Continuing Education Activity
The subaxial cervical spine consists of levels C3 through C7 and includes both the bony anatomy as well as the ligamentous anatomy. Injuries to the subaxial cervical spine can be bony, soft tissue, or a combination of the two. The purpose of this activity is to review the different morphologies of subaxial cervical spine fractures as well as the different approaches to management. Special topics discussed include pediatric cervical spine trauma, cervical spine trauma in athletes, and cervical spine trauma in an ankylosed spine. This activity assists the clinical team in the evaluation, treatment, and interprofessional management of these fractures.
Objectives:
- Review the different mechanisms of action and morphologies of subaxial cervical spine fractures.
- Outline the different imaging studies and when it is appropriate to order them in the evaluation of subaxial cervical spine fractures.
- Summarize the different treatment options for the different patterns of subaxial cervical spine fractures.
- Outline the importance of improving communication between neurosurgeons or orthopedic surgeons (specialized in spine surgery), radiologists, and the rest of the interprofessional healthcare team in regards to advanced imaging to improve outcomes for patients with subaxial cervical spine fractures.
Introduction
The subaxial cervical spine consists of levels C3 through C7 and includes both the bony anatomy as well as the ligamentous anatomy. Injuries to the subaxial cervical spine can be bony, soft tissue, or a combination of the two.[1] The purpose of this activity is to review the different morphologies of subaxial cervical spine fractures as well as the different approaches to management. Special topics discussed include pediatric cervical spine trauma, cervical spine trauma in athletes, and cervical spine trauma in an ankylosed spine.
Etiology
Subaxial cervical spine fractures can be the result of high-energy mechanisms such as motor vehicle accidents and falls from heights to moderate energy mechanisms such as contact and non-contact sports. They can even occur lower energy mechanisms such as ground-level falls. The cervical spine is vulnerable to injury due to the vast amount of motion allowed in this region of the spine.[2] The different mechanisms of injury lead to both different fracture patterns as well as various ligamentous injuries.
Vertebral body fractures can take many forms. An anteroinferior teardrop fracture can result from a flexion compression mechanism.[3] This injury often occurs with the failure of the posterior tension band. An extension teardrop fracture represents an avulsion injury from an extension mechanism and inherently is stable compared to a flexion teardrop. Compression and burst fractures of the cervical spine occur with an axial load applied to the cervical spine in neutral alignment. The load is transmitted through the disc to the vertebral body, which then fails.[3]
The anterior ligaments, along with the intervertebral disc and posterior ligaments are collectively referred to as the discoligamentous complex (DLC).[2] Three column injuries of the subaxial cervical spine can be completely bony, completely discoligamentous, or a combination of the two. A distraction mechanism, often with a rotational force, can lead to facet joint subluxations with associated disruption of the disc or capsule.[2] Injuries to the posterior tension band occur due to an axial load applied to a cervical spine in slight flexion.[3] Injuries to the anterior ligaments can occur with a distraction and extension moment. The superior vertebral body may translate posteriorly in light of this injury and can cause a spinal cord injury.[3]
Epidemiology
Cervical spine injuries occur in 3% of blunt force trauma patients with the subaxial cervical spine being a common location within the cervical spine; 50% of injuries occur between C5 and C7.[2] These can be seen in young patients with high energy mechanisms of injury or older patients with low energy mechanisms of injury. Very low energy mechanisms can present in the patient population with ankylosis spondylitis (AS), and there should be a high suspicion of cervical spine fracture in these patients with even minimal trauma.[4] The risk of a patient with AS sustaining a vertebral fracture throughout their life is four times greater than a patient without the condition. Over 75% of these fractures will occur in the cervical spine.[4] This proclivity is due to the rigidity of the spine due to long-segment fusion.
