Continuing Education Activity
A delay in conduction between the atria and ventricles results in an atrioventricular conduction block. This is indicated by a prolongation of the PR interval on electrocardiogram. Conduction blocks are classified as either first-degree, second-degree, or third-degree blocks. There are two types of second-degree atrioventricular blocks: Mobitz type I, also known as Wenckebach and Mobitz type II. This activity examines when this condition should be considered on differential diagnosis and how to properly evaluate for it. This activity highlights the role of the interprofessional team in caring for patients with this condition.
Objectives:
- Identify the etiology of second-degree atrioventricular blocks.
- Explain how to identify each type of second-degree atrioventricular blocks on electrocardiogram.
- Explain the management of second-degree atrioventricular blocks.
- Explain the need for a well-integrated, interprofessional team approach to improve care for patients with second-degree atrioventricular blocks.
Introduction
An electrical impulse from the sinoatrial node has to travel through the atria, to the atrioventricular node, and down the His-Purkinje system to reach the ventricles and create a ventricular contraction. This process is reflected on ECG as the PR interval which leads to a QRS complex. A delay in conduction in this system results in an atrioventricular conduction block or a prolongation of the PR interval on ECG. Conduction blocks are classified as either first-degree block, second-degree block, or third-degree block. The second-degree atrioventricular block is the focus of this activity. There are two types of second-degree atrioventricular blocks: Mobitz type I, also known as, Wenckebach and Mobitz type II.[1][2][3][4][5]
In general, patients with second degree AV block may have no symptoms or may experience symptoms like syncope and lightheadedness.The second degree heart block may be temporary or permanent, depending on the impairment of the conduction system.
The mobitz type ll block does have the potential to progress to a complete heart block and if unrecognized, can lead to death.
Etiology
Mobitz type I (Wenckebach) is often a normal variant and seen in individuals with a high vagal tone without evidence of structural heart disease. However, this rhythm can result from inferior myocardial ischemia, medication toxicity (AV nodal blocking agents), hyperkalemia, cardiomyopathy (Lyme disease), or following cardiac surgery.
Common drugs that are known to cause AV block include beta-blockers, digoxin, calcium channel blockers, and many antiarrhythmic agents. Recently the immunosuppressant agent, fingolimod, used to treat relapsing multiple sclerosis was also found to cause AV block.
Mobitz type II is rarely seen in patients without structural heart disease. It is often associated with myocardial ischemia and fibrosis or sclerosis of the myocardium. This rhythm often progresses to third-degree atrioventricular block.
Other causes of AV block include the following:
- Infiltrative heart disease- amyloidosis, hemochromatosis
- Acute rheumatic fever
- Malignancies- lymphoma
- Hyperthyroidism, myxedema
- Collagen vascular disorders
- Cardiac tumors
- Following transcatheter placement of valves
- Ethanol injection for hypertrophic cardiomyopathy
Genes
In some patients, the AV conduction block may have a genetic trait. Several mutations in the SCN5A gene have been linked to familial AV conduction block.
Epidemiology
There have not been large population-based studies on the prevalence of Mobitz type I or II atrioventricular blocks. At this time, there is no associated age, racial, or gender correlation. AV block is sometimes seen in athletes and in patients with congenital heart disorders.
