Introduction
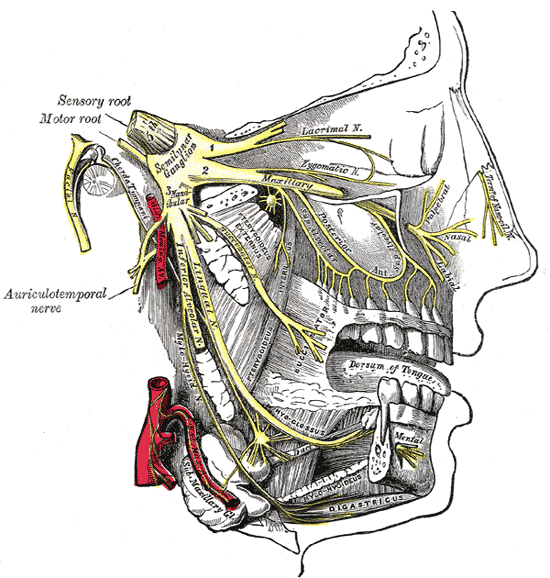
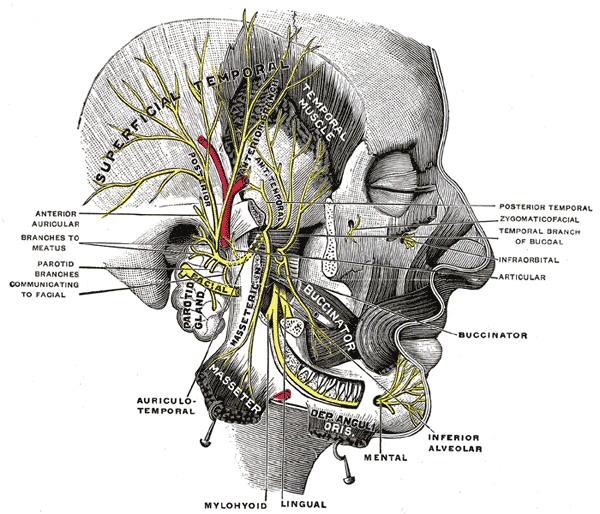
The trigeminal nerve is the fifth cranial nerve (CN V) and the largest of the cranial nerves. Its primary function is to provide sensory innervation to the face and is divided into three main branches. The different branches are the ophthalmic (V1), maxillary (V2), and mandibular (V3) nerves. These branches join at the trigeminal ganglia, which is located within the Meckel's cave of the middle cranial fossa.
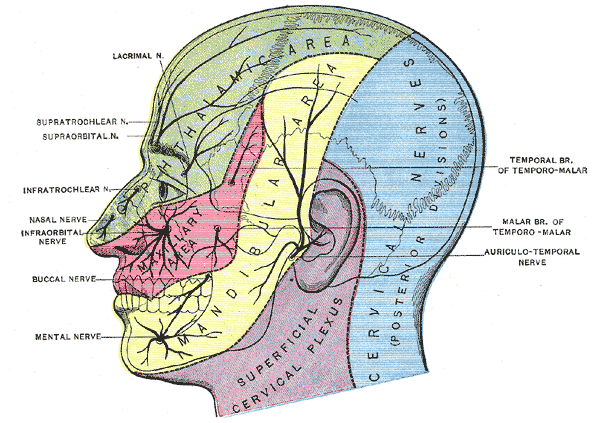
The ophthalmic nerve is responsible for sensory innervation of the face and skull above the palpebral fissure and the eye and portions of the nasal cavity. The maxillary nerve is also a sensory branch and innervates portions of the nasal cavity, sinuses, maxillary teeth, palate, and the middle portion of the face and skull above the mouth and below the forehead. The mandibular nerve is unique in that it contains both sensory and motor fibers. It provides sensory innervation of the buccal mucosa, mandibular teeth, and the skin below the mouth. The motor portion of V3 innervates all the muscles of mastication. This article aims to review the anatomy of the trigeminal nerve, its surgical considerations, and its clinical significance for providers.
