Introduction
The human face possesses over two dozen individual muscles on each side - upwards of 30, depending on how they are counted. The facial muscles are striated muscles that link the skin of the face to the bone of the skull to perform important functions for daily life, including mastication and expression of emotion. While the individual movements these muscles produce are varied and diverse, it may be helpful to categorize them into two rough groups: the muscles of facial expression, also known as the mimetic muscles, and the muscles of mastication. The muscles of facial expression are innervated by the facial nerve (cranial nerve VII), and the muscles of mastication are innervated by the mandibular division of the trigeminal nerve (cranial nerve V3).[1] Using innervation to distinguish the two groups makes categorization largely dependent on embryonic origin, which does not always precisely correlate with function; this is nevertheless the most common method of describing the muscles.
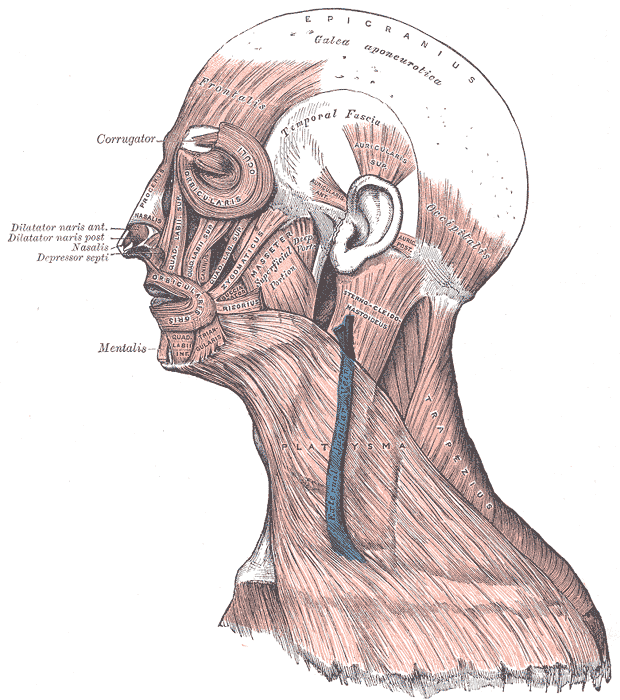
Despite different innervations and functions, the facial muscles, by and large, act in synchrony. For example, during chewing, the orbicularis oris and buccinator muscles act to retain the food inside the mouth while the masseter and temporalis muscles move the mandible to chew the food. If anteroposterior or lateral and medial adjustment of the mandible is required, the pterygoid muscles provide that movement. The facial and mandibular nerves also both control muscles that participate in neither facial expression nor mastication; however, dysfunction of either of these nerves can be debilitating, as few other motor nerves control so many individual muscles that are so critical to the human experience. When facial and trigeminal nerve function is impaired, patients may suffer massive quality of life sequelae and have great difficulty remaining comfortable as members of society.[2][3][4] See Image. Muscular and Fibrous Structures of the Head, Face, and Neck.
Structure and Function
The facial muscles serve two major functions for the body: mastication and facial expressions. The primary muscles of mastication include the temporalis, medial pterygoid, lateral pterygoid, and the masseter, although the mylohyoid and anterior digastric muscles also move the mandible and assist with the acts of chewing and swallowing. The masseter originates on the undersurface of the zygomatic arch and wraps around the angle of the mandible to provide forceful closure of the jaw. The temporalis has a similar function but originates as a large fan shape in the temporal fossa across the frontal, temporal, parietal, and sphenoid bones, then travels deep to the zygomatic arch and inserts on the coronoid process and ramus of the mandible. The medial pterygoid muscle originates on the lateral pterygoid plate of the sphenoid bone and inserts on the medial aspect of the mandibular ramus and angle, completing a sling with the masseter, which inserts on the lateral surface of the mandibular angle; the medial pterygoid aids closure of the jaw and protrusion of the chin. The lateral pterygoid muscle originates on the lateral pterygoid plate as well but inserts on the condyle of the mandible to assist with protrusion of the chin and opening of the jaw. The mylohyoid and anterior digastric muscles also serve to open the jaw, running from the hyoid bone to the inner aspect of the mandible.
