[1]
ALIMUDDIN M. Normal intra-ocular pressure. The British journal of ophthalmology. 1956 Jun:40(6):366-72
[PubMed PMID: 13355942]
[2]
Salvetat ML, Zeppieri M, Tosoni C, Brusini P, Medscape. Baseline factors predicting the risk of conversion from ocular hypertension to primary open-angle glaucoma during a 10-year follow-up. Eye (London, England). 2016 Jun:30(6):784-95. doi: 10.1038/eye.2016.86. Epub 2016 May 13
[PubMed PMID: 27174381]
[3]
Popović-Suić S, Sikić J, Vukojević N, Cerovski B, Nasić M, Pokupec R. Target intraocular pressure in the management of glaucoma. Collegium antropologicum. 2005:29 Suppl 1():149-51
[PubMed PMID: 16193700]
[4]
Brusini P, Papa V, Zeppieri M. Canaloplasty in Pseudoexfoliation Glaucoma. Can It Still Be Considered a Good Choice? Journal of clinical medicine. 2022 Apr 30:11(9):. doi: 10.3390/jcm11092532. Epub 2022 Apr 30
[PubMed PMID: 35566656]
[5]
Toneatto G, Zeppieri M, Papa V, Rizzi L, Salati C, Gabai A, Brusini P. 360° Ab-Interno Schlemm's Canal Viscodilation with OMNI Viscosurgical Systems for Open-Angle Glaucoma-Midterm Results. Journal of clinical medicine. 2022 Jan 4:11(1):. doi: 10.3390/jcm11010259. Epub 2022 Jan 4
[PubMed PMID: 35012000]
[6]
Brusini P, Tosoni C, Zeppieri M. Canaloplasty in Corticosteroid-Induced Glaucoma. Preliminary Results. Journal of clinical medicine. 2018 Feb 11:7(2):. doi: 10.3390/jcm7020031. Epub 2018 Feb 11
[PubMed PMID: 29439499]
[7]
Aziz K, Friedman DS. Tonometers-which one should I use? Eye (London, England). 2018 May:32(5):931-937. doi: 10.1038/s41433-018-0040-4. Epub 2018 Feb 19
[PubMed PMID: 29456251]
[8]
McAllister F, Harwerth R, Patel N. Assessing the True Intraocular Pressure in the Non-human Primate. Optometry and vision science : official publication of the American Academy of Optometry. 2018 Feb:95(2):113-119. doi: 10.1097/OPX.0000000000001171. Epub
[PubMed PMID: 29370024]
[9]
Stamper RL. A history of intraocular pressure and its measurement. Optometry and vision science : official publication of the American Academy of Optometry. 2011 Jan:88(1):E16-28. doi: 10.1097/OPX.0b013e318205a4e7. Epub
[PubMed PMID: 21150677]
[10]
Brusini P, Salvetat ML, Zeppieri M. How to Measure Intraocular Pressure: An Updated Review of Various Tonometers. Journal of clinical medicine. 2021 Aug 27:10(17):. doi: 10.3390/jcm10173860. Epub 2021 Aug 27
[PubMed PMID: 34501306]
[11]
Reis TF, Paula JS, Furtado JM. Primary glaucomas in adults: Epidemiology and public health-A review. Clinical & experimental ophthalmology. 2022 Mar:50(2):128-142. doi: 10.1111/ceo.14040. Epub 2022 Jan 26
[PubMed PMID: 35037725]
[12]
Teo ZL, Soh ZD, Tham YC, Yu M, Chee ML, Thakur S, Nongpiur ME, Koh V, Wong TY, Aung T, Cheng CY. Six-Year Incidence and Risk Factors for Primary Angle-Closure Disease: The Singapore Epidemiology of Eye Diseases Study. Ophthalmology. 2022 Jul:129(7):792-802. doi: 10.1016/j.ophtha.2022.03.009. Epub 2022 Mar 16
[PubMed PMID: 35306094]
[13]
Wijnants D, Stalmans I, Vandewalle E. The Effects of Intranasal, Inhaled and Systemic Glucocorticoids on Intraocular Pressure: A Literature Review. Journal of clinical medicine. 2022 Apr 3:11(7):. doi: 10.3390/jcm11072007. Epub 2022 Apr 3
[PubMed PMID: 35407615]
[14]
Paulson C, Thomas SC, Gonzalez O, Taylor S, Swiston C, Herrick JS, McCoy L, Curtin K, Chaya CJ, Stagg BC, Wirostko BM. Exfoliation Syndrome in Baja Verapaz Guatemala: A Cross-Sectional Study and Review of the Literature. Journal of clinical medicine. 2022 Mar 24:11(7):. doi: 10.3390/jcm11071795. Epub 2022 Mar 24
[PubMed PMID: 35407402]
Level 2 (mid-level) evidence
[15]
Hou X, Guo X, Cui Z, Wang Y, Zhou J, Hu D. Value of ocular trauma score in predicting the incidence of secondary glaucoma after closed globe injury. European journal of ophthalmology. 2022 Sep:32(5):3005-3011. doi: 10.1177/11206721211055628. Epub 2021 Nov 29
