Introduction
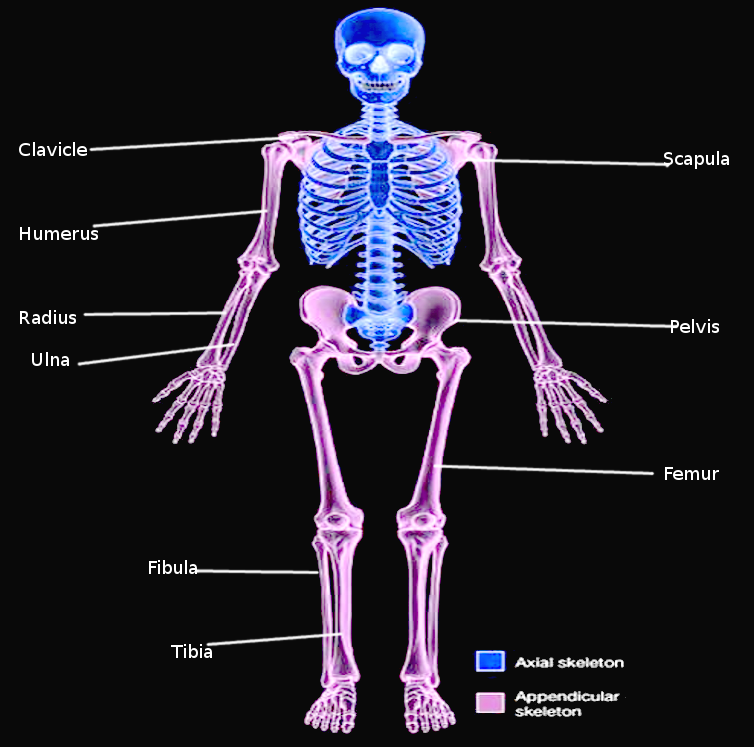
The appendicular skeleton is 1 of 2 major bone groups in the body, the other being the axial skeleton (see Image. Appendicular Skeleton). The appendicular skeleton comprises the upper and lower extremities. The shoulder and hip are important limb segments connecting the appendicular and axial skeleton, essential for mechanical load transfer.
Of the 206 bones in the adult human body, 126 form the appendicular skeleton. A single upper extremity is composed of 14 phalanges (proximal, intermediate, and distal), 5 metacarpals, 8 carpals, 2 forearm bones (radius and ulna), the humerus, and the shoulder girdle (scapula and clavicle). A single lower extremity contains 14 phalanges (proximal, intermediate, and distal), 5 metatarsals, 7 tarsal bones, 2 leg bones (fibula and tibia), the femur, and the hip (ilium, ischium, and pubis).[1]
Many ligaments, cartilage, and tendons strengthen bone articulations within the appendicular skeleton. Bony prominences and protuberances serve as muscle attachment sites. The appendicular skeleton is specialized for enhanced mobility and locomotion compared to the axial skeleton.
Structure and Function
The upper and lower appendicular extremity bones share fundamental similarities in their overall structure and function, including a bony framework consisting of long bones, articulations enabling a wide range of motion, and connections to the axial skeleton. Distinct differences reflect their specialized roles. The lower extremities primarily bear the body's weight and are involved in weight-bearing activities like standing, walking, and running. The upper extremities are designed for object manipulation and fine motor tasks. The upper extremities generally possess greater flexibility and dexterity for intricate movements and are shorter and lighter than the lower extremities. The 126 named appendicular skeletal bones, which exist in pairs, are described below.
Upper Limb
The upper limb bones include the bony framework of the shoulder, arm, forearm, and hand. The upper limb joints contribute to the upper skeleton's motion smoothness and efficiency.
The shoulder is the upper limb's proximal segment connected to the axial skeleton. The 2 shoulder bones are the clavicle and scapula. The clavicle is a long, S-shaped bone horizontally positioned at the front of the shoulder, connecting the sternum to the scapula. This bone acts as a strut, maintaining distance between the shoulder joint and the body, enhancing arm mobility, and providing protective support. The scapula is a large triangular bone on the upper back. This bone serves as an attachment point for shoulder muscles and contributes to shoulder movement and stability by articulating with the humerus.[2]
The arm's primary bone is the humerus, extending from shoulder to elbow. The humeral head articulates with the scapula's glenoid cavity to form the glenohumeral joint. Distally, the trochlea articulates with the ulna and the capitulum with the radius, forming the elbow joint. The humerus facilitates muscle attachment and enables shoulder and elbow movements.[3]
The forearm's 2 bones are the radius and ulna. The radius is the wider bone on the lateral side, while the ulna is the slimmer bone on the medial side. The radius' distal end articulates with the scaphoid and lunate bones of the wrist, allowing for hand and wrist flexion, extension, abduction, and adduction.[4] The ulna does not directly participate in forming the wrist joint. However, this bone forms the distal radioulnar joint with the radius near the wrist, which is crucial in supination and pronation.[5]
The hand bones consist of the carpal (wrist), metacarpal (palm), and phalangeal (finger) bones. The wrist bones are divided into 2 rows. From lateral to medial, the proximal carpal bones include the scaphoid, lunate, triquetrum, and pisiform. Meanwhile, the distal carpal row, from lateral to medial, consists of the trapezium, trapezoid, capitate, and hamate. The proximal carpal bones' distal surfaces articulate with the distal row. The distal carpals unite with the metacarpals distally. The wrist bones transmit muscle forces from the forearm to the palm and fingers, facilitating various hand movements.
