Continuing Education Activity
Peripheral nerve neuralgia or peripheral neuropathic pain may result from damage of a nerve due to various etiologies including medical conditions such as diabetes, infections (e.g., postherpetic neuralgia), kidney diseases, or nerve compressions such as entrapment, as well as peripheral nerve injury due to trauma, cancer, or a combination of the above. Although treatment strategies for neuralgia usually start with pharmacotherapy, drug treatment often fails to obtain effective results and can expose the patient to side effects with poor improvement in the quality of life. It is often necessary to resort to non-pharmacological strategies such as neurolytic blocks. Peripheral neurolytic blocks are indicated to alleviate severe intractable pain. This activity reviews severe intractable pain and highlights the role of the interprofessional team in managing this condition.
Objectives:
- Describe the indications for peripheral neurolytic block procedures.
- Summarize the mechanism behind the efficacy of a peripheral neurolytic block procedure.
- Identify the potential complications of peripheral neurolytic blocks.
- Explain the significance of collaboration and communication among the interprofessional team to enhance the efficacy of peripheral neurolytic blocks and to improve patient outcomes.
Introduction
Peripheral nerve neuralgia or peripheral neuropathic pain may result from damage of a nerve due to various etiologies including medical conditions such as diabetes, infections (e.g., postherpetic neuralgia), kidney diseases, or nerve compressions such as entrapment, as well as peripheral nerve injury due to trauma, cancer, or a combination of the above. Although treatment strategies for neuralgia usually start with pharmacotherapy with antineuropathic drugs such as membrane-stabilizing agents (e.g., gabapentin or pregabalin), anticonvulsants (e.g., carbamazepine, topiramate, and lamotrigine), antidepressants (e.g., amitriptyline), and muscle relaxants (e.g., baclofen) to reduce the excitability of the peripheral nerve and central connections,[1] drug treatment often fails to obtain effective results and can expose the patient to side effects with poor improvement in the quality of life (QoL). Therefore, it is often necessary to resort to non-pharmacological strategies such as neurolytic blocks. These approaches, however, are not only applicable when pharmacological strategies have failed but are to be integrated into the context of multimodal schemes.[2] Moreover, some types of painful conditions, such as pain from pancreatic neoplasia, must necessarily be managed through the use of minimally invasive analgesic techniques, already at the onset of symptoms.[3]
A neurolytic block is a form of block involving the deliberate injury of a nerve by freezing or heating or the application of chemicals to cause a temporary degeneration of targeted nerve fibers, causing an interruption in the signal nerve transmission. In particular, neurolysis implies the destruction of neurons by placing a needle close to the nerve and either injecting neurodestructive chemicals agent or producing damage with a physical method such as cold (i.e., cryotherapy) or heat (i.e., radiofrequency ablation, RFA).
In exemplary terms, neurolytic blocks would represent the natural evolution of neurotomy that is another approach for the treatment of neuropathies. It represents a transaction or partial resection of a nerve performed on small peripheral nerves that are exclusively sensory. It has long been used to treat trigeminal neuropathy, pelvic pain syndrome (presacral neurotomy), and other painful and no-painful conditions (e.g., spastic dysfunction of the elbow). Because the surgical cutting of a nerve can induce over time a painful neuroma or differentiation, neurolytic approaches are usually preferred over the surgical blocks.
Neurolytic blocks, however, are not a recent discovery. The first report of chemical neurolysis for the treatment of pain was made, in 1863, by Luton who administered neurolytic agents into painful areas. Neural blockade with neurolytic agents has been documented for the treatment of pain for over a century. In 1904, Schloesser was the first to report alcohol neurolysis for the treatment of trigeminal neuralgia.[4] Later on, in 1928, Doppler used phenol neurolysis to destroy presacral sympathetic nerves for the treatment of pelvic pain.
