Etiology
A history of smoking, alcohol consumption, and a diet low in fruits and vegetables accounts for almost 90% of esophageal squamous cell carcinoma in the United States. In developing countries, esophageal squamous cell carcinoma risk factors are less certain but may include poor nutritional status, a low intake of fruit and vegetables, and drinking beverages at high temperatures. Human papillomavirus (HPV) infection has been correlated with an increased incidence of squamous cell cancers of the upper esophagus. Preexisting anatomical diseases such as achalasia, caustic strictures, gastrectomy, and atrophic gastritis are associated with an increased risk of esophageal squamous cell carcinoma. A patient's current or previous squamous cell carcinoma of the aerodigestive tract may be related to synchronous or metachronous squamous cell carcinoma of the esophagus. Tylosis, a rare autosomal dominant syndrome associated with non-epidermolytic palmoplantar keratosis (or Howel-Evans syndrome), has a strong association with esophageal squamous cell carcinoma and carries a 40% to 90% risk of developing cancer by age 70. The gene TEC (tylosis with esophageal cancer) has been linked to a region on chromosome 17q25, which has been implicated in sporadic squamous cell carcinoma as well. Bloom syndrome, a rare autosomal recessive syndrome associated with leukemia, lymphomas, and Wilms tumor (or chromosomal breakage syndrome), may include esophageal squamous cell carcinoma diagnosed at an early age. Bloom syndrome is caused by a mutation in the BLM gene at 15q26 with elevated chromatid exchanges that may develop multiple malignancies. Fanconi anemia, an autosomal recessive disorder with congenital malformations, pancytopenia, and risk for hematologic malignancies, also contributes to an increased risk of squamous cell carcinoma. In post-marketing surveillance, oral bisphosphonates have been linked to esophageal squamous cell carcinoma and adenocarcinoma.
Most esophageal adenocarcinomas in the United States arise from Barrett metaplasia, of which 80% of cases are attributed to a history of smoking, high body mass index, gastroesophageal reflux disease (GERD), and a low fruit and vegetable diet. Alcohol intake has not been associated with adenocarcinoma. Barrett esophagus metaplasia has been associated with epidermal growth factor polymorphisms and other conditions which increase esophageal acid exposure, including Zollinger-Ellison syndrome, scleroderma, lower esophageal sphincter relaxing drugs, and procedures. Familial Barrett esophagus may be associated with rare autosomal inherited dominant susceptible alleles. It should be suspected in a patient with esophageal/GEJ adenocarcinoma, particularly in a white male, with GERD and older than 40 years. A high fiber diet, antioxidants, fruits and vegetables, folate, vitamin C, proton-pump inhibitors, and NSAIDs can protect against the development and progression of Barrett esophagus, and hence, esophageal adenocarcinoma, but despite these associations, none has been confirmed to be a preventive intervention.[4][5]
Pathophysiology
Esophageal squamous cell carcinoma arises from small polypoid excrescences, denuded epithelium, and plaques commonly located at the mid-portion of the esophagus. The early lesion may be subtle, and tissue staining with Lugol’s iodine should be used to stain normal squamous epithelium containing glycogen from malignant squamous glycogen-deprived cells to facilitate diagnosis. Advance lesions are ulcerated, circumferential, infiltrate submucosa, and extend in a cephalad direction. Spread occurs via the lymphatic system to regional lymph nodes, but a third of patients will have distant metastases to the liver, lung, and bone, including invasion of malignant cells to the bone marrow.
Approximately 60% of adenocarcinoma of the distal esophagus and, more typically, GEJ cases arise from Barrett esophagus metaplastic epithelium. The typical treatment for patients with Barrett's esophagus is surveillance using upper endoscopy and biopsy to examine tissue for evidence of dysplasia. The incidence rate for adenocarcinoma among patients without dysplasia is 1.0 case per 1000 person-years; on the other hand, the detection of low-grade dysplasia on the index endoscopy is associated with an adenocarcinoma incidence rate of 5.1 cases per 1000 person-years. The annual risk of esophageal adenocarcinoma is 0.12% (95% CI; 0.09, 0.15). High-grade dysplasia should be managed aggressively, including the possibility for surgical resection. Early metastases occur in adjacent or regional lymph nodes. Predictors, such as tumor markers (TP53), may indicate potential progression to malignant disease.