The palm has 5 metacarpal bones, bridging the carpus with the phalanges. These bones articulate with the wrist through their bases (proximal end) and the phalanges through their heads (distal tip). The thumb's metacarpal is the shortest and thickest. The 3rd metacarpal has a styloid process lateral to its base. The metacarpals provide structural support to the palm, transmit muscle forces from the wrist and forearm, serve as muscle insertion points, and contribute to the hand's mobility and flexibility.
The fingers have 14 phalanges, 2 in the thumb (proximal and distal) and 3 in the medial fingers (proximal, middle, and distal). The thumb phalanges are thicker than those in the other digits. Like the metacarpals, the phalanges have a proximal base and a distal head. The thumb is separated from the other fingers and medially rotated to enable power-gripping and object manipulation.[6][7][8]
Lower Limb
The lower limb bones are specialized for body weight support, locomotion, and balance. Lower limb joints are generally stronger and have less movement flexibility than their upper limb counterparts. Bones in this region include the bony framework of the gluteal (buttocks), femoral (thigh), knee, leg, talocrural (ankle), and foot.
The hip bone (also known as the innominate or coxal bone) is formed by 3 fused bones. The ilium, located superiorly in the hip bone, comprises the superior portion and articulates with the sacrum posteriorly and pubis and ischium anteriorly at the acetabulum, contributing to the hip joint. The ilium primarily supports the trunk, transmits the upper body's weight to the lower limb, and serves as a site for various hip and trunk muscles' attachment. The ischium constitutes the hip bone's inferoposterior segment, articulating with the ilium and pubis at the acetabulum. The ischium supports the upper body's weight while sitting and provides attachment sites for hip and thigh muscles, including the hamstrings. The pubis forms the pelvic girdle's anterior portion. The pubic symphysis unites the right and left pubic bones, enhancing pelvic strength and stability, supporting the abdominal muscles, and serving as an attachment point for hip and thigh muscles.[9]
The femur is the thigh bone and the body's longest and strongest bone. The femur articulates with the innominate bone at the acetabulum to form the hip joint, and the tibia and patella to establish the knee joint. This bone sustains the upper body's weight during ambulation, supports thigh movement, and acts as a muscle attachment site.[10]
The leg bones consist of the tibia and fibula. The tibia is the larger and medial bone uniting with the femur at the knee joint superiorly and the talus at the ankle inferiorly. The tibia is united to the fibula at various points, including their proximal and distal articulations and the tibiofibular syndesmoses. The tibia is the only leg bone supporting body weight and stabilizing the ankle and knee joints. Various muscles responsible for knee, ankle, and foot movements attach to the tibia. The fibula is the thinner bone on the leg's lateral side. This bone does not participate in knee or ankle joint formation but acts as an attachment point for muscles that move the ankle and foot.[11][12]
The foot is divided into the tarsus (ankle), metatarsus (forefoot), and phalanges (toes). The tarsus has 7 bones: talus, calcaneus, cuboid, navicular, and 3 cuneiforms. The talus articulates with the tibia superiorly, transmitting body weight to the foot and contributing significantly to ankle movement and stability. The calcaneus is the heel bone and the foot's largest and strongest bone. The calcaneus unites with the talus superiorly and cuboid anteriorly, supporting body weight, absorbing impact forces during locomotion, and accommodating calf and foot muscle attachments. The cuboid lies on the foot's lateral side, articulating with the calcaneus posteriorly and the lateral cuneiform and 4th and 5th metatarsals anteriorly. This bone helps stabilize the midfoot and facilitate foot movement during gait.
The navicular bone is the bone articulating with the talus proximally and cuneiform bones distally, enhancing midfoot flexibility and mobility, maintaining foot arches (through the navicular tuberosity), and accommodating ligaments and muscle attachments. The medial, intermediate, and lateral cuneiforms articulate with the navicular bone proximally and the corresponding metatarsals distally. These bones support midfoot structures, contribute to foot arches, and provide foot ligament and muscle attachment sites.