Nowadays, the specialty of pain medicine defines neurolysis as the selective, iatrogenic destruction of neural tissue to secure the relief of pain. Over time, indeed, knowledge of nervous pathophysiology, refinement of the techniques and tools available, have increasingly flooded the indications of these techniques. Advances in medical imaging, for instance, have allowed precision and, therefore, better efficiency in the practice of interventional pain management. The previous pain treatment algorithms have been progressively modified to include peripheral neural blockade and neuro-destructive techniques.[5] Again, peripheral nerve blockade represents one of the therapeutic possibilities to treat the spasticity of various muscles.[6]
Anatomy and Physiology
Because chemical and surgical neurolysis potentially have very serious side effects, a thorough knowledge of the relevant anatomy and mechanism by which the agent destroys nerve tissue is essential. Anatomy depends on the sensory territory to block. Neurolytic block can, therefore, theoretically be applied anywhere along the sensory pathway. As a consequence, peripheral nerves, sympathetic ganglia, and dorsal roots are all examples of potential targets for neurolysis. The procedure can be practiced by guidance through ultrasonography, fluoroscopy, and/or nerve stimulation. It is important to first perform a prognostic block with a local anesthetic in order to assess efficacy. Important preconditions for the application of peripheral neurolytic block include good knowledge of anatomy, attention to and control of side effects, as well as the choice of the correct block techniques.[7]
Indications
Proper selection of patients for neurolytic blocks is the key to the success of these potentially harmful procedures. Clear communication of alternative techniques, outcomes, complications, expectations, and disease progression with the patient and the family is important prior to a neurolytic procedure. An interprofessional approach, including an aggressive trial of opioids and adjuvant medications, along with temporary nerve blocks and psychological support, are the mainstays of therapy. A thorough medical examination, including laboratory testing and imaging studies, if appropriate, is necessary before performing this procedure.
Neurolytic blocks are also useful in the differential diagnosis of the site and cause of the pain, and in determining the patient's reaction if the pain is eliminated. Properly applied, certain nerve blocks are used to predict the effects of prolonged interruption by injection of neurolytic agents or by the neurosurgical section.
Upper Abdominal Malignancies or Chronic Pancreatitis: Patients with intractable abdominal pain due to upper abdominal malignancies or chronic pancreatitis have chronic refractory pain significantly decreases the quality of life and often requires high doses of opioids, which can lead to serious adverse side effects.[8] In these patients, the percutaneous neurolytic celiac plexus block (NCPB) has been shown to decrease narcotic usage in 70% to 90% of patients.[9] Furthermore, a meta-analysis on the efficacy and safety of NCPB for cancer pain, including 24 papers, was performed.[10] In this evidence-based study, encompassing twenty-one retrospective studies, one prospective, and two randomized and controlled investigations, cancer type was stated in 1117 of 1145 patients reported (63% pancreatic, 37% nonpancreatic). Good to excellent pain relief was reported in 878/989 patients (89%) during the first 2 weeks after NCPB. Long-term follow-up beyond 3 months revealed persistent benefit.