Assessment of human epidermal growth factor receptor 2 (HER2) gene and protein expression has been implicated in tumor invasion and lymph node metastasis associated with poorer survival. HER2 is overexpressed more frequently in adenocarcinoma (30%) than in squamous cell carcinoma (13%). HER2 is recommended for all metastatic adenocarcinomas, first using immunohistochemistry score (negative for 0 or 1+ and positive 3+, with reflex FISH for 2+) to confirm.[7][8]
Evaluation
Clinical examination focused on lymph nodes in the supraclavicular and axillary regions is fundamental. Clinicians may choose to start with barium studies on those patients with clinical suspicion, but upper endoscopy with minimally invasive biopsy should be performed to confirm the diagnosis. Multiple biopsies should provide sufficient histological material with a higher accuracy of obtaining a correct diagnosis (one biopsy has 93% accuracy, four biopsies have 95% accuracy, and seven biopsies have 98% accuracy). In vivo staining with Lugol’s iodine is not established.[9][10][11]
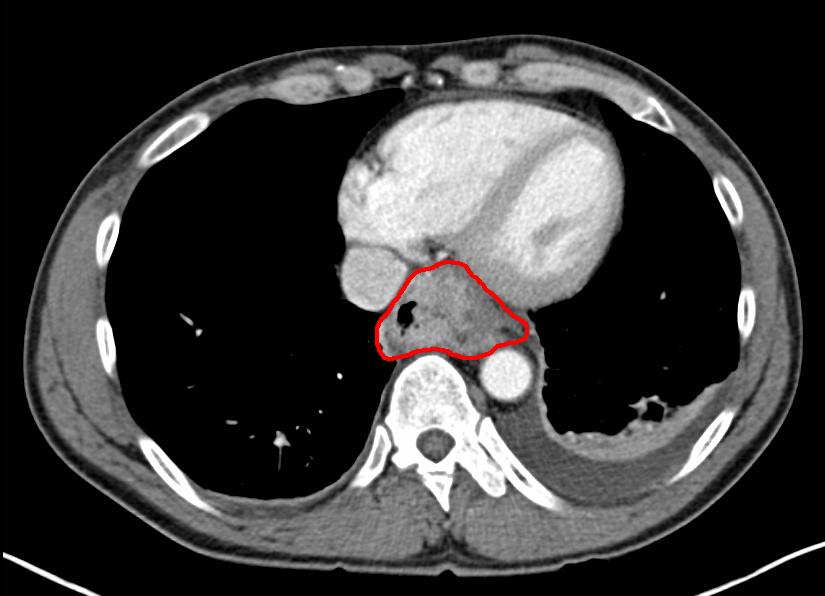
Computed tomography (CT) of the thorax and abdomen should be performed to evaluate the extent of the primary tumor and search for potential liver metastases and celiac lymphadenopathy. However, CT is inconsistent to differentiate tumor depth, has poor lymph node sensitivity, and occasionally fails to detect small metastases, particularly within the peritoneum.
Endoscopic ultrasound (EUS) has become the standard of therapy technique for locoregional staging, with up to 90% accuracy in assessing tumor depth and locoregional and mediastinal lymph nodes involvement. Additionally, EUS allows a fine needle aspiration biopsy of suspicious lymph nodes (more than 1 cm) to confirm the presence of lymph node metastasis which is paramount for appropriate staging. A limitation of EUS is that it cannot transverse tumor stenosis, clinically seen in a third of cases, which can result in an understated tumor. EUS may be used after neoadjuvant therapy to restage local disease before surgery but lacks sensitivity to assess complete response.
