Continuing Education Activity
Granuloma annulare is a cutaneous granulomatous disease that is not caused by an infection. It is the most common non-infectious granulomatous disease. The disease is benign and often self-limited. Granuloma annulare usually presents as erythematous plaques or papules arranged in an annular configuration on the upper extremities. In addition to the more common presentation, termed localized granuloma annulare, other clinical variants of granuloma annulare include generalized, perforating, patch, and subcutaneous. Despite being a benign disease, it can be associated with more serious conditions such as HIV or malignancy. This activity explains when granuloma annulare should be considered in the differential diagnosis, articulates how to evaluate for this condition properly, and highlights the role of the interprofessional team in caring for patients with this condition.
Objectives:
- Describe the pathophysiology of granuloma annulare.
- Summarize the presentation of granuloma annulare.
- Outline the co-morbidities associated with granuloma annulare.
- Explain when granuloma annulare should be considered in the differential diagnosis, articulate how to properly evaluate for this condition, and highlight the role of the interprofessional team in caring for patients with this condition.
Introduction
Granuloma annulare (GA) is a cutaneous granulomatous disease of unknown etiology. It is the most common non-infectious granulomatous disease. The disease is benign and often self-limited. Granuloma annulare usually presents as erythematous plaques or papules arranged in an annular configuration on the upper extremities. In addition to the more common presentation, termed localized granuloma annulare, other clinical variants of granuloma annulare include generalized, perforating, patch, and subcutaneous.[1][2][3] Despite being a benign disease, it can be associated with more serious conditions such as HIV or malignancy.[4]
Etiology
The etiology and pathogenesis of granuloma annulare are largely unknown. However, the disease has been associated with diabetes mellitus, thyroid disease, mild trauma, hyperlipidemia, infections (Ebstein-Barr Virus, human immunodeficiency virus, varicella-zoster virus, tuberculosis), vaccines, malignancy, and certain drugs (TNF-alpha inhibitors). Despite the classic association with diabetes, the evidence is lacking to support a true association with diabetes. Experts believe that a clinician should screen for malignancy in a patient with granuloma annulare under the following circumstances: older age, atypical or widespread presentation, and recalcitrant disease. However, more evidence is needed to establish a true correlation between granuloma annulare and malignancy. Studies suggest that HIV patients are more likely to have generalized granuloma annulare. There are also reports of highly atypical presentations of granuloma annulare in patients with HIV. Antiretroviral drugs have been found to both improve and exacerbate HIV. Patients with new-onset granuloma annulare who have risk factors for HIV should be screened for HIV. Also, patients with the generalized type or perforating type of granuloma annulare should be screened for HIV.[5][6]
Epidemiology
The prevalence of granuloma annulare is estimated to be 0.1% to 0.4%, and the estimated incidence is 0.1% to 0.4%. Women are affected more commonly than men, and the disease can affect persons of any age. More than two-thirds of patients are 30 years of age or younger.
Pathophysiology
The etiology and pathogenesis of this disease are unknown. Some believe that granuloma annulare is caused by a delayed-type hypersensitivity reaction, more specifically a Th1 reaction involving IFN-gamma stimulating macrophages to release matrix metalloproteinases. This ultimately results in connective tissue degradation. Some studies provide support for this theory. For example, helper T cells have been found in samples of granuloma annulare lesions. Another study showed that a significant number of T cells in these lesions were CD3+ and had interferon-gamma receptors. It was also found that macrophages found in the lesions were differentiated to effector cells that expressed matrix metalloproteinases and tumor necrosis factor-alfa.
Impaired neutrophil chemotaxis has been found in patients with granuloma annulare. The authors of this study postulated that macrophages take over an inflammatory site because of the impaired neutrophil response, which leads to the granulomatous inflammation seen in granuloma annulare as opposed to a suppurative neutrophil type inflammation.