Trigeminal Neuralgia (TN): It is one of the most common forms of craniofacial pain.[11] TN is characterized by sudden, brief, and excruciating facial pain attacks in one or more of the branches, leading to a severe reduction in the QoL of affected patients. Internal neurolysis is an effective surgical treatment for TN without neurovascular compression.[12]
Chest Wall Pain or Postsurgical Thoracic Pain: Intractable cancer-associated chest wall pain or for postsurgical thoracic pain, intercostal nerve block by chemical neurolysis with phenol may be a promising therapeutic option in patients with chronic neuropathic pain.[13]
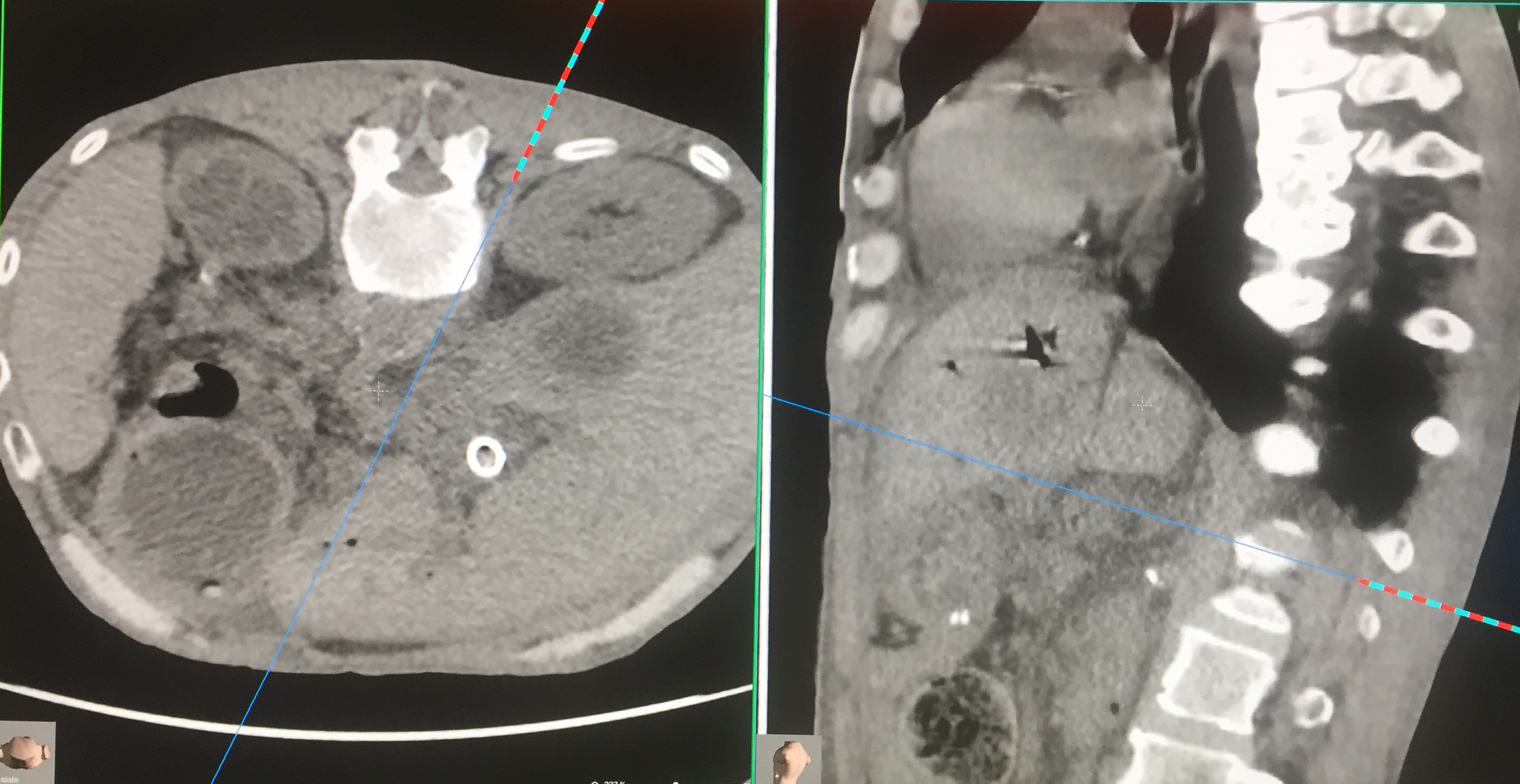
Pelvic Cancer Pain: Pain associated with pelvic malignancies can be treated by superior hypogastric plexus blockade or neurolysis.[14] This block is difficult to perform and hampered by bony structures of the iliac crest and the transverse process of L5. Fluoroscopically guided posterolateral transdiscal technique may be a valuable alternative, the patient reported a reduction of pain in the lower abdomen, and the QoL was significantly improved.[15][16]
Other Indications: Ultrasound-guided alcohol ablation has been described to treat Morton neuroma, and several studies have been performed describing the safety and efficacy of alcohol ablation in these cases.[17] Additionally, alcohol neurolysis of the lateral femoral cutaneous nerve (LFCN) has been described to treat meralgia paresthetica.[18]
Contraindications
Absolute contraindications to a peripheral nerve blockade are rare. They can include:
- Patient refusal
- Skin infection over the intended catheter or needle site
- Allergy to a chemical neurolytic agent
- Uncorrectable coagulopathy
In particular, uncorrectable coagulopathy must be emphasized. Oral anticoagulant needs to be held until the international normalized ratio(INR) is 1.5 or less because a bleeding disorder is considered as a contraindication, particularly if injection occurs at a non-compressible site. If radiofrequency ablation is planned, a patient with a pacemaker must be checked.
Equipment
Methods used to make neurolysis include surgical transection, cryoneurotomy, thermal radiofrequency, neuroselective toxins, nonselective chemical ablation, and laser neurolysis. None of these techniques completely destroy the nerve.
Nonselective neurolytic chemical agents including phenol, ethyl alcohol, and glycerol 50%. Other compounds such as hypertonic saline (e.g., 10% NaCl), ammonium salts (e.g., ammonium sulfate 10%), and chlorocresol are less used. Neuroselective toxins include capsaicin and botulinum toxin.
The perineural administration of ethyl alcohol or phenol results in protein denaturation and neurolysis (Wallerian degeneration). This can produce long-lasting analgesia, with a duration of 3-6 months.[19] Phenol and ethyl alcohol mediate their effect through nonselective denaturing of proteins upon exposure to the nerve leading to loss of cellular fatty content, separation of the myelin sheath from the axon, and axonal edema, thereby causing nerve injury by precipitating and dehydrating the protoplasm.
