individual patient. The outcomes can be very satisfactory in the hands of a knowledgeable and experienced surgeon.
Enhancing Healthcare Team Outcomes
A comprehensive approach is imperative to enhance patient-centered care, improve outcomes, ensure patient safety, and optimize team performance during a direct brow lift procedure. Initially, meticulous skills are required for identifying risk factors and conducting a thorough medical assessment. This involves collaboration among healthcare professionals, including a surgeon well-versed in facial aesthetics, medical optimization for anesthesia, and an ophthalmologist or optometrist evaluation to address potential visual concerns. Responsibility falls on a specialized preoperative, operative, and postoperative nurse who monitors patients and aids in care coordination and patient education. An interprofessional team comprising a facial surgeon, anesthesia provider, and operative nurse should conduct the procedure to achieve optimal outcomes. Subsequent close follow-up is crucial to monitor for potential complications, and patients should receive counseling on wound care and activity levels. Such interprofessional care is paramount in achieving the best results in facial reconstructive surgeries like direct brow lifting, embodying the principles of skill, strategy, ethics, responsibility, interprofessional communication, and care coordination.
Nursing, Allied Health, and Interprofessional Team Interventions
Recovery following direct brow lift surgery differs for each patient due to individual patients' functional and nutritional status. Meticulous local wound care ensures a healthy and clean healing environment. Blood thinners may be restarted on postoperative day 1. The patient should be counseled to avoid heavy lifting or straining until seen in follow-up to minimize edema and ecchymosis. When proper sterile technique is employed, postoperative antibiotics are not necessary. If utilized, permanent sutures for skin closure should be removed within 5 to 7 days, depending on the amount of wound tension present. Following surgery, the patient is typically seen regularly in the outpatient clinic until satisfactory healing has occurred.
Nursing, Allied Health, and Interprofessional Team Monitoring
Close follow-up will help identify any acute postoperative complications. Prompt identification and appropriate management will ensure optimal outcomes. Non-clinician staff should assist in monitoring, educating, and coordinating follow-up.