To evaluate distance metastases, positron emission tomography CT (PET/CT) has become part of the routine pretreatment diagnostic workup. Adenocarcinoma frequently metastasizes to intrabdominal sites, whereas squamous cell carcinoma is usually intrathoracic. PET allows the detection of occult sites of distant metastatic spread and spares the patient the morbidity of an aggressive local-regional treatment approach when unnecessary, as in up to 20% of cases. PET/CT may be clinically useful in patients after induction therapy for the locally advanced disease to help exclude patients from sequential surgery if metastatic disease is found. This occurs in 8% of patients.
The use of diagnostic laparoscopy for resectable disease continues to be controversial and not routinely recommended. Prior tumor, node, metastasis (TNM) staging provided separate esophageal squamous cell carcinoma and adenocarcinoma staging, but the eighth edition in 2017 grouped them back together. A major change is that EGJ tumors will be staged as esophageal if epicenter in origin and less than 2 cm into the proximal stomach (previously 5 cm). EGJ are sub-classified by Siewert et al. depending on the distance to the anatomic junction into type I (less than 1 cm), II (1 to 2 cm), and III (more than 2 cm), the last occurring in more than 66% of cases. The number of lymph nodes is more important than location. Regardless of the histology, half of the patients will present with locally advanced or metastatic disease.
See heading levels below:
- Level 1: These are the headings already established in the article
- Example in the attached: Fundamentals
- Level 2: Title-Cased and Bold
- Examples in the attached: Dissolution and Effect of Temperature and Pressure on Solubility
- Level 3: Sentence-Cased and Bold
- Examples in the attached: Increasing solubility with increasing temperature, Decreasing solubility..., Effect of temperature...
- Level 4: Sentence-Cased with a colon - you must bring the information below this heading up behind the colon unless it is a bulleted list. You can bold this level or leave it as normal text, depending on your preference and understanding.
Example:
Introduction [Level 1 preprogrammed in the template]
Grocery List [Level 2]
Fruits and vegetables [Level 3]
Green beans: Buy canned beans for casserole. [Level 4]
Gala apples: Use to make pie.
Treatment / Management
Accurate preoperative staging will guide the most appropriate treatment selection.[1][12][13] The general recommendations are as follows:
- Endoscopic resection for superficial, limited mucosa disease (less than T1a)
- direct surgical resection with lymphadenectomy for lesions penetrating the submucosa with negative lymph nodes (more than T1b)
- neoadjuvant chemoradiation of resectable lesions invading muscularis propria with positive lymph nodes (less than T2N1)
- palliative systemic therapy for those locally advanced unresectable or metastatic disease
Endoscopic Resection
Routine endoscopic surveillance has contributed to an increase in the incidence of superficial esophageal cancer. Lesions limited to the lamina propria or muscularis mucosae may be candidates for endoscopic resection (ER). Patients who have an invasion of submucosa or muscularis mucosae with lymphovascular invasion are not candidates for ER due to an increased risk of lymph node metastasis. ER alternative techniques are endoscopic mucosal resection or endoscopic submucosal dissection, or endoscopic ablation (cryoablation, radiofrequency ablation, and photodynamic therapy). No randomized clinical trial has compared these techniques. ER is reserved for a center of excellence, interest in pursuing esophagus sparing techniques, high-risk surgical candidates, or elderly patients with multiple comorbid medical conditions. Other esophageal factors that preclude patients from ER are large size lesions (greater than 2 cm), presence and magnitude of Barrett’s esophagus, and other esophageal diseases, for example, varices. Patients who undergo ER will require extended and close follow-up. Patients who are not candidates for ER but are medically fit should be offered esophagectomy; otherwise, chemotherapy and radiation could be an option for patients unfit for surgery.