The 5 metatarsals comprise the forefoot (distal or anterior foot). The 1st metatarsal, lying posterior to the big toe, is the shortest and widest bone in this region. The 2nd metatarsal, situated laterally to the 1st, is longer than the other metatarsals. Each metatarsal's base (posterior) is larger than its head (anterior). The metatarsal bases articulate posteriorly with the cuneiforms and cuboid, while the heads unite anteriorly with the phalanges. The metatarsals serve essential roles in the foot, providing structural support, distributing body weight evenly, and acting as levers for propulsion and movement. The foot has 14 phalanges, 2 in the 1st digit and 3 in each of the other 4. The phalanges aid in propulsion and push-off when walking, running, and jumping by leveraging the toe muscles. The toes contain numerous sensory receptors that provide feedback to the brain about the foot's position and movement, enhancing proprioception and contributing to overall coordination and balance.[13]
Sesamoid Bones
Sesamoid bones are small, round bones embedded within tendons or joint capsules. The appendicular skeleton contains sesamoid bones in various regions, the largest being the patella, which protects the knee joint and acts as an important attachment point for knee extensor ligaments. Other sesamoid bones are mostly in the hands and feet.[14]
Joints Connecting the Axial and Appendicular Bones
The appendicular skeleton directly articulates with the axial skeleton on 2 bilateral joints. The first of these articulations is the sternoclavicular joint, where the axial sternum articulates with the appendicular clavicle. The sternoclavicular joint is a synovial joint.[15] The second is the sacroiliac joint, where the sacrum, the axial bone, articulates with the ilium, the appendicular bone. The sacroiliac joint is both a synovial joint and a syndesmosis. The sacroiliac joint is critical to load transfer from the axial skeletal region to the lower extremity.[16]
The thoracoscapular (scapulothoracic) articulation is a secondary (indirect) articulation between the upper appendicular and axial skeleton, forming between the anterior scapular surface and ribs 2 through 7's posterior aspect. This articulation is not an actual joint and does not have a synovial membrane.
Blood Supply and Lymphatics
The subclavian artery is the upper limb's major arterial source. This blood vessel branches from the brachiocephalic trunk on the right and directly off the aortic arch on the left. The clavicle receives vascular supply from the suprascapular, thoracoacromial, and internal thoracic arteries. The subclavian artery becomes the axillary artery lateral to the 1st rib and continues as the brachial artery after passing the teres minor muscle's inferior border. The brachial artery bifurcates near the elbow into the radial and ulnar arteries, which distally contribute to hand vasculature.[20][21]
The lower extremity's blood supply originates from the common iliac arteries, the descending aorta's terminal branches. The common iliac artery branches into the internal and external iliac arteries, supplying all pelvic and lower limb structures. The external iliac artery continues into the lower extremity to become the femoral artery as it passes deep to the inguinal ligament.
The deep femoral artery, a major femoral artery branch, supplies blood to the femur. The medial and lateral femoral circumflex arteries are early deep femoral arterial branches vascularizing the hip joint. The femoral artery continues posteriorly to the knee as the popliteal artery. This blood vessel then descends into the lower leg, dividing into the anterior and posterior tibial arteries. The posterior tibial artery bifurcates into the posterior tibial and fibular arteries, which distally contribute to foot vasculature.[22]
Venous drainage in the upper limb closely mirrors the arterial pathways, with blood returning through a network of superficial and deep veins. Major veins like the cephalic and basilic veins converge into the axillary vein, which then joins the subclavian vein, returning blood to the systemic circulation.[23] In the lower limb, venous drainage initiates from superficial veins like the great saphenous vein, feeding into deeper vessels like the femoral vein. These veins, along with deep veins like the popliteal and anterior tibial veins, drain into the common iliac vein before returning to the heart via the inferior vena cava. The upper and lower limb lymphatics primarily follow the major blood vessels.[24]
Nerves
The upper extremity nerves originate from the brachial plexus, formed by spinal nerves C5 to T1. The brachial plexus is organized proximodistally into roots (C5-T1), trunks (superior, middle, and inferior), divisions (anterior and posterior), and cords (lateral, posterior, and medial), giving rise to named branches at various levels. The named nerves arising from the brachial plexus include the dorsal scapular, long thoracic, suprascapular, subclavian, lateral and medial pectoral, musculocutaneous, median, medial arm and forearm cutaneous, ulnar, upper and lower subscapular, thoracodorsal, axillary, and radial nerves.[25]
Lower extremity innervation originates from the lumbar and sacral plexuses, formed by spinal nerve roots T12 to S3. Part of the lumbosacral plexus forms the sciatic nerve, which innervates most of the lower limb. The sciatic nerve divides into the tibial and fibular nerves, which continue distally to innervate the leg and foot.[26]
Clinical Significance
The appendicular skeleton is clinically relevant in many areas of medicine. Appendicular skeletal trauma can fracture bones. United States 2016 emergency department national trends revealed that most upper limb fractures occurred in men, who frequently presented with phalangeal fractures. Women more commonly presented with distal radial or ulnar fractures.[36] Smaller, repetitive forces can lead to upper and lower limb stress fractures. Among long-distance runners, the sites most often affected by stress fractures are the tibia, foot, and femur.[37]
Appendicular skeletal bones may also be involved in malignancies, such as multiple myeloma or osteosarcoma.[38] Appendicular skeletal joints are also susceptible to various pathologies, including osteoarthritis, septic arthritis, and autoimmune diseases like rheumatoid arthritis. Appendicular skeletal bones may be evaluated using various modalities, including plain radiography, ultrasonography, computed tomography, and magnetic resonance imaging. The choice of imaging technique depends primarily on the pathology being imaged.[39][40]