Continuing Education Activity
Peroneal tendon disorders are a cause of hindfoot and lateral foot pain. There are three primary disorders of the tendons; Peroneal tendonitis, peroneal subluxation, and peroneal tendon tears. These conditions are a cause of lateral ankle pain and may lead to ankle instability. The peroneal tendons are in the lateral compartment of the leg and include the peroneus longus and peroneus brevis muscles. This activity outlines the presentation and treatment of peroneal tendon syndromes and offers a review of the current non-operative and operative treatment options. This activity also highlights the importance of the interprofessional team in the management of peroneal tendon syndromes.
Objectives:
- Identify the epidemiology of peroneal tendon syndromes.
- Review the evaluation of peroneal tendon syndromes.
- Summarize the treatment and management options available for peroneal tendon syndromes.
- Describe interprofessional team strategies for improving care coordination and communication to advance peroneal tendon syndromes and improve outcomes.
Introduction
Peroneal tendon disorders are a cause of hindfoot and lateral foot pain. There are three primary disorders of the tendons; peroneal tendonitis, peroneal subluxation, and peroneal tendon tears; these conditions are a cause of lateral ankle pain and may lead to ankle instability. The peroneal tendons are in the lateral compartment of the leg and include the peroneus longus and peroneus brevis muscles. Both receive innervation from the superficial peroneal nerve and blood supply from the peroneal artery. The peroneus brevis originates on the lateral aspect of the distal fibula and intermuscular septum and inserts onto the base of the fifth metatarsal. The peroneus longus originates at the proximal fibula and lateral tibia and inserts at the base of the first metatarsal and the medial cuneiform. The tendons occupy a common synovial sheath that runs posterior to the distal fibula, once past the fibula they each have their own synovial sheath. They run in a tunnel bordered by the superior peroneal retinaculum, the posterior fibula that has a retromalleolar groove, and the calcaneofibular ligament.[1] Tendon relationship at the level of the ankle is the peroneus brevis anterior and medial to the peroneus longus.[2] Sometimes anomalous anatomy can lead to a peroneal disorder such as low lying brevis muscle belly or the presence of peroneus quartus muscle.[2] The peroneus quartus muscle most commonly runs form the peroneus brevis to the retrotrochlear eminence of the calcaneus and is associated with peroneus brevis tears, and subluxation.[3]
Etiology
Acute injury with a sudden contraction of the peroneal tendons can lead to acute injuries such as a tear of the tendon, or superior peroneal retinaculum, or avulsion of the tendons or the retinaculum from their attachments. If the tendons chronically subluxate, this can lead to inflammation and irritation causing tendonitis. The tendons rubbing over the posterolateral fibula can also lead to longitudinal tears of the tendons.[4] Chronic lateral ankle stability has also been shown to lead to subluxation and subsequent tears due to increased laxity and motion of the tendons.[5] Anatomical variants of the fibular retromalleolar groove, hindfoot alignment or cavus foot can lead to abnormal movement of the tendon leading to a predisposition towards subluxation or dislocation.[6]
Epidemiology
The most common patient population with tears of the peroneal tendons are active young patients. Tears are more likely to be longitudinal due to subluxation over the fibula, but can also be transverse. The peroneus brevis is more often torn isolated peroneus longus tears occur less frequently. A retrospective review of peroneal tendon tears showed brevis tears in 88% of patients, longus tears in 13% of patients and combined peroneus longus and brevis tears in 37%.[7]
Pathophysiology
The primary function of the peroneal tendons is to evert and plantarflex at the ankle. Also, the peroneus longus will plantarflex the first ray leading to hindfoot varus during walking. Having pre-existing varus hindfoot alignment can increase strain on the peroneus longus tendon that can lead to inflammation, subluxation, and possible tears.[8] The retromalleolar groove has different shapes; a cadaveric study showed out of 178 ankles the groove is concave in 82%, flat in 11 % and convex in 7% with a non-osseous fibrocartilaginous ridge that is on the medial side of the groove.[9]
