Continuing Education Activity
Subacromial bursitis is an inflammatory condition that is a common cause of shoulder pain. It is typically caused by repetitive overhead activities and minor trauma such as falls but the etiology can be multifactorial. This activity describes the evaluation and management of subacromial bursitis and highlights the role of the interprofessional team in evaluating and treating patients with this condition.
Objectives:
- Describe the etiologies of subacromial bursitis.
- Describe presenting symptoms of subacromial bursitis.
- Summarize the treatment considerations for patients with subacromial bursitis.
- Identify the importance of improving care coordination amongst the interprofessional team to enhance the delivery of care for patients affected by subacromial bursitis.
Introduction
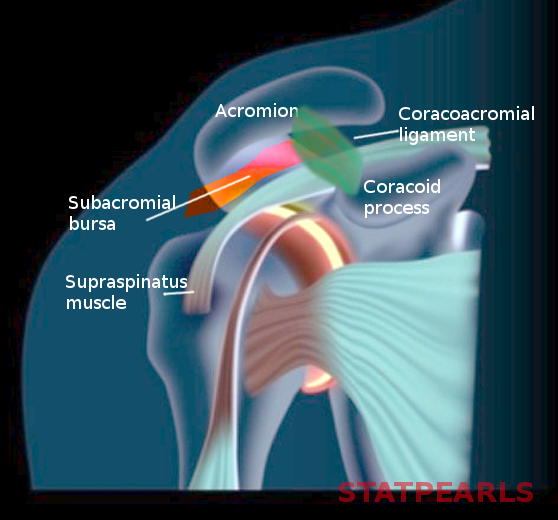
A bursa is a fluid-filled sac found at several locations in the human body. It serves to lubricate joints and body surfaces exposed to higher degrees of wear and friction. The subacromial space in the shoulder is such a location. The subacromial bursa is bordered superiorly by the acromion, coracoid, coracoacromial (CA) ligament and the proximal deltoid muscle fibers and inferiorly by the fibers of the supraspinatus muscle. The height of the subacromial space ranges from approximately 1.0 to 1.5 cm.[1] Inflammation of the bursa can occur due to a variety of reasons leading to the development of subacromial bursitis.
Etiology
Any process that causes inflammation of the subacromial bursa can lead to bursitis. Common etiologies include:
- Subacromial impingement
- Repetitive overhead activities/overuse
- Direct trauma
- Crystal deposition
- Subacromial hemorrhage
- Infection
- Autoimmune diseases (e.g., rheumatoid arthritis)
Epidemiology
Bursitis accounts for approximately 0.4% of all primary care visits. Gender prevalence is equal. It is seen more often in individuals who participate in repetitive overhead activities such as athletes, factory workers, and manual laborers. Older individuals are more prone to experiencing subacromial bursitis likely due to years of wear leading to an increase in subacromial impingement.
Pathophysiology
Any of the etiologies can lead to inflammation of the subacromial bursa, which causes increased fluid and collagen formation by the synovial cells of the bursa. The fluid is often rich in fibrin and can become hemorrhagic[2]. Bursitis can subdivide into three phases: acute, chronic and recurrent. The acute phase is marked by local inflammation with thickened synovial fluid. This condition results in painful movement, particularly with overhead activities as the bursa undergoes friction between the humeral head/supraspinatus inferiorly and acromion/deltoid superiorly. Chronic bursitis leads to the development of constant pain due to a chronic inflammatory process occurring in the bursa, which can also lead to weakness and eventual rupture of the surrounding ligaments and tendons. In cases of chronic bursitis, attention must be paid to tendinitis since these entities can be present simultaneously. Recurring bursitis can occur in patients exposed to repetitive trauma or routine overhead activities. It can also present in patients with inflammatory conditions such as rheumatoid arthritis.
Histopathology
Histopathologic studies are rarely used to diagnose subacromial bursitis. These studies are more relevant in cases of infection or in the setting of chronic or recurrent subacromial bursitis, where the etiology may not be apparent. In their research, Santavirta et al. demonstrated the presence of chronic mononuclear cell infiltrates in inflamed bursal tissue. Immunohistochemistry revealed these cells to be mainly CD2-positive T lymphocytes and less commonly CD11b macrophages/monocytes.[3]
History and Physical
A thorough history and physical is of vital importance since this condition is primarily a clinical diagnosis. Subacromial bursitis usually presents with pain in the anterolateral aspect of the shoulder. Patients may report sustaining trauma such as a fall with direct impact to the shoulder. A history of repetitive overhead activities such as overhead sports, lifting boxes, etc. may also clue the clinician towards the diagnosis.
Impingement syndrome is a common cause of subacromial bursitis. It results when the area of the subacromial space is decreased, mainly due to overhead activities. Abduction of the arm elevates the humerus, bringing it closer to the acromion, which effectively reduces the space under the acromion where the subacromial bursa and the supraspinatus muscle lie. The subacromial bursa serves its function by protecting the underlying supraspinatus muscle from attrition wear between the humeral head and the acromion. However, repetitive activity can lead to irritation and inflammation of the bursa, causing it to get inflamed. When considering impingement as a cause for subacromial bursitis, it is, therefore, essential to also include tendon pathology in the differential since concomitant supraspinatus tendinitis or tendon tear may be present.