Histopathology
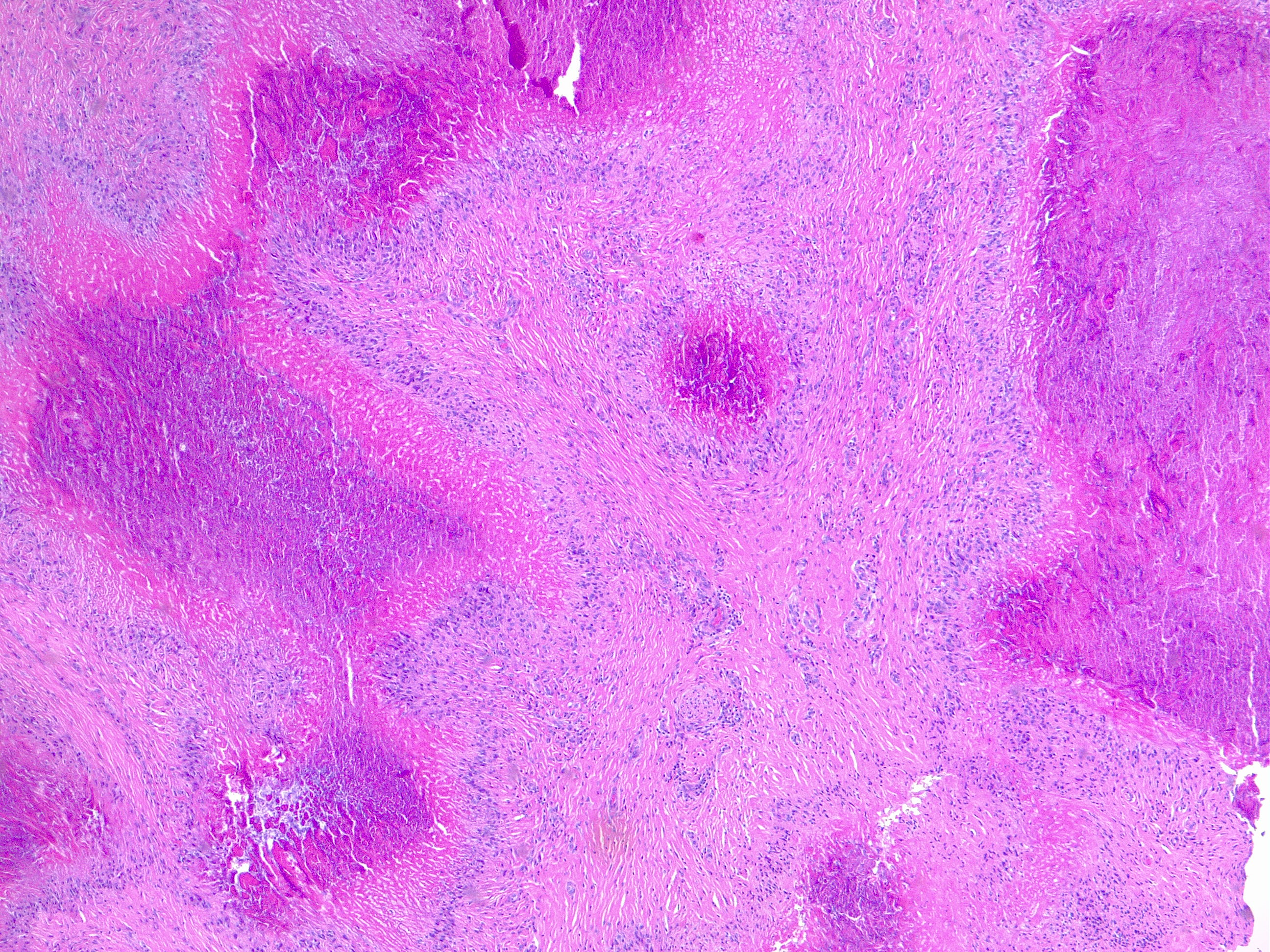
Histologically granuloma annulare is characterized by focal collagen degeneration, inflammation with interstitial histiocytes, and mucin deposition. Four different histopathological patterns are observed; interstitial (57.9%), palisaded granulomatous (26.3%), sarcoidal granulomatous, and mixed. The palisading pattern consists of a rim of histiocytes and lymphocytes that surround an area of necrobiotic collagen. The interstitial pattern consists of histiocytes scattered among bundles of collagen and blood vessels in the dermis. A patient may have more than one of the histopathologic subtypes.