Peroneal Tendonitis[9][5]
- Lateral ankle instability can cause laxity, leading to the increased motion of the tendons around the fibula with stretched superior peroneal retinaculum
- Low lying peroneus brevis muscle belly having to go through the narrow tendon sheath
Peroneal Subluxation/Dislocation[9]
- Instability can be acute from the rupture of the superior retinaculum or fibular groove avulsion or chronic. Chronic subluxation is associated with fibular groove flattening laxity of the superior retinacular ligament
Peroneal tendon tear[9]
- Musculotendinous junction during forceful contraction or in the cuboid tunnel
- Most tears are longitudinal and result from chronic subluxation over the distal fibula
History and Physical
History is essential in differentiating the pathology of peroneal tendons. It is necessary to identify the timing, aggravating position or activity, any traumatic events if there is associated swelling, as well as a description of the pain. A common pertinent history finding is a description of snapping or popping at the lateral malleolus. Patients must undergo screening for prior steroid injections and history of recent antibiotic use; Fluoroquinolones and steroids have associations with tendon disease.[6]
Physical exam should begin with an inspection of the ankle and foot for erythema or swelling, muscle strength testing of eversion and plantar flexion. The examiner can isolate the peroneus longus tendon by resisting active eversion through applying pressure to the medial first metatarsal head. Palpation of the tendons during ROM of the ankle. Evaluation of hindfoot biomechanics such as varus and valgus alignment should take place with the patient standing.[6] Ankle drawer test should be done to asses ankle ligamentous stability. Another physical exam technique is to have the patient lay prone with a knee to 90 degrees flexion and examine for peroneal tendon subluxation.[10]
Peroneal tendonitis presents with gradual onset of pain and swelling. There may be palpable fluid present in the tendon sheath with crepitation. The primary location of tenderness is along the peroneal tendons as they pass posterior and inferior to the fibular head. Tendon tears often have constant swelling, pain, or patient feeling of ankle instability or weakness. Tendon subluxation patients will have painful clicking and popping at the lateral malleolus. Subluxation may be apparent with voluntary eversion.[2]
Evaluation
The primary imaging modality with any suspected peroneal tendon disorder is X-rays of the ankle. X-rays should be weight-bearing and include standard AP, mortise, and lateral ankle views. Additional X-ray views are the axillary/Harris heel view and AP, lateral and oblique views of the foot to look for other fractures and foot alignment. Findings on the x-ray that indicate peroneal pathology are avulsion from the base of the fifth metatarsal, avulsion fracture of the distal fibular groove, os peroneum, and retromalleolar groove flattening.[9]
Ultrasound is a no radiation, inexpensive imaging modality that can provide an evaluation of the tendon in motion, as well as assist with injections. It has been shown to be effective in identifying tears as well with a sensitivity of 100 % and specificity of 85%.[11]
MRI is the next step in evaluation with a high-quality view of the tendons with no exposure to radiation. The sensitivity is 83%, and specificity is 75% for peroneus brevis tears. Findings include fluid surrounding the tendons, discontinuity, edema of the bone, and any bony deformity.[12]
CT scanning does expose the patient to radiation but provides better bony detail to evaluate possible bony deformity causing possible tendon dysfunction. If x-rays indicate the possibility of fracture, peroneal tubercle, or retro trochlear eminence CT scan would be useful and determine possible management.[9]
Treatment / Management
Nonoperative Treatment[9][6]
- Nonsteroidal anti-inflammatory drugs, ice, rest or immobilization, and physical therapy. Immobilization can include cast or controlled ankle motion boot. Modification of shoe wear can also help unload the peroneal tendons with the use of a lateral heel wedge.
- If this does not provide any improvement steroid injection around the peroneal tendon sheath can help with pain as well as assist with diagnosis.
