Continuing Education Activity
Arterial cannulation is a procedure frequently performed in acute and critical care settings. It serves as an invasive means to more accurately measure blood pressure and mean arterial pressure than non-invasive means. Artery cannulation gives precise measurements that allow for immediate recognition of alterations, thus allowing for quicker intervention and potential stabilization of a patient. This activity describes the technique and indications for arterial cannulation and highlights the role of the interprofessional team in ensuring safe arterial access.
Objectives:
- Identify the technique of inserting arterial lines.
- Describe the indications for inserting arterial lines.
- Recall the complications of arterial lines.
- Review the importance of improving care coordination among interprofessional team members to improve outcomes for patients needing arterial access.
Introduction
Arterial cannulation is a procedure frequently performed in acute and critical care settings. It serves as an invasive means to more accurately measure blood pressure and mean arterial pressure than non-invasive means. Artery cannulation gives precise measurements that allow for immediate recognition of alterations, thus allowing for quicker intervention and potential stabilization of a patient. In addition to accurate arterial pressures, arterial cannulation may also serve as a means to collect blood gas samples repetitively without requiring additional punctures and increasing the potential for injury. There are multiple sites for arterial cannulation including but not limited to radial, brachial, and femoral arteries. The radial artery is the most utilized for access in adults and pediatrics. Arterial cannulation is a relatively safe procedure that poses little risk of complication when performed by an appropriately skilled practitioner.[1][2][3][4]
There are several indications for which arterial cannulation may be considered. The most obvious being invasive blood pressure monitoring and accurate mean arterial pressures. Arterial cannulation may also be considered in patients who will require frequent arterial blood samples or in patients which non-invasive blood pressure monitoring is excluded such as those with large surface area burns, severe hypotension, multiple extremity fractures, or extreme obesity.
As in any procedure that has indications, there are also contraindications to arterial cannulation. One of the most common contraindications for arterial cannulation is anticoagulation, especially in those who have recently received thrombolytics for an acute infarct. Other contraindications include coagulopathy, arterial atherosclerosis, insufficient collateral perfusion, partial or full thickness burns over the cannulation site, synthetic arterial or vascular grafts, or infection at the proposed site of cannulation. Caution must be used if one chooses to proceed with arterial cannulation despite the posed contraindications. The procedure has been successfully performed in the presence of contraindications; however, it is not encouraged unless there are extenuating circumstances in which the practitioner feels the procedure is necessary. Absolute contraindications for arterial cannulation are absent pulse, Raynaud Syndrome, full thickness burns over the proposed site of cannulation, inadequate or interrupted circulation. Despite the list of contraindications, there is a less than one percent chance for major complications with arterial cannulation. A risk to benefit analysis should be performed in each patient prior to proceeding with arterial cannulation.
Anatomy and Physiology
With the radial and femoral arteries being the 2 most cannulated sites, we will explore the anatomical site where the 2 can be located and cannulated in detail.
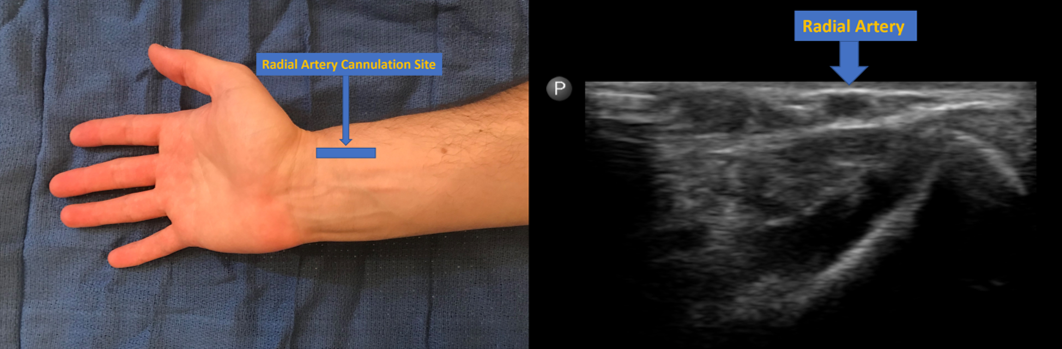
Radial artery: From the brachial artery, the radial artery originates in the cubital fossa and traverses the lateral aspect of the forearm. It supplies the palmar arches that provide adequate blood circulation to the hand. It is palpable at the wrist, proximal to the radial styloid or radial head and slightly lateral. The cannulation site should be at the very distal portion of the arm. The most frequent location for radial artery cannulation is at the proximal flexor crease of the wrist, 1 cm proximal to the styloid process.
Femoral artery: Originating at the inguinal ligament just off of the external iliac artery, lies the femoral artery. It continues posterior to the inguinal ligament, at the median between the anterior superior iliac spine and pubic tubercle. The femoral artery is situated medial to the nerve thus lateral to the vein. Due to the increased risk of bleeding as a result of increased diameter of the femoral artery in relation to the radial artery, the initial access site should be 2.5 cm distal to the inguinal ligament. This allows for suitable compression of the vessel if necessary. The femoral pulse should be easily identified with slight pressure placed median the distance between the anterior superior iliac spine and the symphysis pubis.