Capsaicin is a highly selective agonist for TRPV1 (vanilloid receptor 1) on unmyelinated C fiber nociceptors, provoking an influx of calcium and sodium ions and, in turn, depolarization of the nociceptive afferent terminals.[20] The prolonged exposure of neurons to this agent results in a nerve terminal's desensitization.
Botulinum neurotoxins (BoNT) possess an analgesic effect through several mechanisms. Animal studies have shown that peripheral injection of BoNTs impairs the release of major pain transmitters such as substance P, calcitonin gene-related peptide (CGRP), and glutamate from peripheral nerve endings as well as peripheral and central neurons (dorsal root ganglia and spinal cord).[21] It is neurotoxic to cholinergic nerves by blocking acetylcholine release.
Peripheral cryoneurotomy (or cryotherapy) is performed through nitrogen or argon gas to create extremely cold temperatures to destroy diseased tissue. Studies showed that it resulted in good pain control for several years in patients with intractable neuralgia.[22][23] Nevertheless, cryoneurotomy does not directly damage the structural integrity of the nerve, whereas neurectomy amputates part of it. On the other hand, peripheral surgical neurectomy results in a short-term benefit only and is often followed by severe dysaesthetic pain.[24] One of the key differences between transection and cryoinjury is the extent of the injury. Transection results in full-thickness disruption of the peripheral nerve, whereas with cryoinjury, the structural integrity of the nerve is maintained.[25] In an experimental study, D'Rozario et al. demonstrated the histological effects of surgical transection and cryoneurotomy on the trigeminal ganglion in rats over time. Peripheral cryoneurotomy resulted in degenerative changes in the trigeminal ganglion that rapidly recovered while the transaction of the mental nerve showed irreversible changes. This investigation can help to explain why peripheral cryoneurotomy produces good pain control without nerve damage and also why the symptoms eventually recur.[26]
Radiofrequency denervation or ablation (RFA) or radiofrequency neurotomy, is a procedure commonly adopted in several non-painful conditions (e.g., cardiac arrhythmias, tumors, aesthetics dermatology, varicose veins) and for addressing pain. Through a medium frequency alternating current generated by a radio, a small area of nerve tissue is heat-treated, decreasing pain conduction from that specific area. The effectiveness of the technique depends on the application site. In general terms, it is possible to obtain a good result in over two-thirds of the patients. Concerning the duration of the effects, pain relief can last up to 12 months, but it can last for years. The indications for the technique are manifold. For example, this is approach is also used for treating migraines (sphenopalatine ganglion RFA).[27]
Pulsed radiofrequency, which was first proposed by Sluijter ME as a treatment of neuropathic pain (NP), is a non-destructive, minimally invasive technique applied to the nervous system and has been widely administered clinically in many pain treatment centers.[28] The method is used in the treatment of chronic pain to destroy small nerves conducting nociceptive stimuli, for tumor ablation, and in cardiology to ablate abnormal atrioventricular connections. During the procedure, the current is delivered in short pulses. The recommended parameters are a pulse width of 20 msec and a rate of 2 Hz, and it has recently become an increasingly popular technique for the clinical treatment of neuropathic pain.[29]
Weintraub (1997) reported on the results of laser neurolysis in a series of 30 hands of 23 patients with carpal tunnel syndrome. The laser was delivered at a power of 9 Joules per point at 5 points along the median nerve. The investigators reported that 77% of cases achieved complete resolution of symptoms.
During all procedures, hemodynamic monitoring remains mandatory, and the care unit specializing in neurolysis must have the following equipment:
Drugs
- Chlorhexidine gluconate
- Local anesthetic, typically 2% lidocaine
- Regional block local anesthetic test solution (2% lidocaine)
- Chemical neurolytic agent (phenol, ethyl alcohol, and glycerol, capsaicin, and botulinum toxin)
- A 10 mL to 20 mL syringe with extension tubing
Device
- Block needle (length-variable depending on the region to be treated)
- Fluoroscopy equipment
- Nerve stimulator
- Ultrasound probe
- Radiofrequency probe
- Cryo machine and cryoprobe with cooling agents (i.e., nitrous oxide, carbon dioxide)
- Basic monitoring such as (electrocardiogram (ECG), blood pressure cuff, pulse oximetry, end-tidal carbon dioxide (ETCO2) for the entire procedure for observing symptoms due to inadvertent intravascular injection or other clinical conditions.