[PubMed PMID: 34841932]
[17]
Panta Sitoula R, Gurung J, Anwar A. Primary Congenital Glaucoma among the Children Under 3 Years of Age in the Outpatient Department in a Tertiary Care Hospital: A Descriptive Cross-sectional Study. JNMA; journal of the Nepal Medical Association. 2021 Sep 11:59(241):867-870. doi: 10.31729/jnma.5889. Epub 2021 Sep 11
[PubMed PMID: 35199734]
Level 2 (mid-level) evidence
[18]
Fogagnolo P, Figus M, Frezzotti P, Iester M, Oddone F, Zeppieri M, Ferreras A, Brusini P, Rossetti L, Orzalesi N. Test-retest variability of intraocular pressure and ocular pulse amplitude for dynamic contour tonometry: a multicentre study. The British journal of ophthalmology. 2010 Apr:94(4):419-23. doi: 10.1136/bjo.2009.165142. Epub 2009 Oct 14
[PubMed PMID: 19833616]
[19]
Walker HK, Hall WD, Hurst JW, Alguire PC. Tonometry. Clinical Methods: The History, Physical, and Laboratory Examinations. 1990:():
[PubMed PMID: 21250066]
[20]
Blumberg MJ, Varikuti VNV, Weiner A. Real-world comparison between the Tonopen and Goldmann applanation tonometry in a university glaucoma clinic. International ophthalmology. 2021 May:41(5):1815-1825. doi: 10.1007/s10792-021-01742-z. Epub 2021 Mar 2
[PubMed PMID: 33651312]
[21]
Chou R, Selph S, Blazina I, Bougatsos C, Jungbauer R, Fu R, Grusing S, Jonas DE, Tehrani S. Screening for Glaucoma in Adults: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2022 May 24:327(20):1998-2012. doi: 10.1001/jama.2022.6290. Epub
[PubMed PMID: 35608575]
Level 1 (high-level) evidence
[22]
Wachtl J, Töteberg-Harms M, Frimmel S, Roos M, Kniestedt C. Correlation Between Dynamic Contour Tonometry, Uncorrected and Corrected Goldmann Applanation Tonometry, and Stage of Glaucoma. JAMA ophthalmology. 2017 Jun 1:135(6):601-608. doi: 10.1001/jamaophthalmol.2017.1012. Epub
[PubMed PMID: 28494071]
[23]
Salvetat ML, Zeppieri M, Tosoni C, Brusini P. Comparisons between Pascal dynamic contour tonometry, the TonoPen, and Goldmann applanation tonometry in patients with glaucoma. Acta ophthalmologica Scandinavica. 2007 May:85(3):272-9
[PubMed PMID: 17488456]
[24]
Aldaas K, Challa P, Weber DJ, Fleischman D. Infections and glaucoma. Survey of ophthalmology. 2022 May-Jun:67(3):637-658. doi: 10.1016/j.survophthal.2021.08.009. Epub 2021 Sep 4
[PubMed PMID: 34487741]
Level 3 (low-level) evidence
[26]
Rao A, Gawas L. Atypical associations of viral anterior uveitis with glaucoma-a series of challenging scenarios with review of literature. Seminars in ophthalmology. 2021 Nov 17:36(8):605-613. doi: 10.1080/08820538.2021.1890789. Epub 2021 Mar 18
[PubMed PMID: 33734824]
[27]
Salvetat ML, Zeppieri M, Miani F, Tosoni C, Parisi L, Brusini P. Comparison of iCare tonometer and Goldmann applanation tonometry in normal corneas and in eyes with automated lamellar and penetrating keratoplasty. Eye (London, England). 2011 May:25(5):642-50. doi: 10.1038/eye.2011.60. Epub 2011 Mar 25
[PubMed PMID: 21436848]
[28]
Gismondi M, Salati C, Salvetat ML, Zeppieri M, Brusini P. Short-term effect of intravitreal injection of Ranibizumab (Lucentis) on intraocular pressure. Journal of glaucoma. 2009 Dec:18(9):658-61. doi: 10.1097/IJG.0b013e31819c4893. Epub
[PubMed PMID: 20010243]
[29]
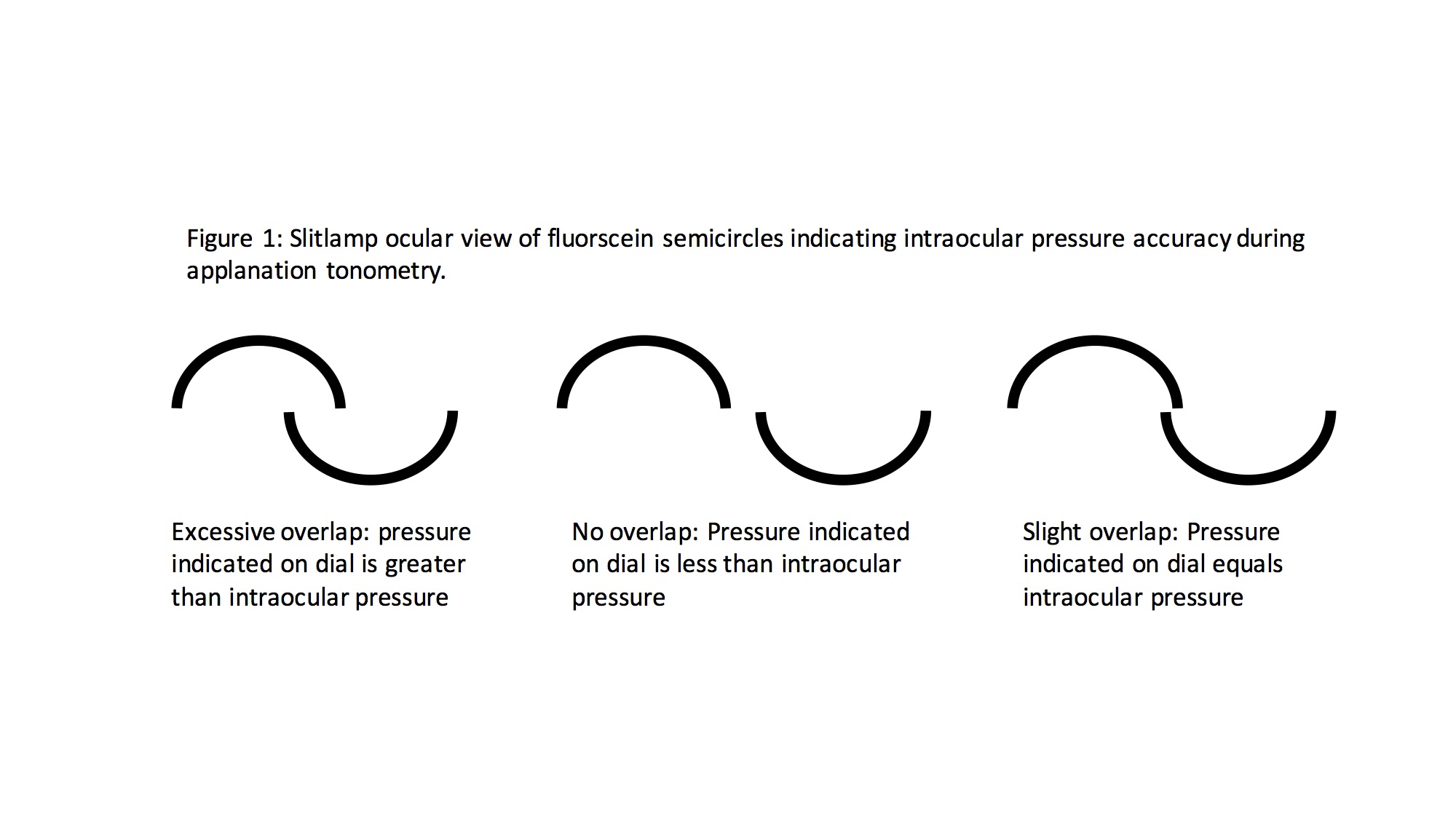
Stevens S, Gilbert C, Astbury N. How to measure intraocular pressure: applanation tonometry. Community eye health. 2007 Dec:20(64):74-5
[PubMed PMID: 18330450]
[30]
Stewart RM, Wishart PK, Kaye SB. Overestimation of Intraocular Pressure by Goldmann Applanation Tonometry Without Astigmatic Correction. JAMA ophthalmology. 2016 Mar:134(3):e153691. doi: 10.1001/jamaophthalmol.2015.3691. Epub 2016 Mar 10
[PubMed PMID: 26967752]
[31]
