Continuing Education Activity
This comprehensive course covers hemifacial spasm (HFS), a neurological disorder characterized by paroxysmal, involuntary twitching of facial muscles on one side of the face, primarily innervated by the ipsilateral facial nerve (seventh cranial nerve). HFS, categorized as a subtype of peripheral (neuromuscular) movement disorders, poses challenges in diagnosis and management.
Participants get an in-depth exploration of HFS, beginning with its distinctive characteristics, causes, and diagnostic criteria. The course covers the rarity of bilateral involvement, occurring in less than 5% of severe hemifacial spasm cases, emphasizing the unilateral nature of this condition. Further, the activity reviews recommended interventions for HFS, encompassing medical, surgical, and therapeutic approaches. From pharmacological management to surgical options such as microvascular decompression, participants gain insights into evidence-based strategies for optimizing patient outcomes.
An aspect of this course is recognizing the interprofessional team's pivotal role in enhancing competence in HFS management. Neurologists, neurosurgeons, physical therapists, and nurses collaborate to address the multifaceted aspects of patient care. Effective communication, shared decision-making, and coordinated interventions are essential to ensuring holistic patient care. Through a collective understanding of diagnostic nuances, treatment modalities, and the varied perspectives of the interprofessional team, participants will gain competence to provide optimal care for individuals affected by HFS.
Objectives:
Identify hemifacial spasm's clinical manifestations and characteristic features for accurate and timely diagnosis.
Select appropriate treatment modalities for hemifacial spasm based on patient characteristics and preferences, aligning with the efficacy of interventions like botulinum toxin.
Differentiate hemifacial spasm from other facial movement disorders, ensuring a precise understanding of its unique characteristics.
Apply effective strategies to improve care coordination among interprofessional team members to use appropriate modalities to improve outcomes for patients affected by hemifacial spasm.
Introduction
Hemifacial spasm (HFS) is characterized by paroxysmal, involuntary twitching of facial muscles on one side of the face innervated by the ipsilateral facial nerve (seventh cranial nerve). The abnormal involuntary firing of the peripheral facial nerve triggers short or longer contractions of muscles of facial expression. HFS is considered a subtype of peripheral (neuromuscular) movement disorder. As the name suggests, the disorder is almost always unilateral except in some rare incidences, with a reported prevalence of 2.6% of all HFS cases, during which one can see the bilateral involvement of facial muscles.[1] This condition generally does not cause significant physical disability, yet it often causes social embarrassment, resulting in severe psychosocial issues for the patient.
Etiology
Primary Hemifacial Spasm
The most common etiology of HFS is compression of the facial nerve that exits the brainstem by an ectatic or aberrant artery. The typical aberrant arterial anomalies leading to facial nerve root compression are the branches of the anterior inferior cerebellar artery, posterior inferior cerebellar artery, and vestibular artery, among others. The point where the facial nerve exits the brainstem, often called the root-exit zone, is only covered with the arachnoid membrane without the epineurium. There are no connective tissue septa between the nerve fascicles; this is also the zone of transition between central and peripheral myelin, produced by oligodendrocytes and Schwann cells, respectively. These unique properties make the nerve susceptible to any trigger, such as nerve compression or irritation.[2]
Secondary Hemifacial Spasm
HFS can occur secondary to the following etiologies:
- Trauma
- Late sequelae to Bell palsy
- Structural lesions along the course of the facial nerve, especially a benign tumor pressing on the intracranial portion of the nerve
- Arteriovenous anomalies, intracranial arterial aneurysm, arterio-venous fistula, angiomas
- Mastoid and ear infections (otitis media, cholesteatoma)
- Parotid gland tumors
- Chiari malformation and other structural anomalies of the posterior cranial fossa
- Brainstem lesions such as demyelinating plaques of multiple sclerosis [3][4]
Epidemiology
HFS is a rare condition, as the estimated worldwide prevalence of HFS is 14.5 per 100,000 women and 7.4 per 100,000 men—suggesting women are twice as prone to have HFS than men.[5] As reported in some studies, those in the Asian population have a slightly higher prevalence as compared to Caucasian populations for unknown reasons.[6][7] Most cases of HFS are sporadic; however, there are some rare case reports of familial HFS in the scientific literature.
