Introduction
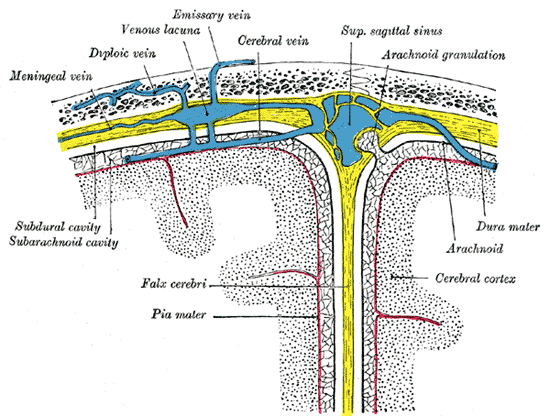
The brain and spinal cord are enveloped within three layers of membrane collectively known as the meninges, with the cranial meninges specifically referring to the section that covers the brain. From superficial to deep, the three layers are the dura, arachnoid, and pia—the term “mater,” Latin for mother, often follows these names (i.e., dura mater, arachnoid mater, pia mater).[1] The dura, Latin for “hard,” is composed of dense connective tissue and adheres to the inner surface of the skull and vertebrae. The arachnoid is a thin wispy membrane that lies just deep to the dura and is superficial to the pia, the very thin, clear membrane that directly adheres to the surface of the brain and spinal cord. Forming from these layers are three clinically significant spaces, or potential spaces (sometimes called cavities): the epidural, subdural, and subarachnoid spaces, from superficial to deep. The chief function of the meninges is to protect the contents of the brain and spinal cord.[2]
Structure and Function
Epidural Space
Between the roof of the skull (i.e., calvarium) and the superior surface of the dura potentially lies the epidural space. While arteries and veins run between the inner surface of the calvarium and the dura, the epidural space typically exists pathologically, since the superficial layer of the dura, the periosteal layer, is securely attached to the periosteum of the skull.
Dura Mater
The outermost mater of the meninges, the dura, is composed of two layers: the periosteal layer that lies closest to the calvarium and the meningeal layer that lies closest to the brain tissue. These together contribute to the dura being a thick, dense, fibrous membrane that is quite inelastic. The periosteal layer consists of fibroblasts and osteoblasts, with a large quantity of extracellular collagen existing within its intercellular space, giving the dura its strength.[1] These two layers are mostly fused, only separating to form venous sinuses and dural reflections. Dural reflections refer to places where two face-to-face meningeal layers descend into the cranial cavity to form the septa that compartmentalize the brain. The two main dural reflections are the falx cerebri and the tentorium cerebelli. The sickle-shaped falx cerebri is attached to the roof of the cranium and suspends down into the interhemispheric fissure, separating the right and left cerebral hemispheres. The “U” shaped tentorium cerebelli runs transversely between the cerebellum and occipital lobes. Importantly, there is an opening in the falx cerebri, known as the tentorial incisura (sometimes referred to as the tentorial notch), that allows the midbrain to pass through into the middle cranial fossa.
Subdural Space
The subdural space is the space that potentially exists between the meningeal layer of the dura and the arachnoid mater. Similar to the epidural space, the subdural space typically exists only under pathological conditions.
Arachnoid Mater
The arachnoid sits between the dura and the pia and is an avascular membrane that is involved in cerebrospinal fluid (CSF) metabolism via the subarachnoid space.[2] Unlike the pia mater, the arachnoid does not follow the contours of the cortical sulci but bridges them. While its appearance varies between locations in the cranium, it is generally a thin, lucent membrane. Its structure consists of a superficial mesothelial layer below the dura, a central layer composed of cells conjoined by many junction proteins, and a deep layer of less tightly packed cells with many collagen fibers within their intercellular space. Evidence suggests that the clusters of arachnoid villi (i.e., arachnoid granulations), or portions of the arachnoid that protrude into the dura mater, serving as a network for communication between the systemic venous system and the CSF.