Arend N, Hirneiss C, Kernt M. [Differences in the measurement results of Goldmann applanation tonometry with and without fluorescein]. Der Ophthalmologe : Zeitschrift der Deutschen Ophthalmologischen Gesellschaft. 2014 Mar:111(3):241-6. doi: 10.1007/s00347-013-2843-9. Epub
[PubMed PMID: 23604252]
[32]
GOLDMANN H, SCHMIDT T. [Applanation tonometry]. Ophthalmologica. Journal international d'ophtalmologie. International journal of ophthalmology. Zeitschrift fur Augenheilkunde. 1957 Oct:134(4):221-42
[PubMed PMID: 13484216]
[33]
Okafor KC, Brandt JD. Measuring intraocular pressure. Current opinion in ophthalmology. 2015 Mar:26(2):103-9. doi: 10.1097/ICU.0000000000000129. Epub
[PubMed PMID: 25594767]
Level 3 (low-level) evidence
[34]
Lubbad A, Oluwatoba-Popoola I, Haar M, Framme C, Bajor A. The influence of corneal density and thickness on tonometry measurement with goldmann applanation, non-contact and iCare tonometry methods. International ophthalmology. 2022 Jul:42(7):2167-2174. doi: 10.1007/s10792-022-02216-6. Epub 2022 Jan 13
[PubMed PMID: 35023013]
[35]
Mark HH. Armand Imbert, Adolf Fick, and their tonometry law. Eye (London, England). 2012 Jan:26(1):13-6. doi: 10.1038/eye.2011.248. Epub 2011 Oct 21
[PubMed PMID: 22020170]
[36]
Zeppieri M, Brusini P, Miglior S. Corneal thickness and functional damage in patients with ocular hypertension. European journal of ophthalmology. 2005 Mar-Apr:15(2):196-201
[PubMed PMID: 15812759]
[37]
Bilgeç MD, Atalay E, Sözer Ö, Gürsoy H, Bilgin M, Yıldırım N. The influence of corneal geometrical and biomechanical properties on tonometry readings in keratoconic eyes. International ophthalmology. 2020 Apr:40(4):849-857. doi: 10.1007/s10792-019-01248-9. Epub 2019 Dec 2
[PubMed PMID: 31792851]
[38]
Arora R, Bellamy H, Austin M. Applanation tonometry: a comparison of the Perkins handheld and Goldmann slit lamp-mounted methods. Clinical ophthalmology (Auckland, N.Z.). 2014:8():605-10. doi: 10.2147/OPTH.S53544. Epub 2014 Mar 26
[PubMed PMID: 24707165]
[39]
Grolman B. A new tonometer system. American journal of optometry and archives of American Academy of Optometry. 1972 Aug:49(8):646-60
[PubMed PMID: 4506671]
[40]
Kamel K, Dervan E, Falzon K, O'Brien C. Difference in intraocular pressure measurements between non-contact tonometry and Goldmann applanation tonometry and the role of central corneal thickness in affecting glaucoma referrals. Irish journal of medical science. 2019 Feb:188(1):321-325. doi: 10.1007/s11845-018-1795-0. Epub 2018 Apr 4
[PubMed PMID: 29616408]
[41]
Parker VA, Herrtage J, Sarkies NJ. Clinical comparison of the Keeler Pulsair 3000 with Goldmann applanation tonometry. The British journal of ophthalmology. 2001 Nov:85(11):1303-4
[PubMed PMID: 11673293]
[42]
Atkinson PL, Wishart PK, James JN, Vernon SA, Reid F. Deterioration in the accuracy of the pulsair non-contact tonometer with use: need for regular calibration. Eye (London, England). 1992:6 ( Pt 5)():530-4
[PubMed PMID: 1286721]
[43]
Kyei S, Assiamah F, Kwarteng MA, Gboglu CP. The Association of Central Corneal Thickness and Intraocular Pressure Measures by Non-Contact Tonometry and Goldmann Applanation Tonometry among Glaucoma Patients. Ethiopian journal of health sciences. 2020 Nov:30(6):999-1004. doi: 10.4314/ejhs.v30i6.18. Epub
[PubMed PMID: 33883845]
[44]
Kouchaki B, Hashemi H, Yekta A, Khabazkhoob M. Comparison of current tonometry techniques in measurement of intraocular pressure. Journal of current ophthalmology. 2017 Jun:29(2):92-97. doi: 10.1016/j.joco.2016.08.010. Epub 2016 Nov 28
[PubMed PMID: 28626817]
[45]
Farhood QK. Comparative evaluation of intraocular pressure with an air-puff tonometer versus a Goldmann applanation tonometer. Clinical ophthalmology (Auckland, N.Z.). 2013:7():23-7. doi: 10.2147/OPTH.S38418. Epub 2012 Dec 27
[PubMed PMID: 23293511]
Level 2 (mid-level) evidence
[46]