The disease onset, especially in primary HFS, usually begins in adulthood, around the fourth through sixth decades of life. This condition commonly involves the left side more than the right, as observed in most reported cases. Researchers have reported that 40% of patients with HFS have coexisting hypertension.
Pathophysiology
Chronic irritation of the facial nerve fascicle and proximal nerve segment at the root-exit zone is the primary pathophysiologic mechanism of HFS. The root-exit zone, where the facial nerve exits the brainstem, is only covered with the arachnoid membrane without the epineurium. Compression of the facial nerve root at the junction of the central (point of exit from brainstem) and peripheral segment (root exit/entry zone) by aberrant/ectatic blood vessels is the most common cause of HFS, as reported in the literature.[8] There are no connective tissue septa between the nerve fascicles, and this is also the zone of transition between central and peripheral myelin, produced by oligodendrocytes and Schwann cells, respectively. These special properties make the nerve susceptible to any trigger, such as nerve compression or irritation.[2] Several theories have been proposed to explain the pathophysiological mechanism by which facial nerve compression leads to HFS.
Nerve Origin Hypothesis/Peripheral Theory
As proposed in this theory, the ephaptic transmission of impulses, or the lateral spread of excitation to adjacent nerve fibers, leads to abnormally excessive firing of the facial nerve; this firing is due to the facial nerve's demyelination at the compression site.[9] Myelin is an insulating material that plays an essential role during nerve impulse conduction by preventing abnormal lateral spread that results in ectopic transmission of impulses that, in turn, cause HFS.
Nuclear Origin Hypothesis/Central Theory
Irritation of peripheral afferent facial nerve fibers leads to aberrant signaling to the central facial nerve nucleus, inducing abnormal firing of the nucleus. This facial nucleus hyperexcitability results in involuntary myoclonic contraction of facial muscle on the affected side.[10]
Hemifacial Spasm Secondary to Bell Palsy
Bell palsy has a clinically similar appearance to other HFS, yet the pathophysiology is different. Strightly speaking, this condition is not a real HFS but a synkinesis. With more severe Bell palsy, there is pathological axonal damage. When the axon regenerates during recovery, regeneration may not occur along the original branches. Consequently, the branch to the orbicularis oculi may regenerate to the orbicularis oris, a process of aberrant reinnervation. When the eye blinks, the orbicularis oris muscle or other lower facial muscles may contract simultaneously or vice versa as the orbicularis oculi muscle, a phenomenon called synkinesis.[11]
History and Physical
Clinical Features of Hemifacial Spasm
Classically, the involuntary tonic/clonic contractions of one side of the face begin with the involvement of orbicularis oculi, leading to brief, intermittent, painless, and involuntary closure of the ipsilateral eye. This involuntary action is associated with infrequent eyebrow elevation and eye twitching. Further, this is known as the "other Babinski sign," named after Joseph Babinski, who first described it in 1905. "Other Babinski sign" is pathognomic of HFS and helps distinguish from eye twitching/closure due to blepharospasm, in which browlift is characteristically absent.
Over several months to years, the irregular tonic/clonic contractions gradually progress and involve lower facial muscles such as perioral muscles (orbicularis oris, mentalis, zygomaticus major, platysma). When the symptoms worsen, there is often involuntarily forced eyelid closure, similar to blepharospasm. The "other Babinski sign" will be most helpful in the differential diagnosis.
In secondary HFS, both the upper and lower face develop synchronous, intermittent contractions, eventually leading to sustained spasms as the disease progresses. The persistence of contractions during sleep is one of the characteristics of hemifacial spasm that distinguishes it from most movement disorders. This may predispose the individual to disturbed sleep and insomnia. In advanced cases, facial deviation/asymmetry and grimacing are evident due to the pull of contracted muscles on one side. Visible asymmetry occurs due to contracted muscles on one side in HFS. Uncommon symptoms, including a clicking sound in the ear (resulting from stapedius involvement), ear pain, and hearing loss, are reported in certain instances of secondary hemifacial spasms. Symptoms are typically worsened by stress, fatigue, eating, and anxiety. Relaxation techniques or simply touching the face subsides the spasm/twitching.