Cervical spine injuries due to athletic activity most commonly occur in athletes under the age of 30.[3] Activities vary by geographic area; in the United States American football, wrestling and gymnastics are the most common sports leading to cervical spine injuries. In Europe, the most common sport that leads to these injuries is rugby, in Canada, it is ice hockey.[3] There should be an increased concern for a cervical spine injury in an athlete who presents with a focal neurologic deficit, has neck pain, torticollis, or reports diving as the mechanism of injury.[5]
History and Physical
A thorough clinical and radiographic evaluation is an absolute requirement when assessing a possible cervical spine injury.[2] After performing advanced trauma life support (ATLS), the cervical spine should be stabilized, and the posterior aspect of the neck palpated for both midline tenderness and any step-off.[2] The entire spine should undergo evaluation if a cervical spine injury is suspected; this includes a log roll with the maintenance of cervical spine stability.[2] About 10 to 15% of patients with cervical spine fractures get diagnosed with noncontiguous spine injuries.[6]
The maintenance of cervical spine stability varies with the age of the patient. As a young child grows, head circumference enlarges faster than the chest circumference. When placed on an unmodified spine board, their necks get forced into flexion due to the disproportionate size of their heads.[7] Alignment of the external auditory meatus with the shoulders, even if this involves a relative extension of the neck, will align the cervical spine in neutral and avoid forward flexion in young children.[7] During immobilization, the clinician must consider modifications with a roll under the shoulders or a cut out in the spine board for the posterior head to facilitate extension with children.
A methodical sensory and motor exam, including reflexes of the upper and lower extremities, should be performed to identify any neurological deficits or any upper motor neuron signs that may indicate cord compression. Any deficit may also be used to help localize the level of injury in the cervical spine. It is important to remember that in the cervical spine, the numbered nerve root will exit above the associate vertebral body, i.e., the C5 nerve root exits through the foramen between C4 and C5.
A detailed history can help define the mechanism of action of the injury as well as identify any pre-existing conditions that may lead to a higher susceptibility of cervical injury, such as AS or spinal fusion either congenital or surgical.[2] The importance of this portion of the patient’s evaluation should not be ignored.
In the setting of an athletic injury with a cervical spine injury suspected, the player needs to be evaluated and handled carefully. A full neurologic exam is a must. The cervical spine should be immobilized, and the player placed on a spine board.[3] Once stabilized, transportation to a hospital for further evaluation can proceed.
Evaluation
Alignment in a normal cervical spine should be 15 to 30 degrees of lordosis from C1 through C7.[1] This is assessable with radiographic studies. When performing a radiographic evaluation, three views of the cervical spine, including an anteroposterior, lateral, and open-mouth odontoid are the standard. It is important to verify that the films are adequate, meaning there is a visualization of the occipitocervical and cervicothoracic junctions. This series will allow for evaluation of the overall alignment of the cervical spine, changes in disc height, and asymmetry in the interspinous distance.[2] While assessing lateral imaging, posterior widening between the spinous processes can indicate a posterior ligamentous injury.[1]