Qin X, Tian L, Zhang H, Zhang D, Jie Y, Zhang HX, Li L. Determine Corneal Biomechanical Parameters by Finite Element Simulation and Parametric Analysis Based on ORA Measurements. Frontiers in bioengineering and biotechnology. 2022:10():862947. doi: 10.3389/fbioe.2022.862947. Epub 2022 Apr 13
[PubMed PMID: 35497338]
Level 2 (mid-level) evidence
[47]
ElMallah MK, Asrani SG. New ways to measure intraocular pressure. Current opinion in ophthalmology. 2008 Mar:19(2):122-6. doi: 10.1097/ICU.0b013e3282f391ae. Epub
[PubMed PMID: 18301285]
Level 3 (low-level) evidence
[48]
Zhang H, Sun Z, Li L, Sun R, Zhang H. Comparison of intraocular pressure measured by ocular response analyzer and Goldmann applanation tonometer after corneal refractive surgery: a systematic review and meta-analysis. BMC ophthalmology. 2020 Jan 10:20(1):23. doi: 10.1186/s12886-019-1288-6. Epub 2020 Jan 10
[PubMed PMID: 31924174]
Level 1 (high-level) evidence
[49]
Fujino Y, Murata H, Matsuura M, Nakakura S, Shoji N, Nakao Y, Kiuchi Y, Asaoka R. The Relationship Between Corneal Hysteresis and Progression of Glaucoma After Trabeculectomy. Journal of glaucoma. 2020 Oct:29(10):912-917. doi: 10.1097/IJG.0000000000001581. Epub
[PubMed PMID: 32555063]
[50]
Susanna BN, Ogata NG, Jammal AA, Susanna CN, Berchuck SI, Medeiros FA. Corneal Biomechanics and Visual Field Progression in Eyes with Seemingly Well-Controlled Intraocular Pressure. Ophthalmology. 2019 Dec:126(12):1640-1646. doi: 10.1016/j.ophtha.2019.07.023. Epub 2019 Aug 9
[PubMed PMID: 31519385]
[51]
Kynigopoulos M, Schlote T, Kotecha A, Tzamalis A, Pajic B, Haefliger I. Repeatability of intraocular pressure and corneal biomechanical properties measurements by the ocular response analyser. Klinische Monatsblatter fur Augenheilkunde. 2008 May:225(5):357-60. doi: 10.1055/s-2008-1027256. Epub
[PubMed PMID: 18454372]
[52]
Halkiadakis I, Tzimis V, Gryparis A, Markopoulos I, Konstadinidou V, Zintzaras E, Tzakos M. Evaluation of Corvis ST tonometer with the updated software in glaucoma practice. International journal of ophthalmology. 2022:15(3):438-445. doi: 10.18240/ijo.2022.03.11. Epub 2022 Mar 18
[PubMed PMID: 35310063]
[53]
Salvetat ML, Zeppieri M, Tosoni C, Felletti M, Grasso L, Brusini P. Corneal Deformation Parameters Provided by the Corvis-ST Pachy-Tonometer in Healthy Subjects and Glaucoma Patients. Journal of glaucoma. 2015 Oct-Nov:24(8):568-74. doi: 10.1097/IJG.0000000000000133. Epub
[PubMed PMID: 25318572]
[54]
Yang K, Xu L, Fan Q, Gu Y, Song P, Zhang B, Zhao D, Pang C, Ren S. Evaluation of new Corvis ST parameters in normal, Post-LASIK, Post-LASIK keratectasia and keratoconus eyes. Scientific reports. 2020 Mar 30:10(1):5676. doi: 10.1038/s41598-020-62825-y. Epub 2020 Mar 30
[PubMed PMID: 32231236]
[55]
Bao F, Huang W, Zhu R, Lu N, Wang Y, Li H, Wu S, Lin H, Wang J, Zheng X, Huang J, Li Y, Wang Q, Elsheikh A. Effectiveness of the Goldmann Applanation Tonometer, the Dynamic Contour Tonometer, the Ocular Response Analyzer and the Corvis ST in Measuring Intraocular Pressure following FS-LASIK. Current eye research. 2020 Feb:45(2):144-152. doi: 10.1080/02713683.2019.1660794. Epub 2019 Dec 26
[PubMed PMID: 31869261]
[56]
Nakao Y, Kiuchi Y, Okumichi H. Evaluation of biomechanically corrected intraocular pressure using Corvis ST and comparison of the Corvis ST, noncontact tonometer, and Goldmann applanation tonometer in patients with glaucoma. PloS one. 2020:15(9):e0238395. doi: 10.1371/journal.pone.0238395. Epub 2020 Sep 23
[PubMed PMID: 32966284]
[57]
Luebke J, Bryniok L, Neuburger M, Jordan JF, Boehringer D, Reinhard T, Wecker T, Anton A. Intraocular pressure measurement with Corvis ST in comparison with applanation tonometry and Tomey non-contact tonometry. International ophthalmology. 2019 Nov:39(11):2517-2521. doi: 10.1007/s10792-019-01098-5. Epub 2019 Apr 9
