[1]
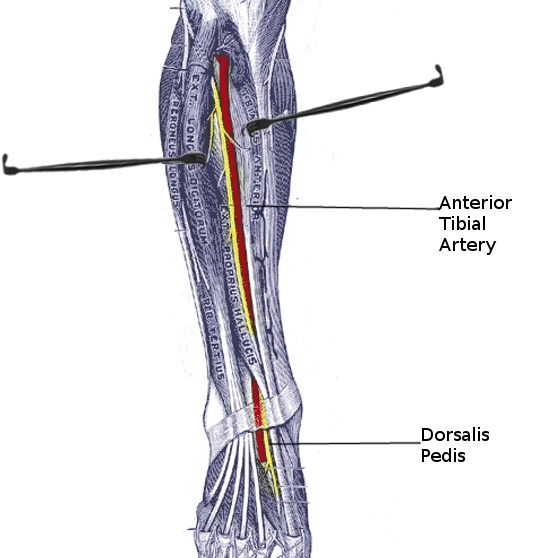
Mróz I, Kielczewski S, Pawlicki D, Kurzydło W, Bachul P, Konarska M, Bereza T, Walocha K, Kaythampillai LN, Depukat P, Pasternak A, Bonczar T, Chmielewski P, Mizia E, Skrzat J, Mazur M, Warchoł Ł, Tomaszewski K. Blood vessels of the shin - anterior tibial artery - anatomy and embryology - own studies and review of the literature. Folia medica Cracoviensia. 2016:56(1):33-47
[PubMed PMID: 27513837]
[2]
Chmielewski P, Warchoł Ł, Gala-Błądzińska A, Mróz I, Walocha J, Malczak M, Jaworek J, Mizia E, Walocha E, Depukat P, Bachul P, Bereza T, Kurzydło W, Gach-Kuniewicz B, Mazur M, Tomaszewski K. Blood vessels of the shin - posterior tibial artery - anatomy - own studies and review of the literature. Folia medica Cracoviensia. 2016:56(3):5-9
[PubMed PMID: 28275266]
[3]
Barham G, Clarke NM. Genetic regulation of embryological limb development with relation to congenital limb deformity in humans. Journal of children's orthopaedics. 2008 Feb:2(1):1-9. doi: 10.1007/s11832-008-0076-2. Epub 2008 Feb 7
[PubMed PMID: 19308596]
[4]
Kil SW, Jung GS. Anatomical variations of the popliteal artery and its tibial branches: analysis in 1242 extremities. Cardiovascular and interventional radiology. 2009 Mar:32(2):233-40. doi: 10.1007/s00270-008-9460-z. Epub 2008 Nov 4
[PubMed PMID: 18982387]
[5]
Olin JW, Sealove BA. Peripheral artery disease: current insight into the disease and its diagnosis and management. Mayo Clinic proceedings. 2010 Jul:85(7):678-92. doi: 10.4065/mcp.2010.0133. Epub
[PubMed PMID: 20592174]
[6]
Caetano AP, Gomes FV, Bilhim T, Coimbra É, Neves J. Percutaneous Mechanical Thrombectomy with Rotarex Using the Retrograde Posterior Tibial Artery Approach for Recanalization of Superficial Femoral Artery In-Stent Occlusion. Journal of vascular and interventional radiology : JVIR. 2019 Oct:30(10):1691-1693. doi: 10.1016/j.jvir.2018.12.027. Epub 2019 Apr 16
[PubMed PMID: 31003846]
[7]
Gür S, Oğuzkurt L, Gürel K, Tekbaş G, Önder H. US-guided retrograde tibial artery puncture for recanalization of complex infrainguinal arterial occlusions. Diagnostic and interventional radiology (Ankara, Turkey). 2013 Mar-Apr:19(2):134-40. doi: 10.4261/1305-3825.DIR.6122-12.1. Epub
[PubMed PMID: 23266971]
[8]
Via AG, Oliva F, Spoliti M, Maffulli N. Acute compartment syndrome. Muscles, ligaments and tendons journal. 2015 Jan-Mar:5(1):18-22
[PubMed PMID: 25878982]
[9]
Jeon S, Kim DY, Shim DJ, Kim MW. Common Peroneal Neuropathy With Anterior Tibial Artery Occlusion: A Case Report. Annals of rehabilitation medicine. 2017 Aug:41(4):715-719. doi: 10.5535/arm.2017.41.4.715. Epub 2017 Aug 31
[PubMed PMID: 28971059]
Level 3 (low-level) evidence
[10]
Li X, Song Y, Wang J. Anterior tibial artery occlusion post total knee arthroplasty: A case report. Medicine. 2019 Jul:98(29):e16503. doi: 10.1097/MD.0000000000016503. Epub
[PubMed PMID: 31335720]
Level 3 (low-level) evidence