Hemifacial Spasm Following Bell Palsy
Following a more severe Bell palsy, some patients may start to have involuntary twitching of the side of the face affected by the prior Bell palsy. This twitching resembles HFS with its involuntary contraction of the facial muscles. However, the pathophysiology and clinical appearance are completely different. The abnormal facial movement after Bell palsy is synkinesis caused by aberrant reinnervation of the facial nerve so that when the eye blinks, the orbicularis oris muscle or other lower facial muscles may contract simultaneously or vice versa as the orbicularis oculi.[11]
Association of HFS and Hypertension
Results from studies indicate that 40% of individuals with HFS also have concurrent hypertension. Therefore, it is crucial to assess the presence of hypertension in the patient.
Evaluation
Diagnosis of HFS is made clinically based on the detailed history coupled with a neurological and local physical examination. Rarely is electrophysiological testing indicated as the diagnosis is made clinically. An electromyogram can be used in the early stages of the disease when it is difficult to distinguish clinically from facial myokymia, blepharospasm, complex partial motor seizures, or motor tics. The diagnostic finding on electrophysiological testing is lateral spread and variable synkinesis on blink reflex testing. Stimulation of one branch of the facial nerve leads to the contraction of facial muscles supplied by a different branch. Needle electromyogram characteristically shows irregular, brief motor unit potentials with high frequency (150-400 Hz), and facial twitching can be clinically correlated with this finding.
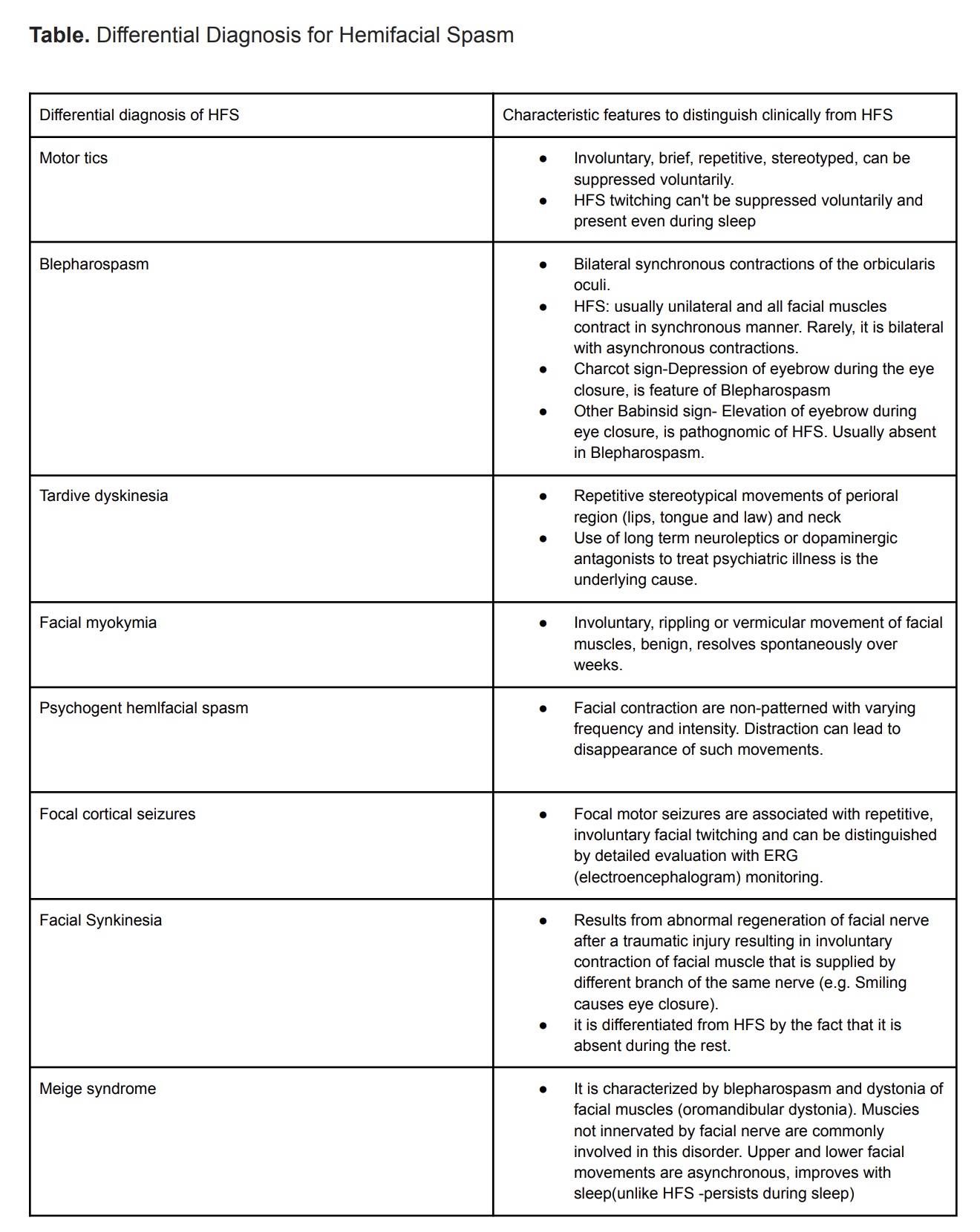
Accurate diagnosis is important as many conditions can mimic HFS (see Table. DDX for Hemifacial Spasm). Where there is suspected facial nerve compression, rule out an underlying structural lesion, especially a benign tumor at the brainstem nerve root exit zone or near the cerebellopontine angle.[12] A brain magnetic resonance imaging scan is the best diagnostic study to rule out structural causes that may need surgical therapy or lesions indicating multiple sclerosis. Computed tomography or magnetic resonance angiography is generally not indicated. In most cases of primary HFS, the computerized tomography and magnetic resonance angiography scans report will be unremarkable because a vascular loop lying close to the facial nerve is commonly found even in individuals without HFS. Magnetic resonance angiography is reserved for patients scheduled for microvascular decompression surgeries. A 3D time-of-flight magnetic resonance angiography with high-resolution T2-weighted images would be very helpful for the preoperative evaluation of microvascular decompression.[13]