[PubMed PMID: 30968328]
[58]
Serbecic N, Beutelspacher S, Markovic L, Roy AS, Shetty R. Repeatability and reproducibility of corneal biomechanical parameters derived from Corvis ST. European journal of ophthalmology. 2020 Nov:30(6):1287-1294. doi: 10.1177/1120672119864554. Epub 2019 Nov 20
[PubMed PMID: 31744320]
[59]
Albert DM, Keeler R. The Pressure: Before and after Schiøtz. Ophthalmology. Glaucoma. 2020 Nov-Dec:3(6):409-413. doi: 10.1016/j.ogla.2020.04.015. Epub 2020 May 5
[PubMed PMID: 32782212]
[60]
Kyari F, Nolan W, Gilbert C. Ophthalmologists' practice patterns and challenges in achieving optimal management for glaucoma in Nigeria: results from a nationwide survey. BMJ open. 2016 Oct 11:6(10):e012230. doi: 10.1136/bmjopen-2016-012230. Epub 2016 Oct 11
[PubMed PMID: 27729348]
Level 3 (low-level) evidence
[61]
Nagarajan S, Velayutham V, Ezhumalai G. Comparative evaluation of applanation and indentation tonometers in a community ophthalmology setting in Southern India. Saudi journal of ophthalmology : official journal of the Saudi Ophthalmological Society. 2016 Apr-Jun:30(2):83-7. doi: 10.1016/j.sjopt.2015.11.002. Epub 2015 Nov 19
[PubMed PMID: 27330381]
Level 2 (mid-level) evidence
[62]
Augsburger A, Terry JE. Non-contact and Mackay-Marg tonometry: comparison in patients ages 7 to 85 years. American journal of optometry and physiological optics. 1977 Jan:54(1):31-4
[PubMed PMID: 871146]
[63]
Tonnu PA, Ho T, Sharma K, White E, Bunce C, Garway-Heath D. A comparison of four methods of tonometry: method agreement and interobserver variability. The British journal of ophthalmology. 2005 Jul:89(7):847-50
[PubMed PMID: 15965164]
[64]
Kontadakis GA, Pennos A, Pentari I, Kymionis GD, Pallikaris IG, Ginis H. Accuracy of dynamic contour tonometry, Goldmann applanation tonometry, and Tono-Pen XL in edematous corneas. Therapeutic advances in ophthalmology. 2020 Jan-Dec:12():2515841420923190. doi: 10.1177/2515841420923190. Epub 2020 Jun 10
[PubMed PMID: 32577607]
Level 3 (low-level) evidence
[65]
Ferguson TJ, Knier CG, Chowdhury UR, Monson KJ, Greenwood M, Swan RJ, Gorham R, Berdahl JP, Fautsch MP. Intraocular Pressure Measurement with Pneumatonometry and a Tonometer Tip Cover. Ophthalmology and therapy. 2020 Mar:9(1):127-137. doi: 10.1007/s40123-020-00235-z. Epub 2020 Feb 20
[PubMed PMID: 32078144]
[66]
Guildford J, O'Day DM. Applanation pneumotonometry in screening for glaucoma. Southern medical journal. 1985 Sep:78(9):1081-3
[PubMed PMID: 4035436]
[67]
Esgin H, Alimgil ML, Erda S. Clinical comparison of the ocular blood flow tonograph and the Goldmann applanation tonometer. European journal of ophthalmology. 1998 Jul-Sep:8(3):162-6
[PubMed PMID: 9793770]
[68]
Gunvant P, Baskaran M, Vijaya L, Joseph IS, Watkins RJ, Nallapothula M, Broadway DC, O'Leary DJ. Effect of corneal parameters on measurements using the pulsatile ocular blood flow tonograph and Goldmann applanation tonometer. The British journal of ophthalmology. 2004 Apr:88(4):518-22
[PubMed PMID: 15031169]
[69]
Bhan A, Bhargava J, Vernon SA, Armstrong S, Bhan K, Tong L, Sung V. Repeatability of ocular blood flow pneumotonometry. Ophthalmology. 2003 Aug:110(8):1551-4
[PubMed PMID: 12917171]
[70]
Brusini P, Salvetat ML, Zeppieri M, Tosoni C, Parisi L. Comparison of ICare tonometer with Goldmann applanation tonometer in glaucoma patients. Journal of glaucoma. 2006 Jun:15(3):213-7
[PubMed PMID: 16778643]
[71]
Realini T, McMillan B, Gross RL, Devience E, Balasubramani GK. Assessing the Reliability of Intraocular Pressure Measurements Using Rebound Tonometry. Journal of glaucoma. 2021 Aug 1:30(8):629-633. doi: 10.1097/IJG.0000000000001892. Epub
[PubMed PMID: 34049350]
[72]