There are far more muscles of facial expression than there are muscles of mastication. The mimetic muscles are considered to be an extension of the superficial musculoaponeurotic system (SMAS) of the face, which is a fascial plane deep to the subcutaneous tissue but superficial to the muscles of mastication, running from the platysma in the neck up to the galea aponeurotica and the temporoparietal fascia under the scalp.[5] In the upper face, there are several muscles, including the frontalis (connected to the occipitalis via the galea aponeurotica), which raises the eyebrows and produces transverse forehead rhytides, the more superficial corrugator supercilii, which depresses the eyebrows and causes vertical glabellar rhytides ("number 11s" or "frown lines"), and the procerus, which is an even more superficial, midline muscle that causes horizontal rhytides at the root of the nose. In the midface, there are the orbicularis oculi sphincter muscles, which close the eyes, depress the brows, and cause crow's feet wrinkles, and there are the muscles of the nose as well. The orbicularis oculi muscles are exceptionally close to the skin surface, with essentially no subcutaneous fat between its fibers and the dermis. Hypertrophy of the orbicularis oculi may produce bags under the lower eyelids known as festoons, although this is not the most common cause of baggy eyelids. The nasal muscles are the nasalis, which causes vertical "bunny lines" on the nasal sidewalls when patients snarl, and the depressor septi, which pulls down the nasal tip when the upper lip moves, and the paired dilator naris, which flares the nostrils. The elevators of the upper lip, from medial to lateral, are the levator labii superioris alaeque nasi, the levator labii superioris (also known as the quadratus labii), and the levator anguli oris, which lies deeper than the other two. Inserting on the modiolus of the oral commissure and serving to move the corner of the mouth upward and outward during smiling are the more medial zygomaticus minor and the more lateral zygomaticus major. The zygomaticus major is the most commonly replaced muscle in facial reanimation surgery, even though additional rehabilitation of upper lip elevation and lower lip depression provides a more natural result when possible.[6][7][8]
Continuing around the oral commissure from lateral to medial along the lower lip is the risorius, which pulls the corner of the mouth directly outward, and the deeper buccinator tightens the cheek to prevent food pocketing while chewing. The depressor anguli oris (also known as the triangularis) is a continuation of the platysma muscle that pulls down on the corner of the mouth, and just medial to that is the depressor labii inferioris. Lastly, the mentalis is an unpaired muscle of the chin that allows protrusion of the lower lip. All of these perioral muscles insert onto the orbicularis oris, which is the sphincter muscle that allows closure of the lips and permits articulate speech. In the neck, the platysma muscles are large sheets that produce vertical bands during contraction and may aid with lower lip depression. Laterally, the superior, posterior, and anterior auricular muscles move the pinna around subtly, which may have had a role in sound localization during evolution many millennia ago. There are also a number of small muscles lying upon the cartilage of the pinna itself, and these have no apparent extant function either. In some patients, a temporoparietalis muscle also exists within the temporoparietal fascia, which may help elevate the auricle and apply tension to the scalp; its function is far from critical. What makes the muscles of facial expression unique is that while most other skeletal muscles in the body serve to move bones, the mimetic muscles originate on bone and insert in the dermis, serving to manipulate the skin and soft tissues.[9] Additionally, the fastest muscles in the human body are muscles of facial expression: the orbicularis oculi and the zygomaticus major. When compared to other muscles, facial muscles have a higher fast-twitch fiber concentration and fewer mitochondria.[10]
Embryology
The facial muscles develop from the first and second branchial, or pharyngeal, arches, beginning to form in the fourth week of development.[11] The arches represent the mesodermal components of the branchial apparatus and develop into the muscles. The branchial clefts contain ectoderm and become skin, while the branchial pouches contain endoderm, which becomes mucosal surfaces. Within the first arch is Meckel's cartilage, which becomes the maxilla and mandible as well as the malleus and incus. Therefore, the muscles that develop from this arch are involved in mastication and are controlled by the mandibular division of the trigeminal nerve (CN V3).[12] In addition to the muscles of mastication, the tensor veli palatini, and the tensor tympani, which inserts onto the neck of the malleus, are also controlled by CN V3.