Structure and Function
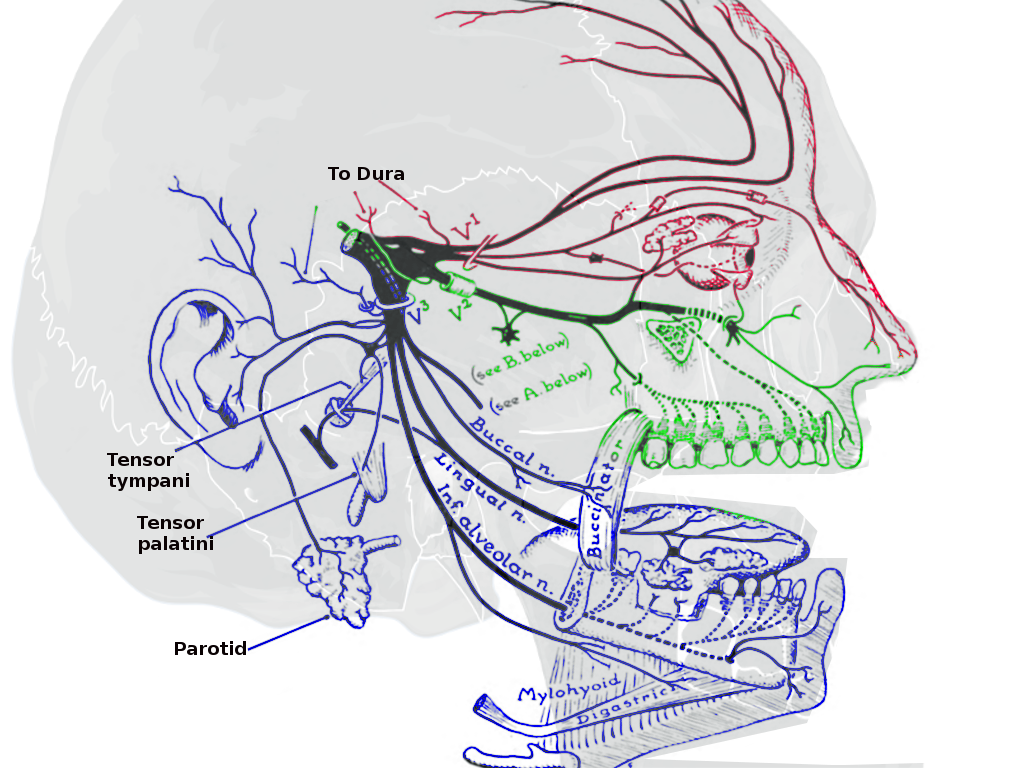
The trigeminal nerve is the largest of the cranial nerves and provides sensory and motor innervation to the muscles of mastication.[1] More specifically, the sensory information conducted by this nerve includes touch, pain, and temperature. This sensory information is relayed through the trigeminal nuclei before traveling to the thalamus and ultimately synapsing in the somatosensory cortex. The trigeminal nerve arises from the anterolateral surface of the mid-pons as a large sensory root (portio major) and a smaller motor root (portio minor).[2] The trigeminal nerve then travels through the prepontine and cerebellopontine angle cisterns before entering a cerebrospinal fluid (CSF) filled space called Meckel's cave via an opening in the dura mater referred to as "porus trigeminus."[2] Inside Meckel's cave, the trigeminal ganglion divides into three subdivisions of the trigeminal nerve: o (V1), maxillary (V2), and mandibular (V3) divisions.
Brainstem Nuclei
The brainstem contains the sensory and motor nuclei of the trigeminal nerve. The trigeminal nerve has three sensory nuclei: the principal sensory nucleus, the spinal trigeminal nucleus, and the mesencephalic nucleus.[1]
Principal Sensory Nucleus
The principal sensory nucleus is located lateral to the motor nucleus within the posterolateral surface of the pontine tegmentum. Fibers carrying fine touch and pressure synapse in the principal sensory nucleus and subsequently ascend in the trigeminal l, which decussates to the opposite side of the brainstem. The trigeminal l and the uncrossed dorsal trigeminothalamic tract both terminate in the ventroposteromedial (VPM) nucleus of the thalamus and ultimately synapse in the somatosensory cortex ipsilateral its respective thalamus.