Rosenfeld E, Rabina G, Barequet D, Mimouni M, Fischer N, Kurtz S. Role of home monitoring with iCare ONE rebound tonometer in glaucoma patients management. International journal of ophthalmology. 2021:14(3):405-408. doi: 10.18240/ijo.2021.03.12. Epub 2021 Mar 18
[PubMed PMID: 33747817]
[73]
Cvenkel B, Velkovska MA, Jordanova VD. Self-measurement with Icare HOME tonometer, patients' feasibility and acceptability. European journal of ophthalmology. 2020 Mar:30(2):258-263. doi: 10.1177/1120672118823124. Epub 2019 Jan 11
[PubMed PMID: 30632407]
Level 2 (mid-level) evidence
[74]
Quérat L, Chen E. iCare® Home vs Goldmann applanation tonometry: Agreement of methods and comparison of inter-observer variation at a tertiary eye centre. European journal of ophthalmology. 2023 Jan:33(1):312-318. doi: 10.1177/11206721221099252. Epub 2022 May 3
[PubMed PMID: 35505614]
[75]
Nakakura S, Asaoka R, Terao E, Nagata Y, Fukuma Y, Oogi S, Shiraishi M, Kiuchi Y. Evaluation of rebound tonometer iCare IC200 as compared with IcarePRO and Goldmann applanation tonometer in patients with glaucoma. Eye and vision (London, England). 2021 Jul 1:8(1):25. doi: 10.1186/s40662-021-00249-z. Epub 2021 Jul 1
[PubMed PMID: 34193284]
[76]
Kato Y, Nakakura S, Matsuo N, Yoshitomi K, Handa M, Tabuchi H, Kiuchi Y. Agreement among Goldmann applanation tonometer, iCare, and Icare PRO rebound tonometers; non-contact tonometer; and Tonopen XL in healthy elderly subjects. International ophthalmology. 2018 Apr:38(2):687-696. doi: 10.1007/s10792-017-0518-2. Epub 2017 Apr 9
[PubMed PMID: 28393323]
[77]
Valero B, Fénolland JR, Rosenberg R, Sendon D, Mesnard C, Sigaux M, Giraud JM, Renard JP. [Reliability and reproducibility of introcular pressure (IOP) measurement with the Icare(®) Home rebound tonometer (model TA022) and comparison with Goldmann applanation tonometer in glaucoma patients]. Journal francais d'ophtalmologie. 2017 Dec:40(10):865-875. doi: 10.1016/j.jfo.2017.06.008. Epub 2017 Nov 22
[PubMed PMID: 29174296]
[78]
Liu J, De Francesco T, Schlenker M, Ahmed II. Icare Home Tonometer: A Review of Characteristics and Clinical Utility. Clinical ophthalmology (Auckland, N.Z.). 2020:14():4031-4045. doi: 10.2147/OPTH.S284844. Epub 2020 Nov 23
[PubMed PMID: 33262568]
[79]
Chen M, Zhang L, Xu J, Chen X, Gu Y, Ren Y, Wang K. Comparability of three intraocular pressure measurement: iCare pro rebound, non-contact and Goldmann applanation tonometry in different IOP group. BMC ophthalmology. 2019 Nov 14:19(1):225. doi: 10.1186/s12886-019-1236-5. Epub 2019 Nov 14
[PubMed PMID: 31726999]
[80]
Kaufmann C, Bachmann LM, Thiel MA. Intraocular pressure measurements using dynamic contour tonometry after laser in situ keratomileusis. Investigative ophthalmology & visual science. 2003 Sep:44(9):3790-4
[PubMed PMID: 12939293]
[81]
Kanngiesser HE, Kniestedt C, Robert YC. Dynamic contour tonometry: presentation of a new tonometer. Journal of glaucoma. 2005 Oct:14(5):344-50
[PubMed PMID: 16148581]
[82]
Özbilen KT, Kocabora MS. Measurement of Intraocular Pressure with Applanation, Dynamic Contour, and Air-Puff Tonometers: A Comparative Study in Primary Open-Angle Glaucoma and Healthy Cases. Beyoglu eye journal. 2020:5(3):178-187. doi: 10.14744/bej.2020.82713. Epub 2020 Dec 28
[PubMed PMID: 35098085]
Level 2 (mid-level) evidence
[83]
Katsimpris JM, Theoulakis PE, Vasilopoulos K, Skourtis G, Papadopoulos GE, Petropoulos IK. Correlation between Central Corneal Thickness and Intraocular Pressure Measured by Goldmann Applanation Tonometry or Pascal Dynamic Contour Tonometry. Klinische Monatsblatter fur Augenheilkunde. 2015 Apr:232(4):414-8. doi: 10.1055/s-0035-1545792. Epub 2015 Apr 22
[PubMed PMID: 25902089]
[84]
Lee SY, Kim EW, Choi W, Park CK, Kim S, Bae HW, Seong GJ, Kim CY. Significance of dynamic contour tonometry in evaluation of progression of glaucoma in patients with a history of laser refractive surgery. The British journal of ophthalmology. 2020 Feb:104(2):276-281. doi: 10.1136/bjophthalmol-2018-313771. Epub 2019 May 14