The mimetic muscles derive from the second branchial arch, which contains Reichert's cartilage, a structure that ultimately forms the styloid process of the temporal bone, the stylohyoid ligament, and the lesser cornu of the hyoid bone.[13] For this reason, the nerve associated with the second branchial arch, the facial nerve (cranial nerve VII), is also responsible for the innervation of the stylohyoid and posterior digastric muscles.
Blood Supply and Lymphatics
The muscles of the face are predominantly perfused by branches of the external carotid artery, particularly branches of the facial artery. The facial artery is generally the fourth branch off of the external carotid, after the superior thyroid, ascending pharyngeal, and lingual, and is inferior to the occipital, posterior auricular, superficial temporal, and internal maxillary branches. The first major branch of the facial artery, the submental artery, supplies the anterior digastric muscle, a portion of the platysma, and the mylohyoid, the latter of which is also fed by the inferior alveolar artery that runs through the mandible. The posterior digastric muscle is perfused by the occipital artery, while the remainder of the platysma is supplied by the suprascapular artery. After crossing the gonial notch, the facial artery courses towards the modiolus of the oral commissure, where it feeds the perioral muscles by branching into the inferior labial and superior labial arteries, the latter of which proceeds towards the nasofacial junction, becoming the angular artery. The superficial temporal artery gives off the transverse facial artery anterior to the auricular lobule, which runs parallel and superior to Stensen's parotid duct and perfuses the midfacial muscles. The superficial temporal artery continues superiorly toward the temporal region and separates into anterior and posterior branches. The anterior branch supplies the frontalis muscle, anastomosing with the supraorbital and supratrochlear arteries - branches of the internal carotid artery - to supply the corrugator and procerus muscles. The posterior branch of the superficial temporal artery supplies the temporoparietalis muscle and the lateral scalp, anastomosing with the occipital and posterior auricular arteries, the latter of which perfuses the auricular musculature.[14][15][16]
The muscles of mastication are supplied by deeper arteries, generally branches of the internal maxillary artery, itself the largest terminal branch of the external carotid artery. This is consistent with the embryology as mentioned earlier, as the internal maxillary artery is the vessel associated with the first branchial arch.[11] The internal maxillary artery often divides into three parts: the inferior alveolar (which supplies the mylohyoid muscle), middle meningeal, and some smaller branches arising from the first section. The second section gives off the anterior and posterior deep temporal branches to the temporalis muscle and the branches to the pterygoid, buccinator, and masseter muscles. Numerous branches come from the third segment, including the infraorbital and sphenopalatine arteries, but these are not critical to the perfusion of the facial musculature.
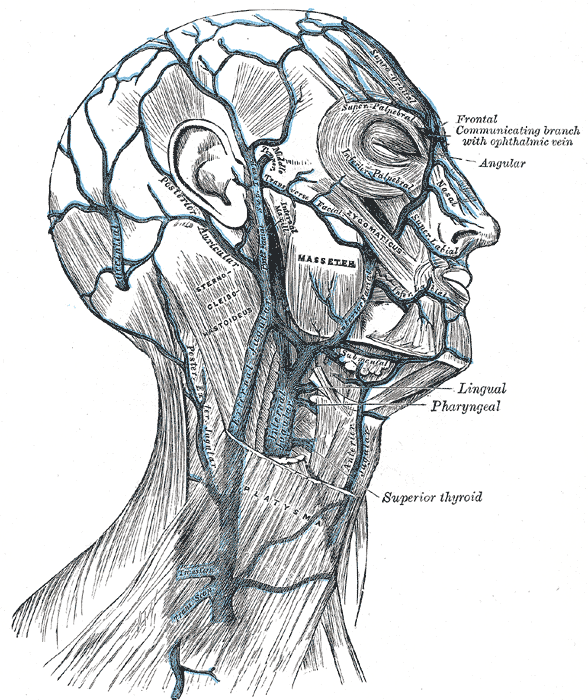
Venous drainage from the face proceeds through a system that largely corresponds to the arterial supply; however, the superficial temporal vein splits and drains both into the deep system (which includes the retromandibular and facial veins that then drain into the internal jugular vein) as well as the superficial system, which drains into the external jugular vein. The deeper muscles of mastication, namely the temporalis, masseter, and pterygoid muscles drain into the pterygoid plexus, which itself drains into both the retromandibular vein and the cavernous sinus; the pterygoid plexus is located between the temporalis and lateral pterygoid muscles. While there exists some variability in arterial anatomy, there is substantially more in venous drainage.[17][16] See Image. Veins of the Neck, Head, and Face, and Their Branches.