History and Physical
Granuloma annulare is often located on the lateral and dorsal hands and feet in a ring-like or circinate configuration. There is usually no pruritus or other symptoms associated with the lesions. The localized variant is the most common subtype of granuloma annulare and represents approximately 75% of the reported cases of granuloma annulare.
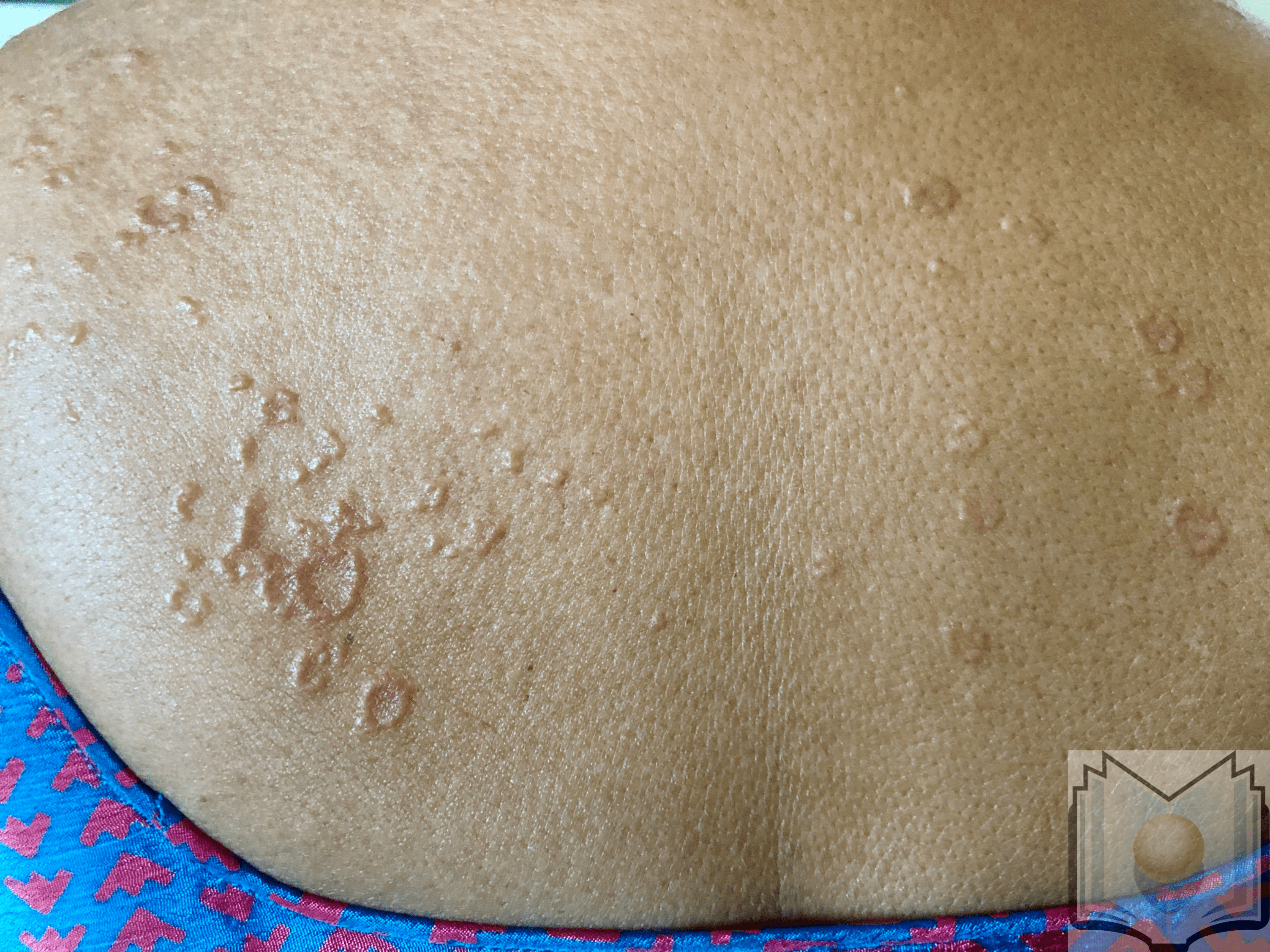
In addition to the localized variant, other clinical variants of granuloma annulare include generalized, perforating, patch, and subcutaneous. Generalized granuloma annulare presents with numerous flesh-colored papules in an annular configuration on the trunk and extremities. Unlike the classic presentation, these lesions are often pruritic. Up to 15% of granuloma annulare cases are of the generalized type. This subtype rarely resolves on its own and has a poor response to therapy.