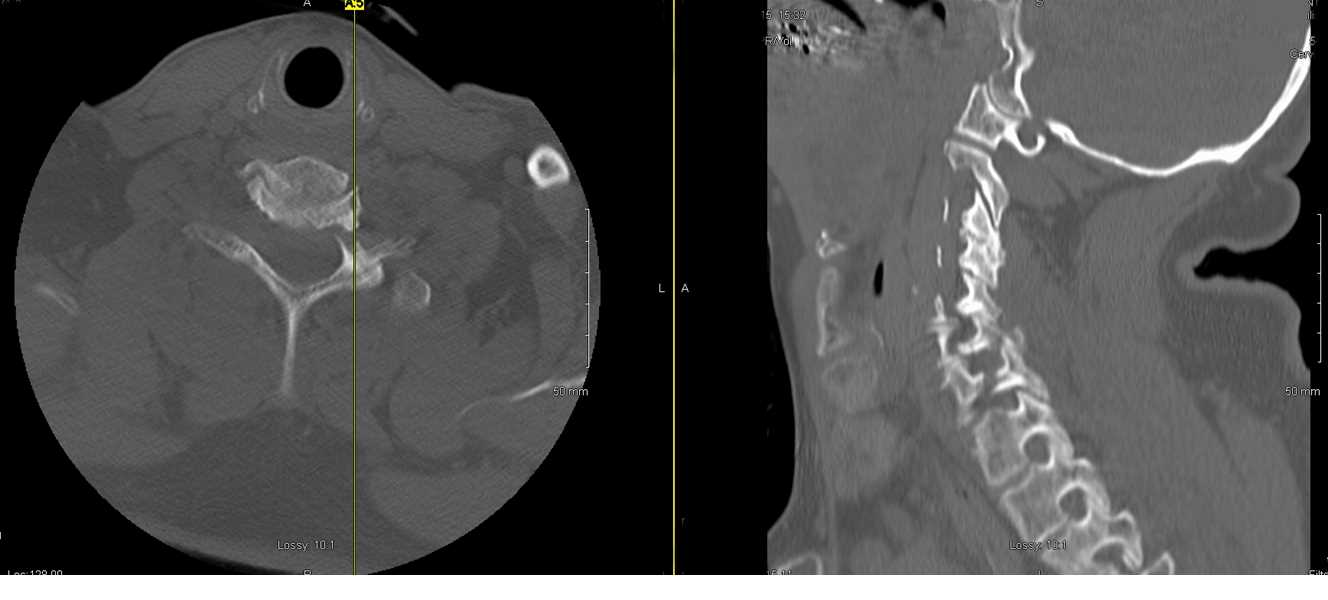
While radiographs of the cervical spine were the standard for trauma patients and patients with suspected cervical spine injuries in the past, the popularity of computed tomogram (CT) scans has led to a change in practice. With its speed, high sensitivity and specificity, and availability, multiplanar CT scans are quickly becoming standard in patients with cervical spine injuries.[2] CT scans are particularly adept at demonstrating malalignment of facet fracture-dislocations. The axial cuts allow for evaluation of the facets and lamina for fractures to help categorize dislocations as osseous-ligamentous or purely ligamentous.[6]
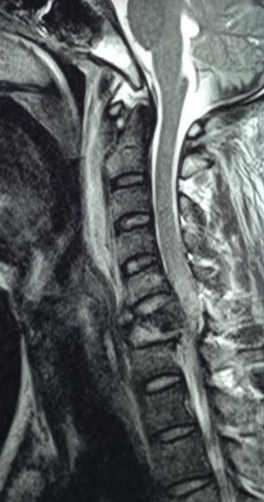
With high suspicion of an associated neural injury, ordering cervical spine magnetic resonance imaging (MRI) is becoming more commonplace as well. MRI is superior to CT scans for evaluating the spinal cord, nerve roots, disc, and ligamentous structures in the cervical spine.[8] MRI studies allow for visualization of the soft tissues surrounding the cervical spine, including the posterior ligamentous complex and the discs, in addition to any hematomas that may have collected.[2]
Due to rising healthcare costs, there has been an effort to determine which patients need advanced imaging with an MRI and which do not. Risk factors of an MRI disclosing a treatment-altering injury missed on the CT scan include age over 60, polytrauma patients, cervical spondylosis, a neurologic deficit, and a patient that cannot undergo evaluation due to a low GCS or other altered mental status.[8] A patient who is awake, alert, cooperative, exhibiting no neurologic deficit on examination, asymptomatic, and without distracting injuries do not need an MRI.[8] If the patient falls between these two broad categories of patients, it is the physician's judgment on whether obtaining an MRI would help you decide how to treat the injuries. [8]
When evaluating the radiographic studies, the different fracture morphologies have different characteristics. Vertebral body compression fractures have visible height loss of the vertebral body with anterior wedging and a maintained posterior cortex. Burst fractures are also in the category of compression fractures.[2] Burst fractures involve the anterior and posterior cortices of the vertebral body and are frequently associated with neurology injury.[1] With any vertebral body compression or burst fracture, be sure to assess for posterior widening of the spinous processes that is greater than the other vertebra. This indicates a posterior ligamentous injury that will lead to continued instability of the segment if not stabilized.[1] This subtle finding can have serious clinical repercussions if missed. Lateral mass and facet fractures that are unilateral and minimally displaced fall into the compression fracture category as well as they are often due to a compressive mechanism.[2]
Facet dislocations and fractures can be unilateral or bilateral. A subluxation of the facet can also occur; referred to as a perched facet. Distraction mechanisms, often with a rotational force, can lead to facet joint subluxations with associated disruption of the disc or capsule.[2] These are visible as asymmetry in the shingling of the facets on the lateral radiographs or the sagittal cuts of the CT scan. Once again, the axial views provided on the CT scan allow for assessment of the facet joint articulation as well as providing information about posterior bony fractures that are difficult to diagnose on X-rays alone.
