Introduction
The nerves of the pelvis and lower limbs originate from sympathetic, parasympathetic, and somatic nerves. The sympathetic component comes from roots T12 through L2 and the parasympathetic from roots S2 through S4. The sympathetic component reaches the pelvis through the superior hypogastric plexus. These nerves are known as sacral splanchnic nerves. The parasympathetic components are referred to as pelvic splanchnic nerves. Somatic innervation for the pelvis arises from nerve roots S2 through S4. Somatic innervation contains two parts, motor and sensory. Afferent fibers carry sensory information while efferent fibers carry motor.
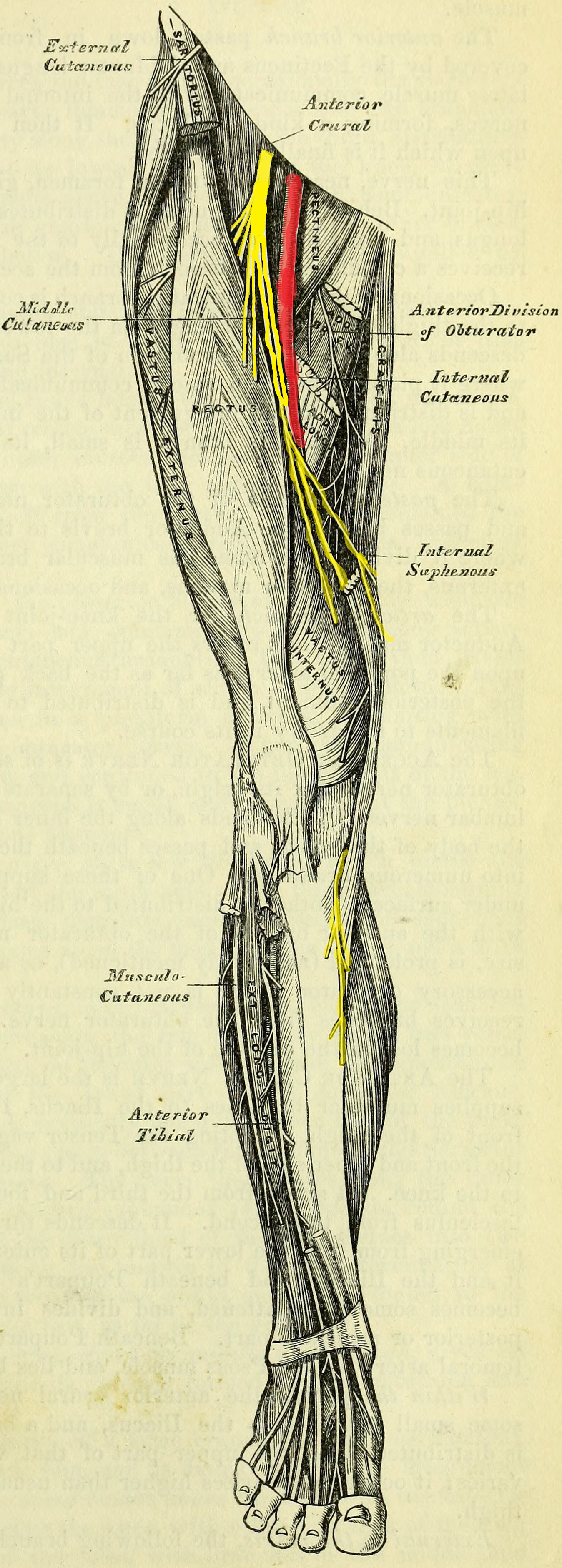
Nerve roots L2 through L4 and L4 through S3 supply all the motor and some sensory information for the lower limbs. Generally, nerves with motor information supply all muscles contained within a given compartment. For example, The tibial nerve supplies the muscles that are within the posterior compartment of the lower extremities. The cutaneous sensation is in a dermatomal distribution.[1]
Structure and Function
The nerves of the pelvis perform both voluntary and involuntary functions. The parasympathetic nerves control opening and closing of sphincters, regulate emptying of the bladder, influence sexual functions such as achieving and maintaining erections, and influence bowel motility. The distal one-third of the transverse colon receives its parasympathetic innervation from the pelvic splanchnic nerves. Parasympathetic fibers are also responsible for transmitting the sensation of pain. Sacral splanchnic nerves supply efferent information to pelvic vessels and organs. Their origin is outside the pelvis and so must be reached via the hypogastric plexuses. Somatic nerves of the pelvis supply purely motor, purely sensory, or both motor and sensory information. The superior and inferior gluteal nerves supply motor information to the gluteal muscles and the tensor fascia lata. The lateral femoral cutaneous nerve provides sensation to the anterior and lateral aspects of the thigh through an anterior and posterior branch. The femoral nerve supplies the anterior compartment and a few medial compartment muscles with motor information. The femoral nerve also supplies the anterior and medial aspects of the thigh with cutaneous sensation. It then continues as the saphenous nerve to provide cutaneous sensation to the lower extremity which will be discussed in more detail later. The obturator nerve sends motor information to the medial compartment of the thigh through posterior and anterior branches. The genitofemoral nerve is composed of 2 separate branches; the genital branch and the femoral branch. The genital branch runs within the spermatic cord and supplies motor information to the scrotum, specifically the cremasteric muscle. The femoral branch supplies cutaneous sensation to the inner aspect of the upper thigh. The ilioinguinal nerve travels through the inguinal canal outside of the spermatic cord and provides sensation to the scrotum, labia, and the upper anterior-medial thigh.