Spinal Trigeminal Nucleus
The spinal trigeminal nucleus is a caudal extension of the principal sensory nucleus and descends from the lower pons to the upper cervical levels of the spinal cord (C2-4), connecting to the dorsal horn of the spinal cord.[2] The spinal trigeminal nucleus is further subdivided from rostral to caudal into the pars oralis, pars interpolaris, and pars caudalis.[3] The pars oralis spans from the mid-pontine level to the rostral third of the inferior olive in the medulla oblongata, the pars interpolaris is from the rostral third of the inferior olive to the obex, and the pars caudalis is from the obex to the upper cervical levels.[4] The spinal trigeminal nucleus is mainly dedicated to thermoceptive and nociceptive fibers for the face.
Mesencephalic Nucleus
The mesencephalic nucleus is a cephalad extension of the principal sensory nucleus spanning from the level of the superior colliculus in the upper midbrain to the middle pontine level.[2] The mesencephalic nucleus is unique in that it is the only known case in which primary sensory neurons are located within the central nervous system instead of in a peripheral ganglion. The mesencephalic nucleus receives proprioceptive fibers from the hard palate, teeth, periodontium, temporomandibular joint capsule, and Golgi tendon organs and muscle spindles from the extraocular and masticatory muscles.[5] The mesencephalic nucleus primarily projects to the motor trigeminal nucleus, but also the ipsilateral VPM of the thalamus and ultimately to the ipsilateral somatosensory cortex.
Motor Nucleus
The motor nucleus is located medial and anterior to the major trigeminal sensory nuclei within the lateral surface of the pontine tegmentum.[6]
CN V is classified into three different branches that have distinct territories of innervation. These branches are namely the ophthalmic (V1), maxillary (V2), and mandibular nerves (V3).[7][8][9][10]
Ophthalmic Nerve (V1)
The ophthalmic nerve (V1) is the smallest division of the trigeminal nerve. V1 is a purely sensory nerve that provides sensory innervation to the scalp, eye, nose, and forehead. It also contains sympathetic nerve fibers with contributions to pupillary dilation and supply to the ciliary body, iris, lacrimal gland, conjunctiva, and cornea. In addition to these superficial sensory functions, the ophthalmic nerve also supplies the superior portion of the nasal cavity, the frontal sinus, and even deeper structures, including the dura mater and portions of the anterior cranial fossa. It travels lateral to the abducens nerve within the lateral wall of the cavernous sinus, inferior to the oculomotor and trochlear nerves. V1 exits the skull through the superior orbital fissure and divides in the orbital apex into the lacrimal, frontal, and nasociliary nerves.[1]
Maxillary Nerve (V2)
The maxillary nerve (V2) is also a sensory branch, and it supplies the territory just below the orbits and above the mouth. This includes the inferior portion of the nasal cavity, the maxillary teeth, and the maxillary sinus. It travels inferior to V1 within the lateral wall of the cavernous sinus. V2 exits the skull base through the foramen rotundum, making it the only cranial nerve within the cavernous sinus not to exit through the superior orbital fissure and subsequently crosses the pterygopalatine fossa. V2 ultimately enters the face through the infraorbital foramen.[1]
Mandibular Nerve (V3)
The mandibular nerve (V3) is the largest branch of the trigeminal nerve. V3 is the only branch of the trigeminal nerve that has both sensory and motor components. V3 receives sensory information from the lower third of the face, the floor of the mouth and jaw, and the tongue. The motor root (portio minor) of V3 supplies the muscles of mastication (masseter, temporalis, pterygoids), as well as the anterior belly of the digastric muscle and the mylohyoid muscle.[11] The mandibular nerve (V3) exits the skull base through the foramen ovale.
Trigeminal Ganglion
The three divisions of the trigeminal nerve reach the trigeminal ganglion (Gasserion or semilunar ganglion), containing the cell bodies for most of the trigeminal sensory axons. The trigeminal ganglion is located within Meckel's cave, a CSF-filled space between two layers of dura mater over the petrous portion of the temporal bone. Meckel's cave encloses the trigeminal ganglion and the three trigeminal nerve roots. The trigeminal neurons in the trigeminal ganglion are pseudo-unipolar neurons with two axonal branches, one extending proximally to the brainstem and the other distally towards one of the trigeminal divisions.[5] As a result, trigeminal neurons are capable of conducting action potentials in both directions: orthodromically, with pain and temperature directed towards the brainstem, as well as antidromically, towards branches of the trigeminal divisions.[5]
Trigeminal Root
The trigeminal root carries sensory fibers extending from the trigeminal ganglion to the ventrolateral aspect of the pons. The trigeminal root entry zone (TREZ) is located at a distance of about 12 mm distal to the pons, where central myelin is replaced by peripheral myelin; it is considered the most vulnerable site along the nerve for neurovascular compression.[12]
Muscles
The mandibular nerve is the only branch of the trigeminal nerve with a motor component (V3). This branch supplies motor innervation to the facial muscles involved in mastication, which include the masseter, temporalis muscle, and lateral and medial pterygoids. Additionally, V3 gives off branches that innervate the tensor veli palatini, the mylohyoid, the tensor tympani, and the anterior portion of the digastric muscle.