Special consideration in the evaluation of a patient with AS is that it can be challenging to identify fractures on plain films due to the fusion mass. The clinician should treat those presenting with acute neck pain or a change in postural position as though they have a fracture until proven otherwise.[4] Advanced imaging of the entire spine, be it CT or MRI, is recommended when a fracture is suspected.[4]
Upon completing the history, physical exam, and imaging studies, the clinician must determine what the treatment plan for the patient will be. There are a couple of classification systems that have been devised to help guide the physician in this decision. The first is the Subaxial Injury Classification System (SLIC). This classification stratifies the type of fracture, the competency of the DLC, and the patient’s neurologic status with numerical values to determine the course of treatment. A score of three or less suggests conservative management; a score of five or more indicates operative management, whereas a score of four is a gray zone and left to physician judgment.[2] A second classification system is the AOSpine Subaxial Cervical Spine Injury Classification. This system was devised in an attempt to create a validated injury classification and settle controversies that came from the SLIC system. This classification system has four categories to grade: fracture type, facet injury, neurological status, and the presence of specific modifiers.[2] The hope in developing this system was that it would provide a more precise definition of facet joint integrity and DLC competency, but this remains unestablished in validation studies.
Treatment / Management
Initially, all patients with subaxial cervical spine fractures require immobilization in a rigid cervical orthosis.[2] Patients receiving conservative treatment are often prescribed a rigid cervical or cervicothoracic orthosis for 6 to 12 weeks with regular follow-up and interval radiographs to assess alignment.[2]
Patients with fractures deemed unstable or neurologic compromise should undergo decompression and stabilization. Intervention within 24 hours of injury leads to better improvement in ASIA scores.[2] Whether the surgeon approaches the fracture from an anterior or a posterior approach will be determined by the pattern of the pathology.[2]
True compression fractures with no posterior ligamentous or capsular involvement can be treated nonoperatively in a hard cervical orthosis. If there is posterior ligamentous or capsular involvement, surgery for stabilization is indicated.[1] Even in the athletic population, when these fracture patterns occur without neurologic compromise and DLC involvement, they can be managed in a hard cervical orthosis.[3] One caveat is that there is a high rate of progressive kyphosis if the fracture is a C7. These need to be followed closely with radiographs and may warrant surgical correction if the deformity is progressing.[3]
Burst fractures with retropulsion in the canal are different than a true compression fracture. Inline cervical traction can often reduce burst fractures and decrease bony retropulsion in the canal. These fractures are often unstable and often associated with neurologic symptoms, and most of the time, require surgical fixation.[1] Burst fractures with retropulsion and flexion-type teardrop fractures often get treated with an anterior corpectomy, bone grafting, and plating. This procedure may require a posterior approach depending on the number of levels involved and the integrity of the DLC.[2]
A timely closed reduction of facet dislocations with cervical traction is appropriate in an awake and alert patient who can undergo serial neurologic exams during the reduction.[2] Unilateral facet dislocations may be locked and difficult to successfully perform a closed reduction with traction alone.[1] While a closed reduction with traction of bilateral facet dislocations is usually easier to reduce, they are often very unstable and require surgical fixation to maintain reduction.[1] Closed reduction with cervical tong traction begins with 10 to 15 pounds (2 - 4.5 kg). The recommendation is then to add 5 to 10 pounds (2 - 4.5 kg) for each level of injury, for example for a dislocation at C5, an initial 10 to 15 pounds is placed, and then an additional 25 to 50 pounds (2 - 4.5 kg) is added incrementally, done with serial neurologic exams.[6] If a patient is obtunded or not able to cooperate with serial neurologic exams, an MRI is necessary before attempts at closed reduction and operative fixation.[6] An anterior discectomy can be utilized to help remove a herniated cervical disc but also the gain reduction of a dislocated facet. Once reduced, the surgeon can perform a fusion. Again, based on the injury extent, this may need to be combined with a posterior approach.[2]
When caring for a patient with AS, upon initial evaluation, they may not have a neurologic deficit. However, they require monitoring. Seemingly small fractures can lead to progressive neurologic deterioration in these patients.[4] These seemingly small fractures are unstable due to the long lever arm of the fused spine and often require surgical stabilization with longer constructs and possibly evacuation of epidural hematomas.[4] These fractures can be approached anteriorly, posteriorly, or in a combined anterior-posterior approach, which is mostly a function of the fracture pattern as well as patient factors, such as a chin on chest deformity that interferes with an anterior approach.[4]
Differential Diagnosis
Subaxial cervical spine fractures include several different morphologies, including compression fractures, burst fractures, distraction injuries, or translational injuries.[2] There can also be a ligamentous injury.
