Introduction
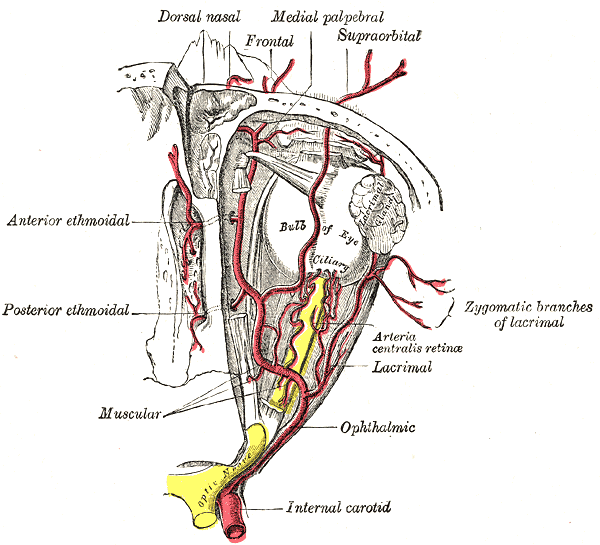
The ophthalmic artery is the first branch of the internal carotid artery. It comes off just distal to the cavernous sinus. The ophthalmic artery gives off many branches, which supply the orbit, meninges, face, and upper nose. When the ophthalmic artery is occluded, it can compromise vision. The ophthalmic artery comes off the internal carotid artery on the medial side of the anterior clinoid process and traverses anteriorly through the optic canal and just lateral to the optic nerve.[1][2][3]
The following are branches of the ophthalmic artery:
- The first branch of the ophthalmic artery is the central retinal artery that runs in the dura mater of the optic nerve. It then moves further along and supplies the inner layers of the retina.
- The second and the largest branch of the ophthalmic artery is the lacrimal artery. It also enters the orbit and traverses along the superior edge of the lateral rectus muscle. It supplies the eyelids, lacrimal gland, and conjunctiva.
- The ophthalmic artery gives off several posterior ciliary arteries that pass through the sclera and supply the posterior uveal tract. Because the posterior ciliary vessels are end vessels, sudden occlusion can produce infarction in the region of the choroid.
- The ophthalmic artery also gives off the inferior and superior muscular vessels that supply the extraocular muscles. The supraorbital artery is also a branch of the ophthalmic artery and passes through the supraorbital foramen to supply the skin of the forehead and Levator palpebrae muscle.
- Other branches of the ophthalmic artery include the ethmoid arteries, medial palpebral vessels, and terminal branches.
When there is occlusion of the ophthalmic artery, it can result in an ischemic syndrome. Amaurosis fugax is a condition associated with temporary, painless loss of vision due to either an embolic phenomenon or hypoperfusion. Emboli to the ophthalmic artery usually originate from the carotid artery bifurcation. One may visualize Hollenhorst bodies (a.k.a., Eickenhorst plaques) in the retina during fundoscopic evaluation. When there is a sudden, painless loss of vision in one eye, it is recommended that one obtain a duplex ultrasound of the neck to assess the carotid artery for atherosclerotic plaques.[4][5][6]
Embryology
Despite tremendous accumulated knowledge of the vascular anatomy, the understanding of the arterial development in the human embryo from the branchial to the postbranchial stage is still relatively poor. Key considerations in the area of blood supply to the orbit include the presence of both internal and external carotid contributions, with this dual "circuit" arrangement structured on embryological origins. In the majority of cases, communication between the middle meningeal artery and the ophthalmic artery is present, passing through the superior orbital fissure in most cases. Less commonly, an additional meningo-orbital foramen (foramen of Hyrtl) may be present lateral to the superior orbital fissure, with the connecting branch known as the sphenoidal artery, recurrent meningeal artery, or orbital branch of the middle meningeal branch.
