Introduction
Glomerular filtration rate (GFR) represents the flow of plasma from the glomerulus into Bowman’s space over a specified period and is the chief measure of kidney function. The kidneys receive 20% to 25% of the cardiac output (about 1.0 to 1.1 liters per minute) with the blood entering individual glomerular tufts via the afferent arteriole and exiting through the efferent arteriole. Of this renal blood flow (RBF), only the plasma can cross the structures comprising the glomerulus. Thus, the renal plasma flow (RPF) is a more accurate expression and is calculated as follows: RBF*(1-Hct)
The RPF is approximately 600 to 720 ml per minute. Within the plasma, organic and inorganic solutes are freely filtered- meaning that they can be found in the ultrafiltrate (the fluid in Bowman’s space) and plasma at the same concentrations. GFR is approximately 120 ml per min (180 L per day). Average urine output, on the other hand, averages only about 1.5 L daily. The reabsorption of 178.5 L requires a sophisticated tubular network.[1][2][3]
Issues of Concern
The structure of the glomerulus exerts both size and charge constraints over what will pass through. The endothelium of fenestrated capillaries permits molecules of less than 70 nM to pass through. The basement membrane also restricts by size (approximately 1 kDa) and by charge, since the negative charge of basement membrane protein repels other proteins but favors filtration of cations. Finally, podocyte food processes on the visceral layer also size selects by about 14 nM.
The forces that govern filtration in the glomerular capillaries are the same as any capillary bed. Capillary hydrostatic pressure (Pc) and Bowman’s space oncotic pressure (πi) favor filtration into the tubule, and Bowman’s space hydrostatic pressure (Pi) and capillary-oncotic pressure (πc) oppose filtration. These terms are expressed together in the Starling force’s law equation, as a measure of J (flow):
- J = Kf ([Pc-Pi] - σ [πc - πi])
Where Kf is the filtration coefficient, and σ is the reflection coefficient, both inherent and fixed values of the epithelium. For the kidney, flow (J) is positive, favoring filtration, meaning that plasma flows from higher hydrostatic pressure in the capillary to lower hydrostatic pressure in the tubular space, despite the unfavorable oncotic gradient (there is higher protein concentration in the capillary). In theory, therefore, GFR is highly dependent on hydrostatic pressure.
However, GFR is tightly regulated through several mechanisms. Firstly, RBF is relatively constant over a wide range of mean arterial pressures (MAP), through what is termed the myogenic response. An increase in hydrostatic pressure in the afferent arteriole stretches vascular smooth muscle, activating inward directed ion channels, leading to depolarization and contraction. This prevents pathologic increases in RBF that would damage the kidney. Notably, this is a localized effect, independent of autonomic regulation (as is the case for autoregulation in other organs). Falling blood pressure does the opposite: dilate the afferent arteriole and preserve blood flow to the kidney. Secondly, the renin-angiotensin-aldosterone system acts to preserve GFR. The juxtaglomerular cells in the afferent arteriole release renin in response to decreased stretch. Circulating renin activates liver-synthesized angiotensinogen to angiotensin I, which is further acted upon by angiotensin converting enzyme in the lung to the active angiotensin II, a potent vasoconstrictor. Angiotensin II raises systemic blood pressure and stimulates the release of aldosterone, which promotes sodium retention/potassium secretion and further increases in blood pressure, in both cases preserving renal perfusion and maintaining GFR. The third mechanism is tubuloglomerular feedback. The macula densa in the thick ascending limb senses an increase in GFR through increased delivery of electrolytes. The increased flow leads to an increased intracellular Cl concentration (sensed by Na-K-Cl transporter), depolarizing the cell, and leading to the release of ATP, adenosine, and thromboxane. These paracrine mediators contract nearby smooth muscle cells in the afferent arteriole to reduce RBF and, thus, return GFR to normal. The macula densa can also independently stimulate the juxtaglomerular cells to release renin, activating the RAAS. We know that this transporter is implicated because the effect can be attenuated by loop diuretics that block the Na-K-Cl channel.
Clearance is the virtual plasma volume from which a solute is removed per unit time, expressed in ml per minute. It can be calculated for any substance given steady-state, known concentrations as [urine concentration] x (urine flow rate) / [plasma concentration], or more simply, C = UV/P. Therefore, it is an indicator of GFR (also ml per minute) for solutes that are freely filtered (not size/charge restricted) and which are not significantly reabsorbed, secreted, synthesized or metabolized in the kidney. Experimentally, inulin, a plant polysaccharide that is indigestible and administered exogenously is used. This requires time to reach a steady state and is not feasible in the clinical setting. Practically, we use creatinine, a breakdown product of creatine phosphate in skeletal muscle. Under normal adult metabolism (catabolic and anabolic in equilibrium), a constant amount of creatinine is released. Under those conditions, any change in creatinine is due to changes in clearance (and therefore GFR). Nonrenal factors that influence the plasma creatinine are strenuous exercise, endogenous consumption (muscle-building supplements), rapid muscle growth, or injury to a skeletal muscle (rhabdomyolysis, burns). We standardize clearances by comparing them to inulin/creatinine which is assigned clearance of 1. Substances that are reabsorbed will have a clearance of less than 1, and those that are secreted will have a clearance greater than 1. We can use the clearance of another compound to look at renal plasma flow. Para-amino hippuric acid (PAH) is filtered and secreted such that, in one pass, it is entirely cleared by the kidney. Therefore, its clearance approximates RPF. We now have the required calculations to describe another measure of kidney function: filtration fraction (FF). This is the portion of plasma entering the kidney (RPF) that ends up as filtrate (GFR). FF = GFR / RPF and is approximately 20% for a healthy individual.
Clinical Significance
Changes in GFR are used to define and diagnose several pathologies. Acute kidney injury (AKI, previously acute renal failure) is an abrupt increase in serum creatinine (generally over days) and is largely reversible. Alternatively, chronic kidney disease is often irreversible damage and persistent over at least 3 months. Chronic kidney disease is staged as follows:
- Stage 1 normal, greater than 90 ml per minute
- Stage 2 mild, 60 to 89 ml per minute
- Stage 3a mild to moderate, 45 to 59 ml per minute
- Stage 3b moderate to severe, 30 to 44 ml per minute
- Stage 4 severe, 15 to 29 ml per minute
- Stage 5 failure, less than 15 ml per minute
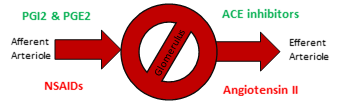
While many medications are eliminated renally and are therefore relevant to a discussion of kidney function, the mechanism of several of them directly affect GFR. NSAIDs and ACE inhibitors (or angiotensin receptor blockers) both decrease GFR by different mechanisms. NSAIDs inhibit prostaglandin synthesis. PGI2 and PGE2 normally dilate the afferent arteriole, so NSAIDs are afferent constrictors. Angiotensin II normally constricts the efferent arteriole, so ACE inhibitors (or angiotensin receptor blockers) dilate the afferent arteriole. Note that endogenously produced compounds (PGE2 and Angiotensin II) increase the GFR, and exogenous medications decrease the GFR (NSAIDS and ACEi or ARBs). This is why taking NSAIDs on ACEi (or ARB) is a relative contraindication, especially with other renally active drugs like diuretics.[4][5][6][7][8]