Surgical Resection
Localized resectable esophageal cancers comprise approximately 22% of all cases, and those presenting with regional lymph node spread comprise another 30%. The goal of surgical resection is curative. The first-line esophagectomy is offered to T1N0M0 (not endoscopic resection candidate) and selected T2N0M0. Neoadjuvant chemoradiation therapy (CRT) followed by esophagectomy is offered to T2 with positive disease node, T3, and selected T4a disease without metastasis. Relative exclusion criteria for esophagectomy include elderly patients (offered to selected patients) and high-risk patients with comorbid medical conditions. The presence of metastatic disease to other organs or extra-regional lymph nodes is an absolute contraindication to esophagectomy. Surgical procedures are divided accordingly to the anatomical position of esophageal cancer. Cervical esophageal cancer usually requires resection of portions of the larynx, pharynx, thyroid, and proximal esophagus with lower esophagus preservation. Thoracic esophageal cancer will include a total esophagectomy (cervical esophagogastrostomy) with radical two-field lymph node dissection and jejunostomy feeding tube placement. EGJ cancer will involve total esophagectomy and partial or extended gastrectomy. Thoracic cancer resection for the middle to lower esophagus can be divided into three major techniques in the United States: transhiatal, transthoracic (Ivor-Lewis), and tri-incisional esophagectomy. Esophagectomy guidelines recommend at least 15 lymph node resection for adequate staging, and this leads to s significant reduction in mortality (5-year disease-specific survival; 55% less than 11 nodes were resected, 66% for 11 to 17 nodes resected, and 75% more than 18 nodes resected). A positive circumferential resection margin has higher overall mortality compared to the negative (OR 4.02, 2.25 to 7.20, p < 0.001). Reported surgery mortality rates should be less than 5%, and a 5-year survival rate ranges from 5% to 34%. Thoracic, minimally invasive esophagectomy with abdominal laparoscopic intervention offers a surgical recovery advantage with promising better oncologic outcomes over an open thoracotomy and abdominal laparotomy procedure with an experienced surgeon at a center of excellence. Patients’ nutritional status on esophageal cancer complicated by dysphagia before and after surgery should be monitored and should be palliated with esophageal stents, lasers therapy, endoscopic dilation, and gastric/jejunal feeding tube when necessary and feasible.
Neoadjuvant Therapy
In the setting of disease localized to the primary site and regional nodes, the use of chemotherapy (CT) or radiation therapy (RT) alone has resulted in a significant improvement in outcome. Radiation therapy, before or after surgery, has been associated with tumor cytoreduction, improved swallowing, and local-regional tumor control, but the combination did not improve survival over surgery alone. Neoadjuvant chemotherapy (without radiation therapy) provides a significant survival benefit over surgery alone; however, it has an uncertain benefit on local control, and results are extrapolated mainly from data. Tri-modality treatment (concomitant chemotherapy and radiation therapy followed by surgery) provides a survival benefit compared with surgery alone (CROSS trial). The addition of chemotherapy is designed to treat micrometastases and enhance the local effects of radiation, providing better surgical outcomes (pathological complete response [pCR] and complete resections [R0]).
RTOG 85-01 is an original landmark clinical trial performed by Herskovic and the first to demonstrate the benefit of chemoradiation therapy, which is currently the standard of care. Patients with locoregional thoracic esophageal cancer (90% squamous cell carcinoma histology; T1-3, N0-1, M0) were randomly assigned to receive either radiation therapy alone (64 Gy in 32 fractions over 6.5 weeks) or chemoradiation therapy (2 cycles of infusional 5-FU [1000 mg/m2 per day, days 1 to 4, weeks 1 and 5] plus cisplatin [75 mg/m2 day 1 of weeks 1 and 5] and radiation therapy [50 Gy in 25 fractions over 5 weeks]). RTGO was closed prematurely after an interim analysis showed 27% of patients were alive at 5 years in the group that received chemoradiation therapy, and none of the patients who received radiation therapy alone were alive at 5 years. Further analysis showed 46% of patients in chemoradiation therapy had no recurrence at 12 months. The results of the study made chemoradiation therapy the standard of care for an unresectable disease or in patients who cannot undergo surgery. RTOG 85-01 led to a series of trials designed to confirm this positive result. INT 0123 trial was the follow-up trial to RTGO 85-01, which compared a higher radiation therapy dose (64.8 Gy) to the standard dose (50.4 Gy), plus 5-FU/CIS in both arms, found no significant difference in median overall survival (mOS).
