Continuing Education Activity
Confluent and reticulated papillomatosis (CRP), also known as Gougerot-Carteaud syndrome, is caused by disordered keratinization. It presents with asymptomatic hyperpigmented papules that can coalesce into plaques and are typically located on the upper trunk and neck of teens and young adults. The cause of confluent and reticulated papillomatosis is controversial. Historically, Malassezia furfur was thought to be the cause of the disease, but studies have since shown that patients with confluent and reticulated papillomatosis are not always colonized with Malassezia furfur. The current theory is infection with Dietzia papillomatosis, a gram-positive aerobic actinomycete. Other proposed causes include diabetes, obesity, ultraviolet light exposure, amyloidosis, and overexpression of keratin-16. First-line treatment is minocycline. Papules can take 12 to 39 months to resolve and have a recurrence rate of 13.8 to 15.4 percent. This activity reviews the evaluation and management of confluent and reticulated papillomatosis and highlights the role of interprofessional team members in collaborating to provide well-coordinated care and enhance outcomes for affected patients.
Objectives:
- Identify the clinical features of confluent and reticulated papillomatosis.
- Review the treatment options available for confluent and reticulated papillomatosis.
- Describe the natural course of confluent and reticulated papillomatosis.
- Outline a structured interprofessional team approach to provide effective care to and appropriate surveillance of patients with confluent and reticulated papillomatosis.
Introduction
Confluent and reticulated papillomatosis (CRP) is a condition due to disordered keratinization. The disease was originally described by Gougerot and Carteaud and is also called Gougerot-Carteaud syndrome. Confluent and reticulated papillomatosis presents as asymptomatic hyperpigmented papules, that can coalesce into plaques, located on the upper trunk and neck in teens and young adults. The cause of confluent and reticulated papillomatosis has been under debate. Malassezia furfur infection was thought to be the cause of the disease, but studies have shown that patients with confluent and reticulated papillomatosis are not always colonized with the yeast. The current theory is infection with Dietzia papillomatosis, a gram-positive aerobic actinomycete. Other possible causes for confluent and reticulated papillomatosis include diabetes, obesity, ultraviolet (UV) light, amyloidosis, and overexpression of keratin-16 (K16). First-line treatment is minocycline. The papules can take 12 to 39 months to resolve. There is a recurrence rate of 13.8% to 15.4%.[1][2][3]
Etiology
Confluent and reticulated papillomatosis was primarily thought to be caused by Malassezia furfur. Still, studies have been inconsistent with the detection of the yeast in patients with confluent and reticulated papillomatosis. The current infectious theory is that confluent and reticulated papillomatosis is caused by bacteria, Dietzia papillomatosis, anaerobic gram-positive coccus/rod actinomycete. There are noninfectious causes of confluent and reticulated papillomatosis, including diabetes, obesity, ultraviolet light, amyloidosis, and K16 mutation. There is an association between confluent and reticulated papillomatosis, diabetes mellitus, and obesity because hyperinsulinemia has mitogenic and antiapoptotic effects. Increased levels of insulin activate insulin-like growth factor 1, tyrosine kinase receptor superfamily, epidermal growth factor, and fibroblast growth factor and induce epidermal proliferation. Changes in confluent and reticulated papillomatosis with changing weight and diabetes control support this theory. UV light can induce confluent and reticulated papillomatosis because it has an effect on melanogenesis and can cause transient epidermal hyperplasia. Amyloid deposits have been found in some patients with confluent and reticulated papillomatosis, suggesting amyloidosis as a cause. Familial cases of confluent and reticulated papillomatosis could be due to overexpression of keratin-16.[4][5][6][7]
Epidemiology
Confluent and reticulated papillomatosis is reported to occur in different geographic areas and regions. It has a higher frequency in Caucasians. The Mayo Clinic conducted a study between 1972 and 2003 with 39 patients diagnosed with confluent and reticulated papillomatosis and determined the mean age of occurrence to be 15 years old with a range of 8 to 32 years and a male predilection of 1.4:1. A Japanese study had similar findings with a mean age of 17 years old and a range of 3 to 30 years and a slight male predilection. A Singaporean study reported a mean age of onset of 29 years old with a range of 16 to 55 years and a male bias of 2.6:1.