Indications
Indications for arterial cannulation include but are not limited to:
- Continuous blood pressure monitoring
- Continuous mean arterial pressure monitoring
- Frequent arterial blood gas specimens
- Frequent blood sampling for diagnostic testing
Contraindications
Strict Contraindications for arterial cannulation:
- Absent pulse at the anatomical location of the artery
- Raynaud syndrome
- Buerger disease (thromboangiitis obliterans)
- Poor perfusion of the appendage
Relative contraindications for arterial cannulation include but are not limited to:
- Coagulopathy (hypo or hypercoagulable states)
- Moderate to severe atherosclerosis
- Insufficient collateral flow
- Infection at the site of cannulation
- Second degree (partial thickness) or third-degree (full thickness) burns at the cannulation site
- Cannulation site within the proposed surgical field
- Artificial vascular graft in the area
Equipment
Equipment needed for successful arterial cannulation and catheter placement includes:
- Sterile gloves and drapes
- Skin prep solution such as povidone-iodine or chlorhexidine
- A 20-ga length appropriate catheter
- Five ml 1% lidocaine without epinephrine
- A 3 ml syringe with 25 ga or 27 ga needle for subcutaneous administration of lidocaine
- No. 11 blade scalpel
- A 4-0 nylon suture
- Sterile 4 x 4s
- Adhesive tape
- A 3-way stopcock
- Transducer kit
- Pressure tubing
- Size appropriate arm board (for radial artery access)
- Needle holder
- Intravenous (IV) tubing T-connector
Many kits are available specific to arterial cannulation that includes a catheter situated over a wire for fast and easy insertion. A 20-ga catheter is an acceptable size for older children and adults, a 22-ga catheter is preferred for pediatrics and infants. When planning for brachial or femoral artery cannulation, appropriate length catheters are necessary to ensure sufficient cannulation. The desired length of a brachial or femoral arterial catheter is 15 cm at a minimum.
Ultrasound guidance may also be used to help define the anatomy and visualize arterial cannulation.
Personnel
When preparing for arterial cannulation, it is important to have at least 1 other member of the healthcare team that is familiar with the process available to assist in the procedure. Appropriate personnel readily available to assist in the procedure will decrease the margin of error related to placement of supplies, securing the arterial catheter post cannulation, and connection of the pressure tubing to the catheter hub.
Preparation
After obtaining consent for the procedure or deeming it an emergency, the first step in preparing a patient for arterial cannulation is to place the area chosen for insertion in the appropriate position. For a radial artery cannulation, placing the hand palmer side-up with the wrist flexed approximately 45 degrees and supported by a gauze roll will allow for maximum access to the artery. Hyperflexing the wrist will potentially compress the artery thus making cannulation difficult or unsuccessful. It is recommended a Doppler be performed before radial artery cannulation. When accessing the femoral artery, it is suggested that the patient is in the supine position with the hip of the chosen side for cannulation slightly externally rotated. The artery should be palpable in the space between the pubic tubercle and the anterior superior iliac spine.
Technique or Treatment
The procedural approach should be decided upon before initiation of the procedure. The 2 commonly utilized techniques are the Seldinger technique, the most common, or the catheter-over-needle technique. The catheter-over-needle technique is basic and can be performed via accessing the artery with a needle that includes an integrated catheter that is easily advanced into the lumen of the vessel following arterial access. Once the artery has been accessed and the catheter placed in the lumen, the needle is completely removed leaving only the catheter in place. The catheter is then properly secured with nylon suture.
The Seldinger technique is performed by accessing the artery with a needle, feeding a guidewire through the lumen of the needle, and finally placing the catheter in the lumen of the artery by feeding it over the guidewire and removing the guidewire leaving only the catheter itself in place. The catheter is then secured with nylon suture. This is the recommended technique for arterial cannulation in an infant or child.
Ultrasound guidance may be utilized to assist in identifying the artery and also to visualize cannulation of the vessel.[5][6][7]
Complications
The most common complications with arterial cannulation are occlusion of the vessel, bleeding from the insertion site, or hematoma. All 3 of these complications can be effectively addressed with minimal effort. Proper attention to complications in a timely fashion can correct the issue and prevent further damage to the area. Less likely complications include, but are not limited to, infection, ischemic damage, compartment syndrome, nerve injury, or sepsis. When appropriate, aseptic technique is used when performing the arterial cannulation procedure, all of these complications are relatively rare.[8]
Clinical Significance
Arterial cannulation has become increasingly significant in the appropriate monitoring and stabilization of the critically ill patient. It allows for continuous monitoring of the patients hemodynamic status by revealing an accurate blood pressure reading as well as a mean arterial pressure. Both of these values, when monitored via the use of arterial cannulation, can depict a sudden change in the patient's condition allowing for more timely and effective intervention thus potentially improving patient outcomes. Arterial cannulation is quickly becoming standard in critical care areas when caring for specific patient populations that have the potential to decline rapidly if certain changes in hemodynamic status go unnoticed. With continued use and increasing comfort regarding arterial cannulation and monitoring, this procedure is sure to aid in improving patient outcomes and aid clinicians in the medical decision making process on a more frequent basis in the critical healthcare setting.
Enhancing Healthcare Team Outcomes
Arterial cannulation is freqently done in an ICU setting for monitoring of blood pressure. Anyone who performs arterial cannulation MUST be fully aware of the anatomy and potential complications. While arterial cannulation is only done by physicians, the care of patients is by ICU nurses. The insertion site must be monitored for bleeding, hematoma and signs of infection. In addition, the distal pulses in the extremity must be monitored. In general arterial lines should be discontinued as soon as hemodynamic stability is obtained.