The sciatic nerve is the largest nerve in the body and arises from L4 through S3 nerve roots. It provides motor innervation to all muscles of the posterior thigh as well as the leg via its continuation as the tibial nerve. The sciatic nerve terminates after it bifurcates into the tibial and common fibular nerve. The common fibular nerve bifurcates in superficial and deep fibular nerve. The superficial fibular nerve supplies the lateral compartment of the leg with motor innervation and the deep fibular supplies the anterior compartment. The superficial fibular nerve supplies sensory information to the dorsal aspect of the foot and the deep provides sensation to the area of skin between the first and second metatarsals. The tibial nerve supplies all motor information to the posterior compartment muscles of the leg. The tibial nerve also gives off a branch known as the sural nerve which provides sensation to the posterior-lateral aspect of the leg.[1][2]
Embryology
Nerves of the pelvis and lower limbs develop with the rest of the nervous system. This process begins around week 4 of developing fetuses. Neural crest cells reside at the age of the neural plate and dorsal to the neural tube. The cells migrate throughout the embryo eventually forming peripheral nerve cells.[3]
Surgical Considerations
Many considerations should be accounted for when performing surgery on the areas, particularly the pelvis. The pelvis is a difficult space to enter as the pelvic bones limit access safely, extensive vasculature and nerve plexuses reside here, as well as organs necessary for reproduction. The lateral femoral cutaneous nerve is frequently injured in hip replacement procedures; the anterior approach puts the nerve at highest risk for injury. Patient's will have numbness in the anterolateral aspect of the thigh. When casting or splinting the lower limbs after surgery, many patients can experience foot drop and loss of sensation on the dorsal aspect of the foot. Wrapping the cast too tight and post-procedural swelling can cause the fibular nerve to be trapped between the cast and the head of the fibula leading to an inability of the nerve to transmit information.
Clinical Significance
There are common pathologies seen due to nerve insults. Piriformis syndrome is a common pathology that is the result of sciatic nerve entrapment beneath the piriformis muscle. Sciatic nerve entrapment causes shooting pain, numbness, and weakness in the lower limbs. Since the sciatic nerve runs beneath the piriformis muscle as well as the nerves large size, this syndrome is common among those who sit for prolonged periods of time such as students, truck drivers, and secretaries. Another common pathology results from superior gluteal nerve iatrogenic injury. Sciatic nerve blockade requires penetration of the gluteal muscles for administration, and if not performed correctly, the risk of injury to the superior gluteal nerve is increased. Superior gluteal nerve injury results in gluteus medius and minimus paralysis. This paralysis causes the patient's hip to drop contralateral to the side of nerve injury. Lead poisoning leads to neuropathy of peripheral nerves. The deep fibular nerve is particularly susceptible to lead-induced axonal degeneration, therefor foot-drop is a common finding in patients with severe lead poisoning. Since the genitofemoral nerve is composed of 2 branches, its sensory component is used to evaluate its motor component. Stroking of the inner aspect of the thigh causes stimulation of the genital branch and therefore contraction of the cremasteric muscle and elevation of the testes. This is a standard physical exam technique when evaluating the scrotum and testes for pathology.[4][5][6]