- PRP injections with ultrasound guidance have shown improved functional outcomes with tendinopathy in the study by Dallaudiere. Four hundred eight patients showed 23 patients with peroneal tendon disorders.[13]
Non-operative treatment should be for 4 to 6 months to allow resolution of inflammation
Operative Treatment[9][2]
If conservative treatment has failed, operative management options of each type of disorder are as follows:
Peroneal Tendonitis
- Open Debridement and synovectomy
- Arthroscopic peroneal tendoscopy
Peroneal Tendon Subluxation
Treatment depends on the cause of the subluxation or dislocation. Goals are to restore the fibrocartilaginous rim, the superior peroneal retinaculum, and periosteum to the fibula and obtain smooth gliding of the tendon with adequate space for motion.
- If the superior peroneal retinaculum is torn then open or endoscopic repair or reconstruction is necessary.
- Avulsion fracture of the fifth metatarsal or fibular groove should entail fixation or repair.
- If the fibular groove is shallow endoscopic or open fibular groove deepening can be performed to provide a better structure for the peroneal tendons. This procedure usually addresses cases of chronic instability.
- If there is any hindfoot varus alignment, this should also be corrected to decrease stress on the peroneus longus with hindfoot osteotomy.
- Rerouting the peroneal tendons underneath the calcaneofibular ligament.[14]
- Bone block procedures that involve performing osteotomy of the fibula lateralizing it to create a bony block for the tendons.[2]
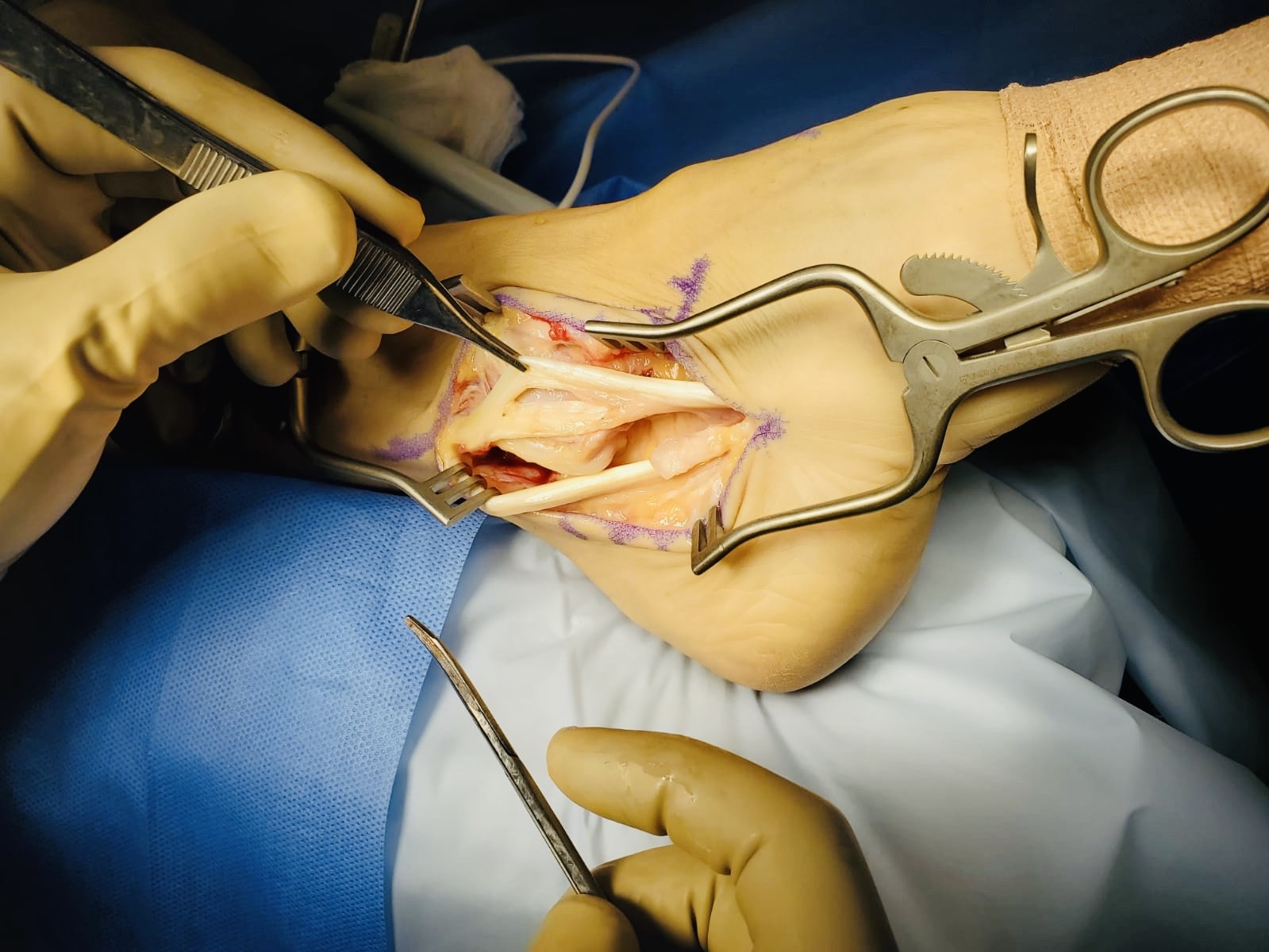
Peroneal Tendon Tears[9]
Treatment depends on the degree of tendon torn and whether the tear is acute or chronic
- Debridement and tubularization- partial tears of less than 50%.