The Dutch CROSS phase III trial confirmed the superiority of a neoadjuvant chemoradiation therapy approach compared with surgery alone for patients with localized esophageal cancer. The study included 368 patients (23% squamous cell carcinoma, 75% adenocarcinoma, 2% other; T2-3, N0-1, M0; majority distal esophageal, 11% EGJ) who were randomly assigned to receive preoperative chemoradiation therapy with weekly paclitaxel 50 mg/m2 plus carboplatin [AUC] of 2 plus concurrent radiation therapy (41.4 Gy over 5 weeks) or surgery alone. The neoadjuvant chemoradiation therapy led to a R0 of 92% and pCR rate of 29%. At median follow-up of 32 months, mOS was significantly better in the chemoradiation therapy arm (HR, 0.657; 95% CI; 0.50, 0.87 [p = 0.003]). The mOS was 49 months in the chemoradiation therapy arm versus 24 months in the surgery alone arm. Five-year survival rate was 47% in the tri-modality arm and 34% in the surgery-alone arm. Importantly, the results appeared to be more convincing in squamous cell sarcoma (pCR 49%) than in adenocarcinoma (23%). Chemoradiation therapy was well tolerated, with a grade of more than 3 in 7% of patients with less than 13% for hematologic and non-hematologic toxicities. In contrast, the FFCD 9901 trial failed to show benefit with 5-FU/CIS with surgery, but rather, there was a significant increase in postoperative mortality compared to surgery alone. CALGB 9781 trial was a prospective randomized trial that would have favored tri-modality therapy (5-Fu/CIS followed by surgery) versus surgery alone but failed to enroll patients. The largest meta-analysis included 12 randomized clinical trials (including the FFCD 9901, CALGB 9781, and CROSS trials) that provided strong evidence for a survival benefit of neoadjuvant chemoradiation therapy (either concurrent or sequential) over surgery alone for esophageal or EGJ cancer across histologic subtypes.
The advantage of neoadjuvant chemoradiation therapy over neoadjuvant chemotherapy has not been established, possibly due to a majority of patients enrolled in comparative trials had squamous cell carcinoma histology that is known to be more sensitive to chemoradiation therapy than adenocarcinoma. However, the Medical Research Council Adjuvant Gastric Infusional Chemotherapy (MAGIC) trial, which compared perioperative chemotherapy (consisted of three preoperative and three postoperative cycles of intravenous epirubicin [E: 50 mg per square meter of body-surface area] and cisplatin [C: 60 mg per square meter] on day 1, and a continuous intravenous infusion of fluorouracil [F: 200 mg per square meter per day] for 21 days) with surgery alone for patients with adenocarcinoma of gastric, GEJ and esophageal cancers, significantly improved mOS (HR, 0.75; 95% CI; 0.60, 0.93 [p = 0.009]) and progression-free survival (HR, 0.66; 95% CI; 0.53, 0.81 [p = < 0.001]) for patients who received perioperative ECF. Twenty-six percent of patients in this trial had esophageal and GEJ cancers, and multivariate subgroup analyses indicated a survival benefit from perioperative chemotherapy, at least for GEJ cancers. Thus, perioperative chemotherapy with ECF should be considered for patients with GEJ cancers who are not optimal candidates for chemoradiation therapy.
In the absence of medical contraindications, most patients in the United States with localized esophageal cancers are receiving neoadjuvant chemoradiation therapy followed by surgery. This practice is so prevalent that clinical trials that try to enroll patients in a surgery-alone arm or compare optimized perioperative chemotherapy with neoadjuvant chemoradiation therapy have major accrual problems.[14][15][16]
Adjuvant Therapy
Patients with R0 resection of node-positive or T4 esophageal cancers who have not received neoadjuvant therapy are routinely offered adjuvant chemotherapy or chemoradiation therapy with no randomized trial data to support or refute either approach. Adjuvant chemoradiation therapy for gastric or GEJ has become a standard based on significantly better OS of 36 months compared to observation of 27 months from the SWOG9008/INT 0116 trial (20% GEJ adenocarcinoma).