On physical exam, the patient will have point tenderness at the anterolateral aspect of the shoulder below the acromion. The pain is localized and does not typically radiate to other parts of the shoulder or the arm (if the pain does radiate, one must include cervical spine pathology in the differential). The skin may also be warm or boggy at this site, although erythema is generally not seen. Pain is also elicited on resisted abduction of the arm beyond 75 to 80 degrees since during this arc of motion the subacromial bursa is compressed at the undersurface of the acromion.
Evaluation
Laboratory tests are unremarkable and are as such not generally indicated for making a diagnosis. If there is a concern for septic arthritis of the shoulder, joint aspiration, and synovial fluid analysis may be an option at that time.
Imaging may be performed but is, once again, not necessary to elucidate a diagnosis of simple subacromial bursitis. However, it may still be worthwhile to obtain X-rays of the shoulder to rule out other causes of shoulder pain including fractures, dislocations, osteoarthritis, etc. A bursa is a soft tissue structure and will not be visible on plain films unless calcification of the bursa is present. The morphology of the acromion can also be studied since certain anatomic variations can increase the likelihood of developing bursitis. The shape of the acromion can be flat (type 1), curved (type 2) or hooked (type 3). With a downward sloping curved or hooked acromion, less space is available in the subacromial space and the probability of developing subacromial bursitis increases.[4] The presence of an os acromiale, i.e., a lack of fusion of the acromion, can also be evaluated. An unstable os acromiale can cause subacromial impingement and lead to bursitis. Other imaging modalities including MRI and ultrasound can also be useful. Bursal fluid accumulation is visible on MRI.
Additionally, MRI is an excellent modality to assess the rotator cuff muscles and any tendon lesions that may be present. Ultrasound can be used to evaluate the thickness of the bursa. In asymptomatic shoulders, Tsai et al. found the average thickness of the subacromial bursa to be 0.75 +/- 0.23 mm. Comparatively, patients with bursitis had a bursal thickness of 1.27 +/- 0.41 mm.[5] Even though ultrasound is not frequently used to diagnose subacromial bursitis, it may be of value in the hands of a skilled clinician.
Treatment / Management
Nonoperative treatment is the usual treatment route for subacromial bursitis. Treatment modalities include rest, non-steroidal anti-inflammatory medications (NSAIDs), physical therapy, and corticosteroid injections.[6] Ultrasound therapy has also been utilized, although literature does not demonstrate it to be efficacious.[7] Operative treatment is only for recalcitrant cases not responsive to conservative treatment. A bursectomy may be performed either arthroscopically or via an open approach. If surgery is performed, additional procedures such as subacromial decompression, rotator cuff repair, etc. can be achieved if needed.
Differential Diagnosis
- Impingement syndrome
- Rotator cuff tendinitis/tear
- Biceps tendinitis
- Adhesive capsulitis
- Acromioclavicular joint osteoarthritis
Prognosis
The prognosis for subacromial bursitis is good. Most patients improve with conservative therapy while those that don’t achieve relief after undergoing operative treatment. Age also plays a role with older patients generally having poorer outcomes.[8] In general, the condition is self-limiting and does not have a long-term impact on the patient’s everyday life.
Complications
On the spectrum of shoulder pathologies, subacromial bursitis is not one that is associated with many complications. Repeated steroid injections always pose the theoretical risk of introducing an infection into the skin or shoulder joint. There is also a concern of damaging the rotator cuff muscles with recurrent injections. However, Bhatia et al. found no significant difference in the incidence of rotator cuff tears in patients who received fewer than or more than three subacromial corticosteroid injections.[9]
Deterrence and Patient Education
Subacromial bursitis is a common etiology of shoulder pain. It results from inflammation of the bursa, a sac of tissue present under the acromion process of the shoulder. It is usually brought about by repetitive overhead activities or trauma. Avoidance of such activities, rest and oral NSAIDs are effective in resolving the condition. Steroid injections and rarely surgery may be necessary in persistent cases.
Enhancing Healthcare Team Outcomes
Subacromial bursitis is a relatively benign condition that is easy to diagnose and treat. It is a frequent presentation in the orthopedist’s office, but patients may initially present to a primary care clinic, sports clinic or the emergency department. Treatment can be rendered in this setting efficiently and effectively. The primary care providers including the orthopedic nurse should educate the patient on methods to prevent this pathology. However, it is important not to miss other pathologies that can coexist such as tendon tears, since leaving these untreated will have a greater impact on the patient’s arm function, activities of daily living and thus, quality of life. Therefore, in cases where the bursitis is unable to be treated, or other pathologies are suspected, the patient should obtain a referral to an orthopedic surgeon for further care.
Subacromial bursitis is best managed by an interprofessional team that includes physicians, specialists, therapists, specialty-trained nursing, and pharmacists, engaged in a collaborative team effort to bring about the optimal care and the best possible patient outcomes.