Subarachnoid Space
The subarachnoid space is the cerebrospinal fluid-filled space that exists between the arachnoid and the pia. Within the lateral ventricles of the brain, the choroid plexus produces CSF, which passes into the subarachnoid space via the foramina of Luschka.[3][4] Since the subarachnoid space is continuous between the brain and spinal cord, CSF flows through the foramen magnum down to the distal portion of the spinal cord. The primary functions of the CSF are to cushion the brain and spinal cord from trauma and to supply them with nutrients and remove waste. In addition to the CSF, the major arteries of the brain run through the subarachnoid space. Also, projecting into this space are arachnoid trabeculae which are strands of arachnoid mater connective tissue.
Pia Mater
The deepest layer of the meninges, the pia mater, is composed of two layers and, unlike the arachnoid, follows the contours of the sulci and gyri. The outer layer of the pia, referred to as the epipial layer, contains collagen fibers; the inner layer, or the intima pia, contains elastic and reticular fibers.[5][6] While mesothelial cells of the epipial layer connect to the arachnoid mater via the arachnoid trabeculae, the intima pia adheres to the outermost layer of neural tissue known as the glial membrane. Importantly, the cerebral pia mater forms sheaths around the blood vessels that enter and exit the brain perpendicular to the meninges, specifically from the subarachnoid space to within the brain parenchyma.[7] This sheathing creates an interstitial fluid-filled space, known as the perivascular or Virchow-Robin space, between the vessel walls and the pia.
Embryology
While the dura mater, sometimes called the pachymeninx, is derived from the mesoderm, the arachnoid and pia mater, together called the leptomeninges, are derived from the ectoderm. Specifically, the development of the meninges begins with what is known as the perimedullarly mesenchyme, which contains cells from both the ectoderm and mesoderm.[1][8] The leptomeninges forms first, as cells from the neural crest differentiate into the pia and arachnoid. Subsequently, dura differentiation occurs from sclerotomes, a subdivision of the mesodermal somites. The dura differentiates from the development of the skull as the venous sinuses begin to develop and arises from two distinct condensations of cells in the peripheral mesenchyme; the thicker condensation forms the periosteal layer, while the thinner forms the meningeal layer.[9]
Blood Supply and Lymphatics
Epidural Space and Dura Mater
While it was once thought that the dura was avascular, it is actually highly vascular in nature, as the major vessels that supply it run in the epidural space deep to the skull. The major arteries that supply the dura are derived from the internal carotid, vertebral, maxillary, ascending pharyngeal, lacrimal, occipital, and ethmoidal arteries. Of the arteries that supply the dura, the middle meningeal artery (MMA), which branches from the internal carotid artery’s maxillary branch, is the most important.[1] The MMA enters the cranium via the foramen spinosum and runs inside the epidural space, forming grooves against the skull. Importantly, while the MMA supplies the dura, the middle cerebral artery that branches from the internal carotid artery supply the brain. Venous drainage of the dura occurs via the satellite veins of the meningeal arterial trunks and the dural venous sinuses.
The dural venous sinuses are venous channels formed where the periosteal and meningeal layers of the dura mater separate and serve as the major pathway for venous drainage from the brain. They include the superior sagittal sinus, inferior sagittal sinus, straight sinus, and sigmoid sinus, among others.[1] The dural sinuses mainly drain blood via the sigmoid sinuses into the internal jugular veins. In addition to receiving blood from both the brain’s internal and external veins, the dural sinuses receive CSF from the subarachnoid space.
Subdural Space
The most notable blood vessels related to the subdural space are the bridging veins, which pass through the subdural space transversely on their way to drain the cerebral hemispheres into the dural venous sinuses. The rupturing of these veins is the most common cause of subdural hematomas.
Arachnoid Mater and Subarachnoid Space
The arachnoid mater is avascular. Areas of the subarachnoid space where there are large gaps are referred to as cisternae. The ambient cistern, which surrounds the midbrain, contains branches of the posterior cerebral and superior cerebellar arteries; it also contains the basal vein of Rosenthal. The superior cerebellar cistern contains the petrosal vein and the superior cerebellar artery. Additionally, where the arachnoid mater bridges the cerebral hemispheres deep to the falx cerebri, the subarachnoid space houses the anterior cerebral arteries.