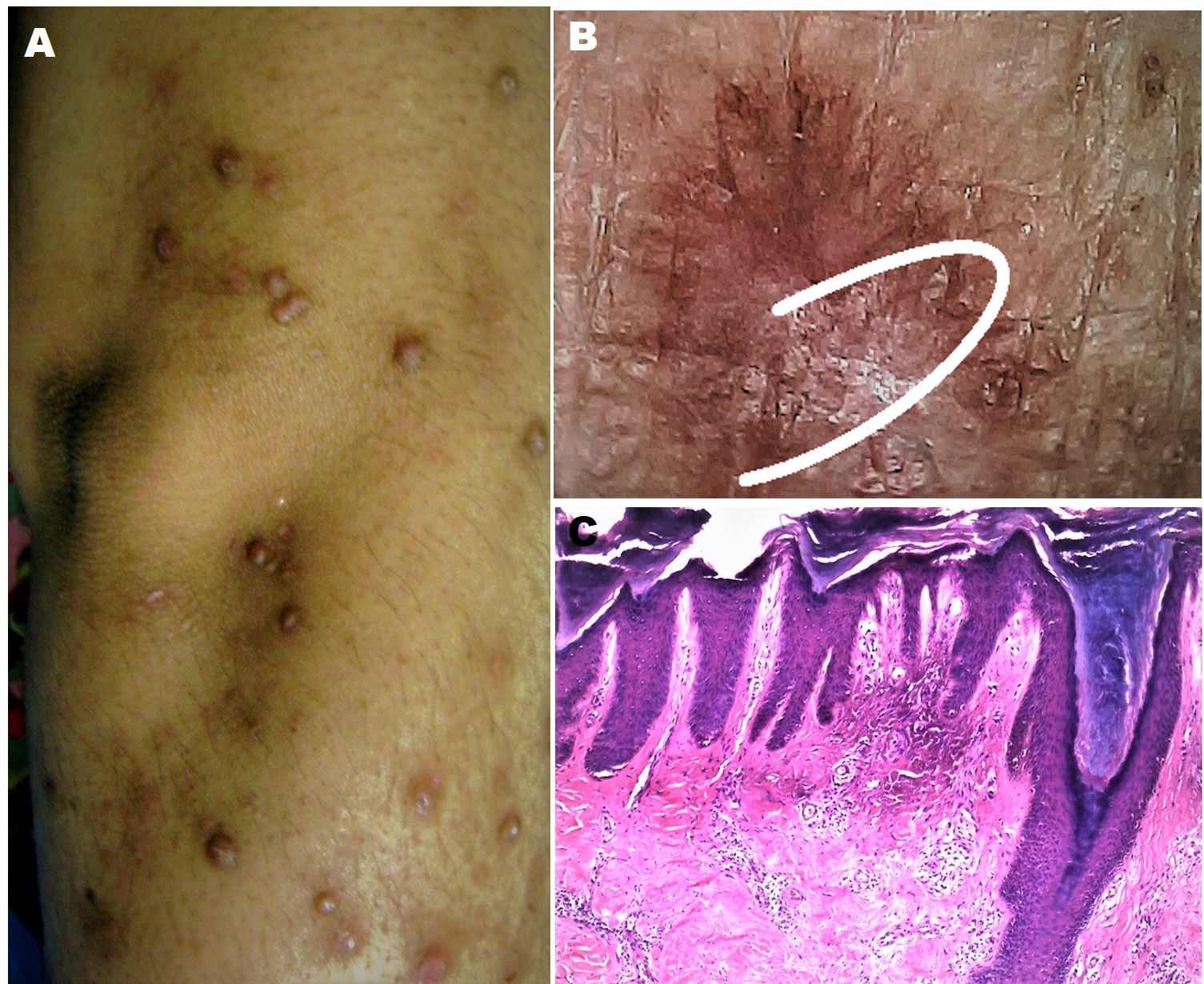
Histopathology
The diagnosis of confluent and reticulated papillomatosis is clinical, but a skin biopsy can be performed to rule out other diseases. Findings on histopathology include:
- Hyperkeratosis
- Papillomatosis
- Focal acanthosis
- Increased melanin pigmentation and melanosomes
History and Physical
Confluent and reticulated papillomatosis is mostly asymptomatic but can present with some pruritus. The disease is limited to the skin and presents as multiple 5 mm brown to hyperpigmented macules and papules in the center that can coalesce to form plaques with reticulation in the periphery. There can be some velvety or warty changes. The papules have epidermal changes, including scaling, hyperkeratosis, and/or atrophy. Confluent and reticulated papillomatosis most commonly occurs on the upper trunk and axilla. It can also occur on the shoulders, arms, antecubital and popliteal fossas and can rarely occur on the forehead.