Treatment / Management
The primary treatment goal for HFS is to reduce the muscle contractions resulting from abnormal impulse transmissions to adjacent neurons (ephaptic transmission). This treatment can be approached medically or surgically based on the underlying etiology and severity of the disorder.
Medical Management
Botulinum Neurotoxin Injections in Hemifacial Spasm
The advent of botulinum neurotoxin (botox) has revolutionized managing HFS. Injecting botox has become a first choice among clinicians and patients due to its efficacy and few adverse events. Botox treatment has achieved notable symptomatic improvements in 85% to 95% of patients in various clinical trials.[14] A thorough evaluation to exclude the secondary causes, such as tumors or vascular malformations, is essential before botox treatment.
Botox is a simple and noninvasive procedure injected in affected muscles, most commonly the orbicularis oculi (upper and lower eyelids), corrugator, frontalis, zygomaticus major, buccinators, and masseter.[15] However, the patient should be forewarned about adverse events, such as ptosis, temporary bruising, swelling, facial asymmetry, asymmetric eyebrows, and facial weakness, among others—which are mild and transient.
The most commonly used botox used to treat HFS is onabotulinumtoxinA. Other commercially available botox preparations include rimabotulinumtoxinB and abobotulinumtoxinA. Botox acts on the presynaptic terminal at the neuromuscular junction and blocks the calcium-mediated release of the presynaptic neurotransmitter acetylcholine, leading to non-conduction of a nerve impulse across the neuromuscular junction leading to temporary paralysis of muscles supplied. This chemodenervation effect usually lasts 3 to 6 months and reverses back to baseline.
Botox has a dual benefit as it also reportedly reduces depression among patients with HFS. The theory postulated includes 2 ways by which botox alleviates depression. The first is by providing symptomatic relief, leading to less social embarrassment. The other possible mechanism is via reducing the activation of the amygdala, as increased activation can cause depression and anxiety. Botox causes chemical denervation in adjacent muscles of the face, interrupting afferent sensory information to the trigeminal tract, leading to reduced trigeminal sensory input to the brainstem and amygdala.