Subcutaneous granuloma annulare presents with large nodules on the extremities. These nodules are sometimes called pseudorheumatoid nodules. Subcutaneous granuloma annulare is seen almost exclusively in children; the age range for developing the disease is about 1 to 14 years of age.
The patch variant of granuloma annulare presents with erythematous patches that may involve large areas of skin. There is some overlap between this subtype and reactive granulomatous eruptions; differentiating between the two is sometimes difficult. Perforating granuloma annulare presents with umbilicated papules. The lesions may be confined to the extremities or involve the trunk and the extremities. It is estimated that approximately half of the patients with the localized form of granuloma annulare will experience spontaneous remission within a 2-year period. A patient may have more than one of the subtypes of granuloma annulare.
Evaluation
Granuloma annulare is diagnosed by correlating clinical presentation (see above) with the histologic features found on biopsy (see above).
Treatment / Management
Although the lesions of granuloma annulare usually regress, they tend to recur. For this reason, and for cosmetic reasons, treatment sometimes is indicated. Physicians try many therapies, but there is little research-based evidence to support them. Further, in one study conducted with 67 granuloma annulare patients, researchers did not find a significant difference between the duration of lesions between untreated and treated patients.[7][5][8][9]
Despite the lack of evidence, experts agree that intralesional steroid injection is first-line therapy for lesions of granuloma annulare. There are reports of improvement after certain types of trauma to the lesions such as biopsy, pricking, incision, and cryotherapy. Phototherapy has shown promising results in some studies. There are reports of success with both excimer laser and pulsed dye laser. Hydroxychloroquine has shown success in a few small studies and reports. Although more evidence is needed to prove efficacy, some researchers believe that hydroxychloroquine should be first-line therapy for generalized granuloma annulare. Tumor necrosis factor-alpha inhibitors have shown efficacy in treating generalized and recalcitrant granuloma annulare. However, as mentioned above, there are reports of TNF-alpha inhibitors triggering or exacerbating the disease, so more research is needed to weigh the risks and the benefits of using TNF-alpha inhibitors to treat this disease. Physicians have also tried surgical excision, but lesions tend to recur.
In addition to the therapy mentioned above, vitamin E, isotretinoin, tetracyclines, intralesional interferons, topical imiquimod, niacinamide, oral calcitriol, dapsone, hydroxyurea, topical tacrolimus, clofazimine, and rifampin have been tried and reported to be effective in small studies.
Differential Diagnosis
- Actinic granuloma annulare
- Erythema annulare centrifugum
- Elastosis perforans serpiginosa
- Necrobiosis lipoidica diabeticorum
- Perforating granuloma annulare
- Subcutaneous granuloma annulare
Prognosis
Granuloma annulare is a benign, often self-limiting condition. Lesions can disappear spontaneously without sequelae, typically within several months to years. There is no satisfactory treatment for GA, but since the lesions are usually asymptomatic, watchful waiting is often acceptable.
For most patients, the condition disappears within a few years. It tends to be more persistent when it spreads to other areas (generalized form) than when it is only in one location (localized form).
Complications
Granuloma annulare is a benign, often self-limiting condition.
Deterrence and Patient Education
There is not much that patients can do to influence the course of granuloma annulare. No evidence exists showing diet to influence the condition. Patients can use skin camouflage to conceal affected areas.
Pearls and Other Issues
More research is needed to better determine the epidemiology, disease associations, pathophysiology, and treatment of this disease.
Enhancing Healthcare Team Outcomes
Patients with granuloma annulare may present to their primary care provider, internist, or dermatologist. The key thing to know is that this skin lesion is benign and can spontaneously regress. Most cases do not require any treatment. However, patients do seek treatment for cosmesis. Unfortunately, despite the availability of dozens of treatments, none works with any reliability or consistency; recurrences are common with all treatments.[10][11]