Lymphatic drainage of the facial muscles occurs via nodes in the preauricular, infra-auricular, parotid, nasolabial, buccinator, submandibular, submental, internal jugular, and anterior jugular basins.[16] These nodes themselves ultimately drain into the cervical lymph nodes.
Nerves
As mentioned above, the primary difference between muscles of facial expression and muscles of mastication is their embryological origin, and the embryological origin is what determines their innervation. The muscles of facial expression are innervated by the facial nerve, whereas the muscles of mastication receive innervation from the mandibular division of the trigeminal nerve.
The facial nerve exits the stylomastoid foramen in the lateral skull base and gives off branches to the auricular muscles, the posterior digastric muscle, and the stylohyoid muscle, then it enters the parotid gland, where it divides the superficial and deep lobes. Within the parotid gland, the facial nerve splits into five major branches at a point referred to as the "pes anserinus" because the branches and their anastomoses resemble the webbed foot of a goose. The branches then exit the anterior, superior, and inferior borders of the parotid gland en route to the mimetic muscles. These facial nerve branches travel on the masseteric fascia within the midface, deep to the SMAS. Because the SMAS is contiguous anteriorly with the facial muscles, inferiorly with the platysma, and superiorly with the temporoparietal fascia and the frontalis muscle, facial nerve branches in these areas are likewise found on the deep surface of these structures. There are three exceptions, which are muscles innervated from their superficial surfaces because of their deep location within the face. They are the buccinator, the mentalis, and the levator anguli oris muscles.[18]
The muscles of the upper face are innervated by the frontal (also known as temporal) branch: frontalis, corrugator supercilii, and procerus.[19] The orbicularis oculi muscle is innervated by the frontal branch as well as the zygomatic branch, which also controls the muscles of the midface along with the buccal branch.[20] The marginal mandibular branch of the facial nerve innervates the depressor labii inferioris and the depressor anguli oris and mentalis muscles. The cervical branch is primarily responsible for controlling the platysma muscle.[21][22]
The mandibular nerve separates from the trigeminal ganglion in Meckel's cave, a pouch in the tentorium cerebri at the petrous apex of the temporal bone. From there, it exits the skull via the foramen ovale and enters the infratemporal fossa, where it passes between the tensor veli palatini and the lateral pterygoid muscles and gives off branches to the medial pterygoid, tensor veli palatini, and tensor tympani muscles. It then divides into anterior and posterior branches; the anterior branch gives off motor fibers to the lateral pterygoid and masseter muscles, as well as the deep temporal nerves that control the temporalis muscle. The posterior branch is predominantly sensory but includes motor fibers within the inferior alveolar nerve that control the anterior digastric and mylohyoid muscles.[23]
Surgical Considerations
While damage to facial muscles intraoperatively is unlikely to result in long-term dysfunction of either mimetic function or chewing, facial nerve branches are easily injured during multiple different types of surgery, which may result in temporary or permanent muscle weakness. Iatrogenic injury most commonly results from tumor resection, especially in the parotid and skull base regions, but also occurs with temporomandibular joint replacement, middle ear surgery, and facelifting.[24] If transected, the facial nerve is ideally repaired via primary neurorrhaphy or cable grafting, ideally within 72 hours after an injury because the Wallerian degeneration that occurs thereafter makes identifying the nerve stumps more challenging, as they will have become non-stimulable after that time period.