Personnel
The neurolytic block must be practiced in care units specialized in the interventional treatment of pain, equipped with a pain medicine specialist with training in ultrasound and fluoroscopic-guided nerve injections.
Preparation
Patient preparation must be carried out considering that the procedure, although well-tolerated and safe in most cases, can still lead to serious complications:
- Informed Consent: Before conducting the intervention, informed consent is mandatory for getting permission. It must contain details of the procedure and possible complications (possibly with frequency).
- An intravenous line may be placed.
- Aseptic technique should be maintained throughout the procedure.
- Positioning: The patient's position depends on the procedure to be performed.
- Sedation: Although sedation by hypnotics may be necessary for certain painful acts such as chemical neurolysis, excessive sedation of the patient should be avoided to allow patients to remain alert enough to report symptoms suggestive of any complication.[30]
Technique or Treatment
Social, emotional, financial, and legal factors compound the complexity of chronic pain. To clarify these challenging clinical situations, diagnostic blocks are used to determine the site of nociception and the pathway of afferent neural signals. As a general scheme, neurolysis procedures can be divided into three phases:
- Under aseptic precaution and cardiovascular monitoring, the desired target nerve is first identified via ultrasound, nerve stimulation, or fluoroscopy, and a local anesthetic is infiltrated at the skin.
- Subsequently, the needle for a radiofrequency probe or cryoprobe is advanced toward the target nerve, and a diagnostic block with a local anesthetic may be performed.
- After confirmation of block efficacy, the neurolysis procedure is performed. In the case of RFA, a microelectrode is inserted through the needle to begin the neurolysis. If the procedure provides the use of chemical agents, the prepared chemical solution like phenol may then be injected. Because phenol has immediate local anesthetic effects, injection is typically painless. Cardiovascular monitoring during and after the procedure with resuscitative backup is important in preventing and treating adverse outcomes.
Complications
Risks associated with any injection include:
- Infection at the site of the injection
- Increased inflammation and pain at the site of the injection
- Bleeding and/or bruising
- Injury to blood vessels or nerves
- Allergic reaction to the local anesthetic or other medications used during the procedure.
An accidental intravascular injection of phenol may cause tinnitus and flushing. Partial nerve destruction may cause neuritis of a somatic nerve with subsequent regeneration and dysesthesia or hyperesthesia (procedure failure).[31]
Systemic side effects (e.g., due intravascular injection of a local anesthetic) include nausea and vomiting, leg numbness which usually lasts a few hours, as well as serious side effects such as central nervous system (CNS) stimulation with seizures, and cardiovascular and/or CNS depression until cardiac arrest and coma.
Clinical Significance
Neurolysis is an alternative to allow patients the ability to control their pain with less systemic medication, significantly improving their QoL. Peripheral neurolytic blocks are advocated to treat severe malignant intractable pain caused primarily by advanced terminal cancer. Rarely, some forms of nonmalignant pain can be treated with neurolysis (for example, intractable postherpetic neuralgia and chronic pancreatitis). Nevertheless, the role of these non-pharmacological approaches for the management of chronic, nonmalignant painful conditions is debated and often discouraged.
In the literature currently, there are large-scale controlled studies on the use and beneficial effects of the peripheral neurolytic block in the treatment of malignant and nonmalignant pain. These investigations include randomized controlled trials (RCTs), observational trials, and many case series.
To evaluate the efficacy of cryoneurolysis for reduction of pain associated with knee osteoarthritis (OA), a randomized, double-blind, sham-controlled, multicenter trial with a 6-month follow-up in patients demonstrated that patients randomized to cryoneurolysis targeting the infrapatellar branch of the saphenous nerve (IPBSN) had a statistically significant greater change from baseline in the WOMAC (Western Ontario and McMaster Osteoarthritis Index) pain subscale score at day 30, day 60, and day 90 after cryoneurolysis.[32] The authors concluded that the cryoneurolysis of the IPBSN resulted in statistically significant decreased knee pain and improved symptoms compared to sham treatment for up to 150 days, and appeared safe and well-tolerated. Of note, permanent blockade with cryoneurolysis does not usually occur because the cryoinjured axons regenerate, the median duration of pain relief is 2 weeks to 5 months; thus, it is considered best suited for clinical situations when analgesia is required for weeks or months.[33] Also, for pain that originates from small, well-localized lesions of peripheral nerves (e.g., neuroma, entrapment neuropathies, and postoperative pain).