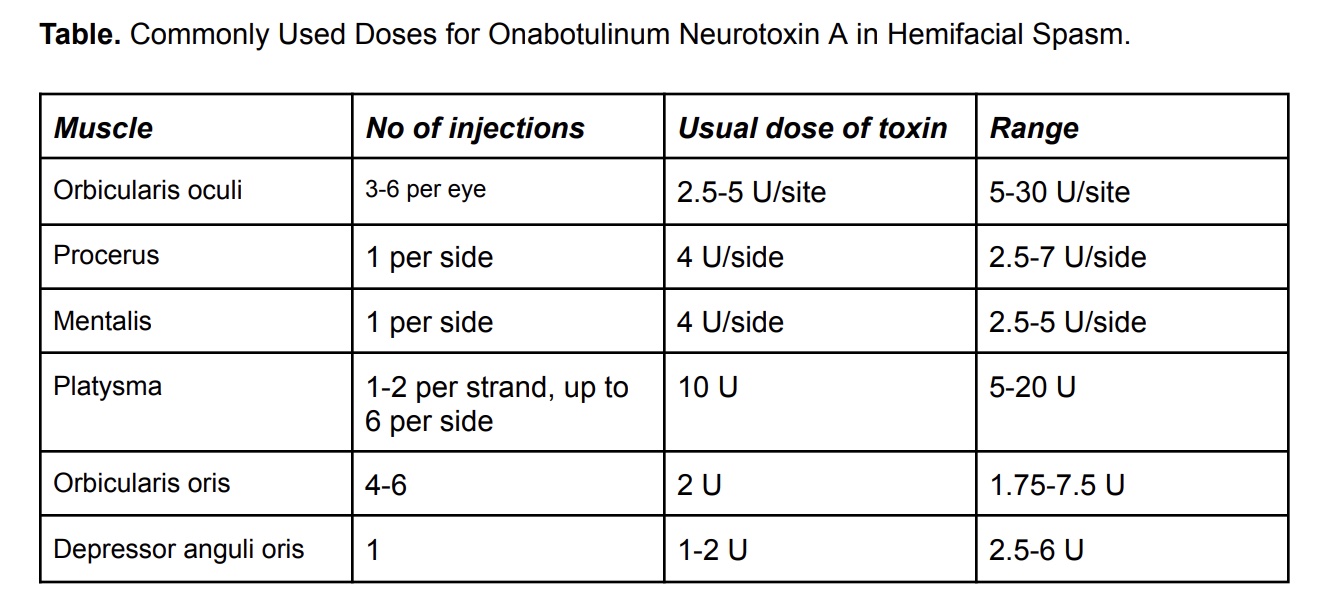
Dosing and Scheduling of Botoxin Injections
The usual dose of onabotulinum neurotoxin A is 10 to 36 U. There is a need for repetitive injections scheduled at intervals of 3 to 6 months. Some physicians prefer flexible dosing intervals ranging from 6 to 20 weeks as lasting effects vary. The symptomatic improvement after botox injection is evident 3 to 6 days after the injection and reaches a peak after 2 weeks (see Table. Onabotulinum Neurotoxin A Dosing).[16]
Oral Medications
Traditionally, the treatment of HFS, especially in the mild form and early stages, was oral medications. Commonly prescribed oral medications include anticonvulsants such as carbamazepine, gabapentin, benzodiazepines (clonazepam), anticholinergics, baclofen, and haloperidol. These drugs have some efficacy in relieving the spasm, but the results are inconsistent. The major drawback of most of these medications is adverse events such as excessive sedation, fatigue, and dependency associated with their long-term use. Oral medications can be considered as first-line therapy for those who are unwilling to undergo botox therapy and are not good candidates for surgery.