Facial muscles themselves may also play a role in reconstructive surgery, particularly the rehabilitation of facial paralysis. When the facial nerve is dysfunctional, one entire side of the face may be either weak or completely paralyzed. Depending on the etiology of the palsy, numerous treatment options may exist; however, in more severe cases, transfer of a muscle innervated by the mandibular branch of the trigeminal nerve may provide a viable reanimation option. Historically, the masseter was disinserted from the angle of the mandible and attached to the modiolus of the oral commissure so that the act of biting would help to produce a smile, but the unnatural bulk and movement vector that resulted led the procedure to be abandoned in favor of repositioning of the temporalis muscle instead.[25][26] When only a single branch of the facial nerve has been injured, such as the marginal mandibular branch, transfer of the anterior belly of the digastric muscle or the platysma may help restore lower lip depression and a more symmetric smile.[27][28] Additionally, in cases of severe blepharoptosis, even though it is not due to facial nerve dysfunction, the frontalis muscle may be used to help raise the eyelid via a surgically placed sling.[29]
Lastly, facial muscles may serve as useful landmarks in facial surgery. The deep plane facelift, a commonly-employed technique originally described by Hamra in 1990, uses the surface of the zygomaticus major muscle as a dissection plane for elevating the malar fat pad.[30] Following the zygomaticus major muscle also serves as an excellent method of identifying the modiolus of the oral commissure when performing a static sling or dynamic reanimation procedure to restore smiling in cases of facial paralysis.
Clinical Significance
The most common clinical issues affecting facial musculature are facial paralysis, blepharospasm or hemifacial spasm, and bruxism. Facial paralysis can result from myriad pathologies affecting either the central or peripheral nervous system and from localized or systemic processes.[31] The most common facial paralysis is Bell's palsy, which fortunately has an excellent prognosis, with 70-90% of patients ultimately regaining premorbid function.[32][33] Patients who do not regain normal mimetic function may suffer from chronic problems with corneal exposure as well as difficulty eating, articulating certain sounds while speaking, and generally feeling uncomfortable interacting in society.[2]
Blepharospasm is a condition in which the orbicularis oculi muscle twitches periodically and occasionally can spread to involve other midfacial muscles; this condition is termed "hemifacial spasm." Common causes of facial spasms include neoplastic lesions abutting the facial nerve and blood vessels, such as the anterior inferior cerebellar artery, pulsating on the nerve and causing irritation and excitability. Some patients present with congenital hemifacial spasm, and in some cases, the movement disorder is psychogenic.[34] Regardless of the cause, patients often find that blepharospasm and hemifacial spasm make them self-conscious, and many limit their social activities in a similar manner to patients with facial paralysis. In many cases, chemodenervation with botulinum toxin provides some symptomatic relief.
Bruxism is more common than either of the first two conditions and affects between 8% and 31% of the population, causing teeth grinding that occurs most commonly at night.[35] Daytime bruxism is likely related to stress or other behavioral factors, whereas nocturnal teeth grinding may result from central neurotransmitter abnormalities.[36] Frequent grinding of the teeth often results in accelerated dental wear and facial pain syndromes, such as temporomandibular joint dysfunction, if allowed to continue chronically. The wear of mouthguards at night and injection of botulinum toxin can often alleviate symptoms.
From an aesthetic standpoint, facial muscles often contribute to signs of aging and are frequent targets for cosmetic procedures. As mentioned above, hypertrophy of the orbicularis oculi muscles can cause festoons, which contribute to a chronically tired appearance. Removing them surgically is challenging but can be very rewarding for patients. Many facial muscles also contribute to the production of wrinkles, particularly the "crow's feet" lateral orbital rhytides caused by the orbicularis oculi, glabellar "frown lines" caused by the corrugator supercilii muscles, "bunny lines" caused by the nasalis muscle, and "smoker's lines" caused by the orbicularis oris. Transverse forehead rhytides result from chronic frontalis contraction, frequently due to compensation for brow ptosis, and vertical platysmal bands often appear as the medial edges of the muscles separate from each other over time. Excessive tone in the depressor anguli oris muscles can cause the corners of the mouth to turn downwards, resulting in a chronically angry appearance. All of these complaints are frequently treated successfully with botulinum toxin injections.[37]