[PubMed PMID: 31088795]
[85]
Kandarakis A, Soumplis V, Pitsas C, Kandarakis S, Halikias J, Karagiannis D. Comparison of dynamic contour tonometry and Goldmann applanation tonometry following penetrating keratoplasty. Canadian journal of ophthalmology. Journal canadien d'ophtalmologie. 2010 Oct:45(5):489-93. doi: 10.3129/i10-035. Epub
[PubMed PMID: 20847755]
[86]
Sales-Sanz M, Arranz-Marquez E, Arruabarrena C, Teus MA. Influence of LASEK on Schiøtz, Goldmann and dynamic contour Tonometry. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2018 Jan:256(1):173-179. doi: 10.1007/s00417-017-3825-4. Epub 2017 Oct 14
[PubMed PMID: 29032414]
[87]
Bäurle S, Viestenz A, Seitz B, Viestenz A. [Intraocular pressure elevation after vitrectomy-Goldmann applanation tonometry measures lower intraocular pressure than dynamic contour tonometry]. Der Ophthalmologe : Zeitschrift der Deutschen Ophthalmologischen Gesellschaft. 2022 Jan:119(Suppl 1):71-76. doi: 10.1007/s00347-021-01443-z. Epub 2021 Jul 6
[PubMed PMID: 34228205]
[88]
Salvetat ML, Zeppieri M, Tosoni C, Brusini P. Repeatability and accuracy of applanation resonance tonometry in healthy subjects and patients with glaucoma. Acta ophthalmologica. 2014 Feb:92(1):e66-73. doi: 10.1111/aos.12209. Epub 2013 Jul 10
[PubMed PMID: 23837834]
[89]
Eklund A, Lindén C, Bäcklund T, Andersson BM, Lindahl OA. Evaluation of applanation resonator sensors for intra-ocular pressure measurement: results from clinical and in vitro studies. Medical & biological engineering & computing. 2003 Mar:41(2):190-7
[PubMed PMID: 12691439]
[90]
Jóhannesson G, Hallberg P, Eklund A, Koskela T, Lindén C. Change in intraocular pressure measurement after myopic LASEK: a study evaluating goldmann, pascal and applanation resonance tonometry. Journal of glaucoma. 2012 Apr-May:21(4):255-9. doi: 10.1097/IJG.0b013e31820719c8. Epub
[PubMed PMID: 21654513]
[91]
Mulak M, Czak WA, Mimier M, Kaczmarek R. A comparison of intraocular pressure values obtained using a Goldmann applanation tonometer and a handheld version of applanation resonance tonometer: A preliminary report. Advances in clinical and experimental medicine : official organ Wroclaw Medical University. 2018 Apr:27(4):481-485. doi: 10.17219/acem/68559. Epub
[PubMed PMID: 29558028]
Level 3 (low-level) evidence
[92]
Ottobelli L, Fogagnolo P, Frezzotti P, De Cillà S, Vallenzasca E, Digiuni M, Paderni R, Motolese I, Bagaglia SA, Motolese E, Rossetti L. Repeatability and reproducibility of applanation resonance tonometry: a cross-sectional study. BMC ophthalmology. 2015 Apr 10:15():36. doi: 10.1186/s12886-015-0028-9. Epub 2015 Apr 10
[PubMed PMID: 25885814]
Level 2 (mid-level) evidence
[93]
Liu JH, Kripke DF, Hoffman RE, Twa MD, Loving RT, Rex KM, Gupta N, Weinreb RN. Nocturnal elevation of intraocular pressure in young adults. Investigative ophthalmology & visual science. 1998 Dec:39(13):2707-12
[PubMed PMID: 9856781]
[94]
Asrani S, Zeimer R, Wilensky J, Gieser D, Vitale S, Lindenmuth K. Large diurnal fluctuations in intraocular pressure are an independent risk factor in patients with glaucoma. Journal of glaucoma. 2000 Apr:9(2):134-42
[PubMed PMID: 10782622]
[95]
Zimmermann M, Giers BC, Beck A, Bell K, Zimmermann H, Hechtner M, Hoffmann EM, Pfeiffer N, Lorenz K. Short- and long-term agreement and reproducibility of 48-hours intraocular pressure measurements in glaucoma patients. BMC ophthalmology. 2021 Jun 21:21(1):262. doi: 10.1186/s12886-021-02003-4. Epub 2021 Jun 21
[PubMed PMID: 34154547]
[96]
Esen F, Eraslan M, Cerman E, Celiker H, Kazokoglu H. Diurnal Spikes of Intraocular Pressure in Uveitic Glaucoma: A 24-hour Intraocular Pressure Monitoring Study. Seminars in ophthalmology. 2020 May 18:35(4):246-251. doi: 10.1080/08820538.2020.1809683. Epub 2020 Sep 3