Systemic Treatment
The treatment goals for metastatic esophageal cancer are symptom palliation, improved quality of life, and prolonged survival. Therapy is guided by symptom burden, performance status, comorbidities, histologic type, tumor-targeted biology, and patient preference. Several chemotherapy agents have demonstrated some activity against esophageal cancer, including fluoropyrimidines (fluorouracil [FU] and capecitabine), platinum agents (cisplatin and oxaliplatin), taxanes (paclitaxel, docetaxel), irinotecan, irinotecan, mitomycin-C, anthracyclines, and, to a lesser extent, methotrexate, vinorelbine, and gemcitabine. Treatment commonly involves a combination of two or three drugs with a response rate as high as 65%, modestly translating to survival of weeks to a few months or, less frequently, as single-agent therapy ranging from 10% to 40%, typically with survival of fewer than 6 months. Palliation therapy may include local interventions (e.g., esophageal stent) and radiation therapy with or without chemotherapy, particularly in scenarios such as dysphagia or bleeding. If available, enrollment in clinical trials is preferred.
All patients with esophageal adenocarcinoma who are chemotherapy candidates should have their tumor assayed for HER2 overexpression. HER2-positive adenocarcinoma can have trastuzumab added to a cytotoxic chemotherapy doublet backbone (most commonly fluoropyrimidine plus platinum). Non-HER2 or squamous cell carcinoma fit patients can be offered doublet therapy (e.g., oxaliplatin plus leucovorin and infusional FU [FOLFOX], oxaliplatin plus capecitabine [XELOX], irinotecan plus leucovorin and FU [FOLFIRI] or FU plus cisplatin) over triplet regimen (e.g., epirubicin plus cisplatin and infusional FU [ECF], epirubicin, cisplatin and capecitabine [ECX], epirubicin plus cisplatin and capecitabine [EOX], docetaxel, cisplatin, infusional FU [DCF] or modified DCF due to treatment toxicities. Poor performance or elderly patients may be appropriate for single agents (e.g., leucovorin-modulated fluorouracil alone, single-agent capecitabine, single-agent irinotecan, or low-dose weekly taxanes). Docetaxel and irinotecan have shown a survival benefit for second-line chemotherapy. Nevertheless, there is no optimal standard of care.
The REAL-2 trial compared four triplet regimen (ECF, ECX, EOF or EOX), and results showed outcomes were comparable when capecitabine was substituted for infusional FU and EOX. This was preferred due to a longer mOS of 11.2 months compared to 9.9 months with ECF (HR, 0.80; 95% CI; 0.66, 0.97 [p = 0.02]). Patients on oral capecitabine should not take proton pump inhibitors due to inferior absorption on less acid gastric pH. A multinational TAX-325 trial compared DCF (or Taxane cisplatin FU [TCF]) with cisplatin and FU, favoring docetaxel addition for a significant response rate (37% versus 25%), time to progression (5.6 versus 3.7 months), and 2-year survival (18% versus 9%); although, higher toxicity rates requiring supportive granulocyte-colony stimulating factor were seen.
Different targeted agents added to cytotoxic backbone have been investigated in clinical trials with unfavorable results in first-line therapy. Bevacizumab failed to improve overall survival, epidermal growth factor receptor monoclonal antibodies exhibited a detrimental effect, and ramucirumab had no significant impact. Trastuzumab was added to standard chemotherapy in HER2-overexpressing gastric and GEJ cancers and showed improved overall and progression-free survival (PFS) compared with chemotherapy alone. The ToGA was a phase III trial that compared six courses of cisplatin plus either infusional FU or capecitabine with and without trastuzumab. Patients received trastuzumab 8 mg/kg loading dose, then 6 mg/kg every 3 weeks until disease progression on HER2-positive either by IHC 3+ or FISH+ on a majority gastric adenocarcinoma (80%). The primary endpoint of mOS was significantly better with trastuzumab 13.8 versus 11.1 months (p = 0.046). Trastuzumab, in combination with chemotherapy, became a new standard of care for patients with HER2-positive advanced or metastatic GEJ and gastric. Higher trastuzumab dose (10 mg/kg) did not improve efficacy in a phase III HELOISE trial. Trastuzumab candidates should be evaluated for cardiac eligibility criteria before invasive procedures or starting treatment.