Among clinically relevant, practical anatomy, important anomalies pertinent to the ophthalmic artery warrant being mentioned at this juncture. Dilenge and Ascherl (1980) reported on 42 anomalies of the ophthalmic and middle meningeal arteries. In that study, approximately 2.4% of anomalies involve the separation of ocular branches of ophthalmic artery from extraocular intraorbital branches. The same figure (2.4%) has been noted for the presence of accessory ophthalmic artery. In approximately 7.1% of cases, the ophthalmic artery arises from the middle meningeal artery. Approximately 17% of anomalies involve the ophthalmic artery arising from an extradural portion of the carotid siphon. The most common anomaly of this vascular circuit (about 40% of cases) is the middle meningeal artery arising from ophthalmic artery.[7][8]
In summary, the ophthalmic artery can arise from the middle meningeal artery, middle cerebral artery, or the posterior communicating artery. In addition, the middle meningeal artery can arise from the ophthalmic artery. Furthermore, the cavernous origin of the ophthalmic artery has been reported. Finally, the presence of persistent stapedial artery has been well described by neurovascular anatomy experts. All of the above anatomic variations must be recognized at the time of invasive procedures involving related blood supply to this critically important body region. For example, embolization of a tumor supplied by the external carotid artery may result in loss of vision if the eye depends on the anatomically anomalous routing of blood to maintain retinal perfusion.
Nerves
The ophthalmic artery is intimately associated with the optic nerve (e.g., Cranial Nerve II). Additional important neurovascular structures in proximity to the ophthalmic artery include the following structures:
Nerves
- Lacrimal Nerve (Cranial Nerve Va)
- Frontal Nerve (Cranial Nerve Va)
- Trochlear Nerve (Cranial Nerve IV)
- Superior Division of the Oculomotor Nerve (Cranial Nerve IIIs)
- Nasociliary Nerve (Cranial Nerve Va)
- Inferior Division of the Oculomotor Nerve (Cranial Nerve IIIi)
- Abducens Nerve (Cranial Nerve VI)
- Ganglionic Branches (from Pterygopalatine Ganglion to Maxillary Nerve)
- Infraorbital Nerve (Cranial Nerve Vb)
- Zygomatic Nerve (Cranial Nerve Vb)
Veins
- Superior Ophthalmic Vein
- Inferior Ophthalmic Veins
- Infraorbital Vein
Arteries
Muscles
As mentioned previously, the ophthalmic artery continues medially as the superior and inferior muscular branches. These important branch vessels originate either directly from the ophthalmic artery or from a separate trunk that subsequently divides into the superior and inferior branches. These branches provide blood supply to the extraocular muscles.
Clinical Significance
Additional important considerations regarding the ophthalmic artery include the following arterial branches:
- Ethmoidal Arteries = The ophthalmic artery turns anteriorly after reaching the medial orbital wall. The anterior ethmoidal artery enters the nose after traversing the anterior ethmoidal canal and brings blood supply to the anterior/middle ethmoidal and the frontal sinuses. This branch subsequently enters the cranium and supplies blood to the meninges. The posterior ethmoidal artery enters the nose through the posterior ethmoidal canal. It provides the blood supply for the posterior ethmoidal sinuses. It also subsequently enters the cranium and supplies the meninges.
- Medial Palpebral Arteries = The ophthalmic artery courses anteriorly toward the trochlea. Here, the superior and inferior medial palpebral arteries originate. This is the blood supply to the eyelids.
- The Supraorbital Artery = Branches from the ophthalmic artery during its course over the optic nerve, passes anteriorly along the medial border of the levator palpebrae and superior rectus, and then through the supraorbital foramen to provide blood supply to the muscles and skin of the forehead.
- The Terminal Branches = There are two terminal branches of the ophthalmic artery. The supratrochlear (frontal) artery and the dorsal nasal artery. Both of these vessels exit the orbit medially and supply the forehead and scalp.
Other Issues
It may be helpful for those studying the anatomy of the ophthalmic artery to utilize the mnemonic "DR MCLESSI," which stands for:
- D = Dorsal Nasal Artery
- R = [Central] Retinal Artery
- M = Muscular Artery
- C = Ciliary Arteries [Long / Short / Anterior]
- L = Lacrimal Artery
- E = Ethmoidal Arteries [Anterior / Posterior]
- S = Supraorbital Artery
- S = Supratrochlear Artery [Frontal]
- I = Internal Palpebral Artery
Because the mnemonic does not represent the correct order of ophthalmic artery branches, the reader should note that the first and second last branches of the mnemonic are the terminal branches, both exiting the orbit medially to supply the forehead/scalp.