RFA for the lumbar medial branch has been most studied. It is an emerging treatment option for chronic low back pain (LBP). In a recent study, the authors investigated long-term treatment outcomes of patients selected (n=85) for zygapophyseal joint (z-joint)-mediated LBP.[34] At a minimum of six months, 70.6% of patients reported a pain reduction. The authors concluded that RFA is an effective, durable treatment for a significant proportion of patients with recalcitrant lumbar z-joint pain. A systematic review was conducted retrieving 1063 papers.[35] Eleven sham-controlled RCTs were included: three studies involving discogenic back pain, six studies involving lumbar facet joint pain, and two studies involving sacroiliac joint pain. The evidence supports RFA as an efficacious treatment for lumbar facet joint and sacroiliac joint pain, with five of six and both of the RCTs demonstrating statistically significant pain reductions, respectively.
As to the long-term effectiveness of the RFA for chronic LBP, controversies exist, for example, in RCTs including 681 participants with chronic LBP originating from the facet joints, sacroiliac joints, or a combination of these or the intervertebral disks, radiofrequency denervation combined with exercise compared with exercise alone resulted in either no significant difference in pain intensity after 3 months.[36] Nevertheless, radiofrequency denervation is commonly used for the treatment of chronic facet joint pain that has been refractory to more conservative treatments. In a recent meta-analysis including data from seven trials involving 454 patients who had undergone radiofrequency denervation (n=231) and control treatments such as sham or epidural block procedures (n=223), the authors found that a subgroup of patients who responded very well to diagnostic block procedures demonstrated significant improvements in back pain relative to the control group at all times.[37] However, the matter is subject to debate. Maas et al., for instance, conducted a Cochrane analysis including 23 RCTs (n=1309) of RFA for patients with chronic LBP who had a positive response to a diagnostic block or discography. Of note, the authors found no high-quality evidence suggesting that RF denervation provides pain relief for patients with LBP.[38]
Endoscopic ultrasound-guided neurolytic celiac plexus block (NCPB) should be considered as the adjunct method to standard pain management because it may reduce pain in pancreatic cancer. In a systematic review, 27 RCTs were considered.[39] Regardless of the technique used, NCPB improved analgesia and/or decrease opioid consumption, and decreased opioid-induced adverse effects in comparison with conventional analgesic treatment. Nevertheless, the authors concluded that there is high-quality evidence of the analgesic efficacy of NCPB in patients with pancreatic cancer pain. The level of evidence on the reduction of opioid consumption and opioid side effects is not as good. At present, the majority of current data supports the use of NCPB, and in comparison to standard pharmacotherapy, it has been shown to be more effective in reducing pain and leads to decreased opioid requirements and their related side effects, and in turn, preventing deterioration in the QoL in such patients
Of all peripheral nerve neurectomies, ilioinguinal and iliohypogastric neurectomy have been most extensively studied. Inguinal neurectomy at the time of hernia repair may reduce the risk of postoperative pain. In a meta-analysis, 11 studies on 1031 patients included performed Lichtenstein hernia repair and showed a significant reduction in pain with neurectomy for short and midterm.[40]
Interventional techniques to manage pain may be efficient treatment modalities in patients unable to tolerate systemic opioids or patients who have limited life expectancy with localized pain. Outcomes data for pain relief remains inconsistent due to variable patient prognosis, so the selection of appropriate patients, pain location, and prognosis are mandatory. However, indication and selection of the right technique demand knowledge, which is still incipient among clinicians. Peripheral neurolytic blocks should be considered only after a failure of other modalities, including pharmacologic, physical, psychiatric, and non-destructive interventional therapy. In selected cases, for example, in case of severe pain from pancreatic neoplasia, minimally invasive techniques (e.g., NCPB) must be considered at the beginning of the treatment path.
Enhancing Healthcare Team Outcomes
An interprofessional approach is fundamental for the success of the therapy. The professional figures involved are manifold and involve the pain therapist, the oncologist for the management of combined therapy, a nurse specialist in minimally-invasive procedures, an x-ray technologist. Very often, an interventional radiologist (e.g., CPB under CT guidance), and a palliative radiotherapist can be involved. In addition, psychological intervention is often required, especially for cancer patients who are subjected to enormous stress loads related to disease, pain, and consequent impairment of QoL.[41] This aspect is very important because, for the completion of the procedure and its successful outcome, it is essential to have the full patient's collaboration.