Evaluation
Diagnosis is clinical. A skin biopsy can be performed to rule out other disorders. Dermoscopic evaluation will show brown pigmentation with white scales and a pattern of sulci and gyri.
Davis et al. proposed five criteria for the diagnosis of confluent and reticulated papillomatosis.
- Clinical findings of scaling brown macules and patches, part of which appear reticulated and papillomatous
- Involvement of the upper trunk and neck
- Fungal staining is negative for fungus
- No response to antifungal treatment
- Excellent response to minocycline
Jo et al. in 2014 proposed a change to the criteria.
- Scaly brown macules and patches with some appearing reticulated and papillomatous
- Involvement of the upper trunk, neck, or flexural areas
- Negative fungal staining or no response to antifungal treatment
- Excellent response to antibiotics
Differential diagnoses to consider are acanthosis nigricans, tinea versicolor, Dowling-Degos disease, Galli-Galli disease, dyskeratosis congenita, prurigo pigmentosa, terra firma-forme dermatosis, and Darier disease.
Treatment / Management
The main treatment options for confluent and reticulated papillomatosis are antimicrobials. Confluent and reticulated papillomatosis is usually asymptomatic. Treatment can help with emotional distress and cosmetic appearance. [8]
Antibiotics
First-line treatment is oral minocycline. Minocycline 50 mg twice a day for six weeks produces a good response with minimal side effects. Possible side effects include drug-induced hypersensitivity, drug-induced lupus, pigment changes, and vestibular toxicity. It is a category D medication and is not recommended in pregnancy. Azithromycin is a good alternative and can be used in pregnancy because of its category B rating. Azithromycin 500 mg once a day for two weeks and azithromycin 500 mg three times a week for three weeks can improve the appearance of confluent and reticulated papillomatosis. Oral clarithromycin 500 mg once a day for five weeks and erythromycin 1000 mg daily for six weeks have been shown to produce a good response. These antibiotics are effective because they are antibacterial and anti-inflammatory. The anti-inflammatory response of tetracyclines is due to their inhibition metalloproteinases, hydrolases, phospholipase A2, TNF-a, IL-1B, and IL-6. Macrolides work through inhibiting IL-8 and decreasing neutrophil oxidative burst.
Antifungals
- Acanthosis nigricans
- Achlorydria
- Dermatopathia pigmentosaa reticularis
- Epidermal nevus syndrome
- Epidermodysplasia Verruciformis
- Keratosis folicularis
- Pityriasis rubra pilaris
- Pseudoatrophoderma colli
- Seborrheic keratosis
- Syringoma
The use of antifungals is due in large part to the previous theory that Malassezia furfur causes confluent and reticulated papillomatosis. Topical selenium sulfide applied once a day for three weeks and then once a week for another three weeks produced a good response, but this could be due to its keratolytic properties. Other antifungals, such as ketoconazole, tolnaftate, and itraconazole, have worked, but recurrences were common.
Topical therapy and other treatments
Systemic retinoids, like isotretinoin and etretinate, have shown to be effective, but minocycline and azithromycin are safer and are preferred. Topical therapies such as topical retinoids, urea, calcipotriol, and tacrolimus have been successful. Ozdemir et al. reported a case of a patient with polycystic ovarian syndrome (PCOS) and confluent and reticulated papillomatosis that was treated successfully with oral contraceptives that contained drospirenone.
Differential Diagnosis
- Dermatopathia pigmentosa reticularis
- Epidermodysplasia verruciformis
Enhancing Healthcare Team Outcomes
Primary care providers and mid-levels are often the first to see patients with skin problems. In some cases, the diagnosis may be difficult. In such cases, a referral to a dermatologist is recommended. Nurse practitioner dermatology and specialty-trained dermatology nurses are involved in the diagnosis, follow up, and patient education. Pharmacists review presciptions, check for drug-drug interactions, and also education Confluent and reticulated papillomatosis is usually asymptomatic. When confluent and reticulated papillomatosis is diagnosed, the initial treatment is with antimicrobials. Treatment can help with emotional distress and cosmetic appearance. Patients should be advised to keep the skin moisturized and avoid prolonged exposure to the sun. [Level V]