- Repair end to end of acute complete tears
- Side-to-side anastomosis or Pulvertaft weave with chronic tears
- Allograft reconstruction
Differential Diagnosis
Must rule out ankle sprain, rheumatoid arthritis, calcaneus fractures, or fractured os peroneum. Some associated injuries with peroneal disorders are lateral ankle ligament tears as well as lateral ankle instability. Patients with varus heel may have associated Charcot-Marie-Tooth.[1][9]
Prognosis
For patients with Peroneal tendon tears, postoperative outcomes are good. With pain improvement and return to activity. Saxena showed 87% return to the sport in a case series of operatively treated tears.[15] Post-op repair of peroneal tendon tears in a retrospective review by Dombek showed that 98% of patients returned to full activities at an average follow up of 13 months.[7] Outcomes for operative treatment of tendon subluxation are good with Saxena showing a 100% return to sport after repair of the superior retinacular ligament.[16]
Complications
Reports exist of peroneal compartment syndrome after acute rupture of the peroneus longus tendon.
After tendon tear repair surgery, complications are re-tear and continued symptoms, shown to occur in about 10% of patients by Dombek.[7]
Deterrence and Patient Education
- Peroneal tendon disorders can cause lateral ankle pain
- There are three basic types of peroneal tendon disorders, tendonitis, subluxation, and tears.
- Not recognizing or treating these conditions may lead to continued pain or lateral ankle instability.
Enhancing Healthcare Team Outcomes
Peroneal tendon injuries vary in their severity and are managed by an interprofessional team to achieve the best outcomes. Patients with mild injury may present to the nurse practitioner or primary care provider. However, if the injury is severe, the patient should be referred to a specialist. Clinicians who manage these injuries should be aware that lateral ankle pain can have a multitude of isolated injuries or a combination of injuries.
Adequate interprofessional communication between athletic trainers, sports medicine physicians, nurse practitioner, podiatrists, and foot and ankle surgeons is paramount for diagnosing peroneal tendon injuries. The orthopedic surgeon should see patients and athletes who do not respond well to conservative management. Communication among these physician specialties is crucial. Additionally, a pharmacist may be necessary to verify medication reconciliation if the decision is made to institute NSAID or other pain management pharmacotherapy. Nurses will often be the point of initial contact at each visit, and their input on whether therapy is progressing should merit consideration. In both surgical and non-operative cases, a physical therapist will almost certainly be involved, and they will report to the healthcare team on the progress or lack thereof in the rehabilitative process. All members of the interprofessional healthcare team, therefore, must communicate and collaborate to drive patient outcomes to their best possible result. [Level V]
Most patients will require some type of rehabilitation to regain muscle function and strength. However, return to sporting activity should not be rushed, and the orthopedic surgeon should see the patient for clearance.
If promptly diagnosed, and surgical treatment of peroneal tendon injuries are required, athletic patients may return to sport by three months with successful outcomes.[16] [Level 2]