Pia Mater
The pia mater is highly vascularized and contains networks of capillaries that nourish the brain. Additionally, the portions of the pia mater that form the perivascular space eventually fuse with the blood vessels they surround.
Meningeal Lymphatic Vessels
The lymphatic system of the meninges was recently discovered in 2015 via the use of electron microscopy, and work is ongoing to better understand its structure and function.[10][11] Lymphatic vessels run tangentially to the dural venous sinuses and meningeal arteries and connect to the deep cervical lymph nodes. Additionally, these vessels have been shown to absorb CSF for drainage and are thought to play a central role in connecting the immune and nervous systems through immune cell trafficking.
Nerves
The meninges primarily receives innervation by the vagus and trigeminal nerves, with some cervical spinal nerves contributing to a lesser degree.[2] While the dura of the anterior cranial fossa is primarily innervated by the anterior and posterior ethmoidal nerve branches of the ophthalmic division of the trigeminal nerve, the dura of the middle cranial fossa receives nerve supply from a branch of the maxillary division of the trigeminal nerve. The tentorium cerebelli and the posterior third of the falx cerebri are primarily innervated by the tentorial nerve, which is also a branch of the ophthalmic division of the trigeminal nerve. The first three cervical spinal nerves, along with the cranial sympathetic trunk, mainly innervate the infratentorial dura of the posterior cranial fossa.
Surgical Considerations
Meningiomas are the most common type of cranial neoplasms and arise from the cells that make up the arachnoid villi, known as arachnoid cap cells. They are typically benign but can present in an atypical or malignant fashion.[12] While surgery is usually employed to treat meningiomas, the risk of serious neurological complications had led to its steady decline, especially when the tumor is in regions of the skull near the critical neurovascular structures.[13] The primary strategy for cranial meningioma removal is total excision, which typically entails the removal of the dura, bone, and vascular sinuses that have been infiltrated by the tumor. In recent decades, endoscopic and minimally invasive keyhole approaches to surgery have seen heightened implementation in select cases. Ultimately, the surgical strategy is patient-tailored and depends on each tumor’s location and characteristics.
Clinical Significance
The meninges plays a role in numerous pathological conditions. Bacterial meningitis (BM) is a condition where one gets inflammation of the meninges due to bacteria invading the subarachnoid space, most commonly by the pathogens Streptococcus pneumoniae and Neisseria meningitides.[14] Bacterial meningitis may lead to neuronal damage as a result of increases in intracranial pressure and subsequent parenchymal damage due to brain edema, hydrocephalus, and vascular alterations. Additionally, evidence suggests that toxins released from the infiltrated pathogens may contribute to neuropsychological deficits — treatment centers around immediate antibiotic therapy.
Traumatic and atraumatic intracranial hemorrhages within different locations of the meninges are a common set of conditions that are directly related to the structure and function of the meninges and can be classified by their specific location within the meningeal layers. For example, an epidural hematoma is the collection of blood in the tight potential space between the dura and the skull (i.e., the epidural space).[15] This condition is usually caused by the rupturing of the middle meningeal artery as a consequence of the fracture of the temporal bone as a result of head trauma. As the hemorrhage rapidly expands under arterial pressure, the dura peels away from the calvarium creating a lens-shaped biconvex hematoma, as seen by a CT scan. As the hematoma compresses the underlying brain tissue, brain herniation can occur and lead to death unless treated with surgery. Other intracranial hemorrhages include subdural hematomas, which usually result from rupturing of the bridging veins and the accumulation of blood in the potential subdural space between the dura and the arachnoid,[16] and subarachnoid hemorrhages, which occur in the subarachnoid space.[17] Subarachnoid hemorrhages are often further classified as nontraumatic (spontaneous) or traumatic; nontraumatic subarachnoid hemorrhages are usually a result of a spontaneous aneurysm (or rupture) of an artery in the space between the arachnoid and the pia and present with a sudden onset headache.[18]