[PubMed PMID: 32881589]
[97]
Mansouri K, Gillmann K. Intereye Symmetry of 24-Hour Intraocular Pressure-related Patterns in Untreated Glaucoma Patients Using a Contact Lens Sensor. Journal of glaucoma. 2020 Aug:29(8):666-670. doi: 10.1097/IJG.0000000000001563. Epub
[PubMed PMID: 32487950]
[98]
Shioya S, Higashide T, Tsuchiya S, Simon-Zoula S, Varidel T, Cerboni S, Mansouri K, Sugiyama K. Using 24-hr ocular dimensional profile recorded with a sensing contact lens to identify primary open-angle glaucoma patients with intraocular pressure constantly below the diagnostic threshold. Acta ophthalmologica. 2020 Dec:98(8):e1017-e1023. doi: 10.1111/aos.14453. Epub 2020 Apr 27
[PubMed PMID: 32339402]
[99]
Tojo N, Hayashi A. Twenty-Four-Hour Intraocular Pressure Indicators Distinguish Normal Tension Glaucoma From Healthy Eyes Measured With a Contact Lens Sensor. Journal of glaucoma. 2022 Aug 1:31(8):639-644. doi: 10.1097/IJG.0000000000002071. Epub 2022 Jun 29
[PubMed PMID: 35766388]
[100]
Tojo N, Hayashi A, Otsuka M. Correlation between 24-h continuous intraocular pressure measurement with a contact lens sensor and visual field progression. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2020 Jan:258(1):175-182. doi: 10.1007/s00417-019-04487-9. Epub 2019 Oct 28
[PubMed PMID: 31659459]
[101]
Kim YW, Kim JS, Lee SY, Ha A, Lee J, Park YJ, Kim YK, Jeoung JW, Park KH. Twenty-four-Hour Intraocular Pressure-Related Patterns from Contact Lens Sensors in Normal-Tension Glaucoma and Healthy Eyes: The Exploring Nyctohemeral Intraocular pressure related pattern for Glaucoma Management (ENIGMA) Study. Ophthalmology. 2020 Nov:127(11):1487-1497. doi: 10.1016/j.ophtha.2020.05.010. Epub 2020 May 15
[PubMed PMID: 32417391]
[102]
Mottet B, Aptel F, Romanet JP, Hubanova R, Pépin JL, Chiquet C. 24-hour intraocular pressure rhythm in young healthy subjects evaluated with continuous monitoring using a contact lens sensor. JAMA ophthalmology. 2013 Dec:131(12):1507-16. doi: 10.1001/jamaophthalmol.2013.5297. Epub
[PubMed PMID: 24158696]
[103]
Holló G, Kóthy P, Vargha P. Evaluation of continuous 24-hour intraocular pressure monitoring for assessment of prostaglandin-induced pressure reduction in glaucoma. Journal of glaucoma. 2014 Jan:23(1):e6-12. doi: 10.1097/IJG.0b013e31829e5635. Epub
[PubMed PMID: 24370812]
[104]
Lee JO, Park H, Du J, Balakrishna A, Chen O, Sretavan D, Choo H. A microscale optical implant for continuous in vivo monitoring of intraocular pressure. Microsystems & nanoengineering. 2017:3():17057. doi: 10.1038/micronano.2017.57. Epub 2017 Dec 18
[PubMed PMID: 31057882]
[105]
Dick HB, Schultz T, Gerste RD. Miniaturization in Glaucoma Monitoring and Treatment: A Review of New Technologies That Require a Minimal Surgical Approach. Ophthalmology and therapy. 2019 Mar:8(1):19-30. doi: 10.1007/s40123-019-0161-2. Epub 2019 Feb 6
[PubMed PMID: 30725339]
[106]
Mariacher S, Ebner M, Januschowski K, Hurst J, Schnichels S, Szurman P. Investigation of a novel implantable suprachoroidal pressure transducer for telemetric intraocular pressure monitoring. Experimental eye research. 2016 Oct:151():54-60. doi: 10.1016/j.exer.2016.07.016. Epub 2016 Jul 25
[PubMed PMID: 27456134]
[107]
Choritz L, Mansouri K, van den Bosch J, Weigel M, Dick HB, Wagner M, Thieme H, ARGOS study group. Telemetric Measurement of Intraocular Pressure via an Implantable Pressure Sensor-12-Month Results from the ARGOS-02 Trial. American journal of ophthalmology. 2020 Jan:209():187-196. doi: 10.1016/j.ajo.2019.09.011. Epub 2019 Sep 20
[PubMed PMID: 31545953]
[108]
Wormald R. Treatment of raised intraocular pressure and prevention of glaucoma. BMJ (Clinical research ed.). 2003 Apr 5:326(7392):723-4
[PubMed PMID: 12676823]