Surgical Considerations
One of the most common surgical procedures related to the trigeminal nerve is a surgical intervention for trigeminal neuralgia. The types of surgical interventions for trigeminal neuralgia are divided into two categories: non-destructive and destructive. The goal of non-destructive surgery is to alleviate nerve compression by removing any structure that may be impinging on the nerve, typically the superior cerebellar artery, via a microvascular decompression. Destructive procedures include percutaneous rhizotomy and stereotactic radiosurgery to disrupt the trigeminal nerve completely so that the nerve no longer transmits pain. A destructive procedure results in the irreversible loss of sensation of the affected side of the face within the ablated nerve distribution.[13][14][15]
Clinical Significance
Corneal Polysynpatic Reflex
The corneal polysynaptic reflex results in bilateral closure of the eyelids following light touch to the cornea. Efferent input is from the ophthalmic division (V1) to the trigeminal ganglion projecting to the spinal trigeminal nucleus. There is then an indirect connection with the facial nuclei via lateral reticular formation interneurons, which project to the orbicularis oculi muscles, both ipsilateral (direct) and contralateral to corneal stimulation (consensual corneal response).[16]
Jaw-Jerk Monosynaptic Reflex
The jaw jerk reflex results in the closure of the jaw following sudden stretching of the masseter muscle. The trigeminal mesencephalic nucleus receives afferent impulses from the masticatory muscle spindles, which project onto the trigeminal motor nucleus. Efferent output is from the motor trigeminal nucleus through V3 to reach the masticatory muscles.
Trigeminal Neuralgia
Trigeminal neuralgia is a clinical condition characterized by sharp, electrical, shock-like, paroxysmal lancinating pain within the distribution of one or more of the trigeminal nerve branches. Most cases are due to compression of the trigeminal nerve at the root entry zone by the superior cerebellar artery. Other etiologies of trigeminal neuralgia include compression from an adjacent aneurysm, arteriovenous malformation, tumor, or due to intrinsic abnormality such as demyelinating multiple sclerosis plaques. Diagnosis is made based on the combination of clinical presentation and radiographic imaging, typically in the form of magnetic resonance imaging (MRI) of the brain with particular attention to the cisterns, which can be aided with MRI sequences such as Fast-Imaging-Employing-Steady-state-Acquisition (FIESTA).
Treatment of trigeminal neuralgia depends on the underlying etiology. First-line treatment is carbamazepine, and second-line medications include lamotrigine, oxcarbazepine, phenytoin, gabapentin, pregabalin, and baclofen.[15] Surgery may be an option if the pain becomes refractory to medications or the patient develops significant side effects secondary to the drugs.
Cluster Headache
Cluster headaches have a similar presentation to trigeminal neuralgia. Cluster headaches most often present as severe headache on one side of the head that affects the territory of the trigeminal nerve occurring in short intervals, often multiple times within the same day. These headaches can be accompanied by autonomic symptoms such as nasal congestion, swelling, and lacrimation on the affected side. While the cause of cluster headaches is currently unknown, there is often an external stimulus that triggers the onset of symptoms. Prophylactic treatment usually includes a combination of trigger avoidance and pharmacotherapy. Acute attacks can be remediated with fast-acting triptans and oxygen.
Lateral Medullary Syndrome (Wallenberg Syndrome)
The lateral medullary syndrome is a clinical syndrome that occurs when the lateral portion of the medulla in the brainstem becomes damaged, typically due to a stroke of the posterior inferior cerebellar artery or vertebral artery. A lesion in this region of the brain stem results in an ipsilateral sensory loss in the territory of the trigeminal nerve and contralateral sensory loss in the rest of the body, among other signs/symptoms, including vertigo, ataxia, horner syndrome, dysphagia, and hoarseness among others.