Prognosis
Patients with increased time from injury to surgery, more severe injury as graded on the Subaxial Cervical Spine Injury Classification, and larger maximal spinal cord compression exhibit a poorer prognosis.[9] The more time the cord is compressed, the less chance for neurologic recovery.[9] Of patients that present with a neurologic deficit and receive surgical treatment, 60% had no progression of their deficit, and about 30% had improvement of their deficit at follow-up.[4] Surgical treatment leads to a decreased overall complication rate as compared to nonoperative management at both short and long-term follow-up.[4]
There is a higher incidence of major neurologic complications in patients with AS, such as paresis, following a cervical spine fracture as compared to a patient without the diagnosis.[4]
Complications
Inadequate plain films and lack of advanced imaging can lead to a missed cervical spine injury.[10] Missed subaxial cervical spine injuries can lead to neurologic deterioration and spinal cord injuries.[2] If the entire spine does not undergo adequate assessment, there can be missed injuries elsewhere in the spine.
Injury to the vertebral artery may occur as a result of subaxial cervical spine trauma or intraoperatively.[6]
Secondary neurologic deterioration is a potential complication of cervical spine injuries - this manifests as a progressive motor or sensory loss at or above the level of the injury after the initial assessment. Risk factors for this deterioration include a flexion mechanism of injury and an underlying ankylosed spine.[10] Ankylosing spondylitis can also lead to a delay in the diagnosis of subaxial cervical spine fracture if advanced imaging does not occur promptly.[4]
Surgical treatment of these fractures can lead to the known complications of spine surgery, including infection, dural tears, neurologic injury, pseudarthrosis, and hardware loosening.[6]
Deterrence and Patient Education
In patients treated conservatively, the importance of adherence to the prescribed orthosis must be a topic of discussion. Proper discharge instructions, as well as follow-up appointments, must be arranged with the patient.
In patients that are undergoing surgical stabilization, adequate informed consent with an explanation of all the potential risks and benefits of the procedure and alternatives must take place.
Enhancing Healthcare Team Outcomes
Due to the high level of potential neurologic compromise, randomized controlled trials of treatment strategies with subaxial cervical spine fractures are not feasible. Continued research in the validity of a subaxial cervical spine fracture classification system can lead to a more standardized approach and even a better idea of patient prognosis.
Depending on the level of injury and the extent of spinal cord compression, these patients need a great deal of communication between multiple specialists, including the neurosurgeon or orthopedic surgeon (specialized in spine surgery), neuroradiologist, neuro-anesthetist, intensivist, neuro nurse, and physiatrist. Early intervention with rehabilitation and mobilization once the spine has undergone stabilization is important.
These injuries require open communication and collaboration among all members of the healthcare team; this could even include chiropractors, since they may be the first to encounter these patients and take in-office radiographs, and need to understand when manipulation is inappropriate. After surgery, physical therapists may play a role in the rehabilitation process. Specialty-trained neurological or orthopedic nurses will assist in management before, during, and following any procedure, whether it is a closed reduction or surgical. All these disciplines must work together with open communication to bring about the best result with minimal disability for the patient. [Level 5]