The vascular endothelial growth factor receptor 2 monoclonal antibody ramucirumab dosed at 8 mg/kg intravenously (IV) every 2 weeks showed a modest survival benefit of 9.6 months when combined with paclitaxel versus paclitaxel alone dosed at 80 mg/m on days 1, 8, and 15 of each 28-day cycle alone (7.4 months), RAINBOW trial. Ramucirumab also showed a modest survival benefit in the REGARD trial when used as a single agent (5.2 months) versus best supportive care (3.8 months). The two trials mentioned above were both phase III clinical trials in patients with advanced gastroesophageal cancers who progressed first-line chemotherapy on a fluoropyrimidine and platinum agent. Other second-line targeted therapy agents with clinical improvement in survival outcomes in clinical trials are apatinib (an oral VEGFR-2 inhibitor with a median of 6.5 versus 4.7 months with placebo), regorafenib (an oral multikinase inhibitor with a median of 5.8 versus 4.5 months with placebo). Bevacizumab, sunitinib, sorafenib, aflibercept, gefitinib, and everolimus had no significant overall survival benefit with other secondary outcome improvements. A clinical trial selected patients with low expression of ataxia telangiectasia protein had a significant survival benefit from paclitaxel plus olaparib (an oral active poly-ADP ribose polymerase inhibitor) with mOS not reached compared to paclitaxel plus placebo of 8.2 months, and a phase III trial is ongoing. A 2017 study hypothesized that microsatellite instability-high (MSI-H) and deficient mismatch repair (dMMR) tumors might be susceptible to immune checkpoint inhibition. The frequency of dMMR or MSI-H has been reported as high as 7% for esophageal/GEJ adenocarcinoma. Eighty-six selected dMMR patients with 12 different tumor types (including refractory advanced or metastatic esophageal carcinoma) who received pembrolizumab achieved 53% objective response and 21% complete response, with subsequent FDA approval for all solid tumors with those characteristics.[17][18]
In 2021, FDA approved the antibody-drug conjugate fam-trastuzumab deruxtecan for the treatment of advanced HER2-positive gastric or GEJ adenocarcinoma after prior trastuzumab-containing chemotherapy.[19]
Enhancing Healthcare Team Outcomes
Esophageal cancer is a deadly malignancy with very low survival, even with treatment. Over the past few decades, the rates of squamous cell cancers have declined, but the rates of adenocarcinoma have gradually increased, chiefly because of GERD. The care of a patient with esophageal cancer is interprofessional. The inability to eat affects every organ in the body. At presentation, the majority of patients are severely emaciated. The role of the nurse in looking after these patients after surgery and teaching about prevention cannot be overemphasized. In the postoperative period, the nurse is responsible for initiating J-tube feeds, weighing the patient, and monitoring for side effects. Many patients develop a whole host of complications that gradually leads to poor quality of life. A dietitian should be involved in the care of these patients to ensure they are receiving adequate calories. The key preventive measure that nurses should emphasize is the discontinuation of tobacco and abstaining from alcohol. In addition, patients should maintain a healthy body weight and get GERD treated. Since many of these patients are not able to eat, the pharmacist is responsible for ensuring that the medications available are in liquid form so that they can be administered via the J-tube. Since the patients are weak and frail, consultation with a physical therapist and an occupational therapist is recommended.[20][21][22] [Level 5]
Outcomes
For both adenocarcinoma and squamous cell cancer, the prognosis depends on the stage. In general, the survival rates per stage are similar for both cancers.
Once a patient has positive lymph nodes, survival is decreased. Less than 20% of patients with esophageal cancer are alive at 5 years, with stage IV having the worst prognosis. [Level 2]
Surgery has slightly increased survival rates, but the postoperative complications are often serious, and the quality of life is poor.[14][6] [Level 5]