Surgical Management
Surgical treatment is the only permanent treatment solution that addresses the underlying cause and is preferred in most severe cases of HFS and those refractory to botox therapy. The procedure of choice is microvascular decompression, which entails releasing the facial nerve from the compression of the aberrant vessel at the root exit zone of the brainstem. As discussed earlier in electrophysiological findings, the lateral spreading response results from the ephaptic transmission of nerve signals to neighboring neurons due to compression-related demyelination of the facial nerve root at the exit/entry zone. When such compression is relieved, the lateral spreading response on nerve stimulation will disappear. A high-resolution 3D time-of-flight magnetic resonance angiogram with high-resolution T2-weighted imaging may improve the visualization of the aberrant vessel preoperatively.[13] Following the first year after surgery, the average success rate of microvascular decompression surgery is reported to be 80% to 88%.[17]
There are issues associated with any invasive procedure. In addition to risks related to anesthesia, adverse effects specific to this complex procedure may include transient or permanent facial nerve palsy, hearing loss, cerebrospinal leakage, and recurrence of symptoms. Recurrent HFS rarely develops (1%) when patients remain asymptomatic for at least 2 years after surgery.[18]
Differential Diagnosis
Accurate diagnosis is important to help plan effective treatment for HFS. Many conditions can mimic HFS (see Table. DDX for Hemifacial Spasm). When a patient younger than 40 years presents with HFS, clinicians must evaluate the possibility of multiple sclerosis. However, this condition is rarely reported with the initial presentation as HFS. Demyelinating plaques in the brain stem region can involve the facial nerve roots, leading to aberrant signaling that results in HFS.
Prognosis
Although hemifacial spasm is known for a chronically progressive course, rare spontaneous resolution can be seen in up to 10% of cases.[16] The patient needs to be counseled about this relatively benign but persistent condition.[19] Facilitating patient understanding that the most effective and straightforward therapy involves repeated botox injections every 3 to 6 months. Microvascular surgery may be considered only when the HFS is not responding well to botox injections or the patient no longer prefers repeated injections.
Consultations
A neurovascular surgery consult is indicated if microvascular decompressive surgery is considered.
Deterrence and Patient Education
Timely diagnosis and management are essential as HFS is associated with social embarrassment, anxiety, and depression due to disability. In severe cases, persistent eye closure results in functional blindness and can be dangerous to the patient and surroundings, especially while driving or operating heavy machinery. While injecting botox has become the preferred management strategy due to its efficacy, the frequent repetition of procedures and high cost are the 2 major drawbacks of this therapy. If considering surgical intervention, patients must be fully educated on and comprehend the benefits and risks associated with an invasive and intricate microvascular decompression surgery that involves a craniotomy.
Pearls and Other Issues
Key facts to keep in mind regarding HFS include the following:
- HFS is an involuntary, repetitive contraction of facial muscles, almost always unilateral, non-suppressible, and persists even during sleep. In most cases, the underlying etiology is a facial nerve compression by an aberrant or ectatic blood vessel at the exit from the brainstem.
- The diagnosis is usually clinically based on a patient's history and physical exam. EMG and magnetic resonance imaging are conducted to identify or rule out the underlying cause before planning the treatment.
- In many cases, the condition leads to significant social embarrassment, anxiety, and depression among the patients. In most severe cases, functional blindness resulting from sudden, persistent, involuntary eye closure might be risky to the patient and others, such as while driving. Accurate diagnosis, timely management, and patient education are key elements to improve the quality of life of these patients.
- Botox is the treatment of choice for HFS due to its tremendous efficacy (success rate of 85% to 95%) and low incidence of adverse events. However, botox gives only temporary symptomatic relief. OnabotulinumtoxinA is the most widely used commercially available botox in the United States.
- Microvascular decompression is the only therapeutic modality that addresses the underlying cause, thereby leading to a complete cure with an average success rate of 85%.
Enhancing Healthcare Team Outcomes
Although a rare movement disorder, physicians must be aware of HFS as this condition can be misinterpreted with several other facial movement disorders, such as blepharospasm, motor tics, and facial myokymia. Patients often present to primary care providers and are referred to otolaryngologists or neurologists. Radiologists assist in the interpretation of imaging. Specialty-trained nurses may be involved in evaluating, treating, and educating patients with this condition. Pharmacists may assist in education of medication administration with particular consideration to polypharmacy. This interprofessional team is essential for optimal care of patients with HFS.
The local botox injection is the favored treatment of choice by patients and physicians. A systemic review of the literature shows only 2 high-quality studies showing HFS (one class II study and one class III study) as an indication to be treated with a botox.[14] The American Academy of Neurology's evidence-based treatment guidelines for HFS recommend that botox be offered as a treatment option.[14]