Pathophysiology
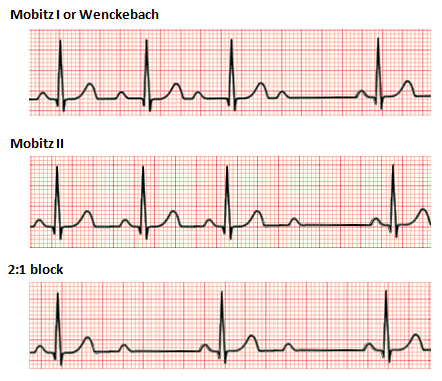
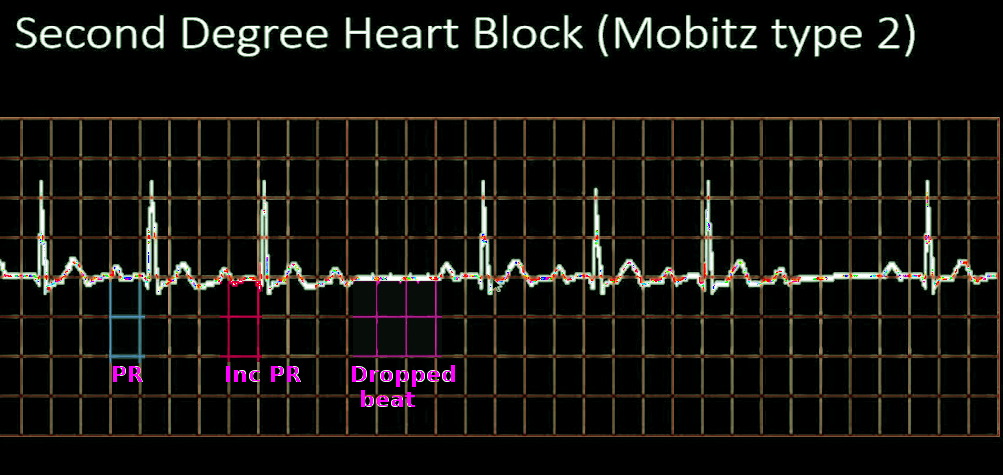
In Mobitz type I (Wenckebach) there is a progressive prolongation of the PR interval (AV conduction) until eventually an atrial impulse is completely blocked. When an atrial impulse is completely blocked there will be a P wave without a QRS complex. This pattern is often referred to as a “dropped beat.” Mobitz type I occurs because each depolarization results in the prolongation of the refractory period of the atrioventricular (AV) node. When an atrial impulse comes through the AV node during the relative refractory period, the impulse will be conducted more slowly, resulting in a prolongation of the PR interval. Eventually, an impulse comes when the AV node is in its absolute refractory period and will not be conducted. This will manifest on the ECG as a P wave that is not followed by a QRS complex. This non-conducted impulse allows time for the AV node to reset, and the cycle continues. This phenomenon leads to a grouped beating.
In Mobitz type II there is a constant PR interval across the rhythm strip both before and after the non-conducted atrial beat. Each P wave is associated with a QRS complex until there is one atrial conduction or P wave that is not followed by a QRS. Mobitz type II is often a problem in the infra-nodal conduction system, and therefore, is associated with a widened QRS complex, bundle-branch block, or fascicular block. Be aware that if more than one P wave is not conducted this is no longer a Mobitz type II and is considered a high degree AV block.
History and Physical
Questions should involve any history of cardiac disease both current and congenital, recent cardiac procedures and current medications. Patients with Mobitz type II often present with fatigue, dyspnea, chest pain, presyncope or syncope, and even sudden cardiac arrest.
Physical examination will often reveal bradycardia. Patients who have severe bradycardia resulting in hypotension and decreased cardiac output may be diaphoretic and pale. Patients who have a second-degree atrioventricular block secondary to myocardial ischemia may present with chest pain.
Evaluation
ECG is used to determine if a second-degree AV block is present. If ischemia is suspected based on the clinical picture and/or ECG findings, then cardiac biomarkers and chest radiography may be indicated. Serum electrolytes, calcium, and magnesium should be checked. If a patient is on digoxin, a level should be obtained to evaluate for toxicity. Routine imaging is not required for initial evaluation of second-degree atrioventricular block.[6][7][8][9]
Electrophysiologic testing is sometimes done to determine the level of the block and the need for a pacemaker.
Treatment / Management
Treatment for a Mobitz type I (Wenckebach) is often not necessary. Occasionally type I blocks may result in bradycardia leading to hypotension. If hypotension and bradycardia occur, type I blocks respond well to atropine. If unresponsive to atropine, pacing (transcutaneous or transvenous) should be initiated for stabilization.
If the patient is on any beta blockers, calcium channel blockers or digoxin, the dose of these medications should be reduced or the medication discontinued. All patients with Mobitz 1 block should be admitted and monitored.
Treatment for a Mobitz type II involves initiating pacing as soon as this rhythm is identified. Type II blocks imply structural damage to the AV conduction system. This rhythm often deteriorates into complete heart block. These patients require transvenous pacing until a permanent pacemaker is placed. Unlike Mobitz type I (Wenckebach), patients that are bradycardic and hypotensive with a Mobitz type II rhythm often do not respond to atropine.
Differential Diagnosis
Differential diagnosis includes congenital heart block, sinoatrial exit block, non-conducted premature atrial complexes, first-degree atrioventricular block, myocardial infarction, medication toxicity, and third-degree atrioventricular block.
Prognosis
The prognosis for Mobitz type I (Wenckebach) is excellent. This is usually asymptomatic and requires no intervention in asymptomatic patients.
The prognosis for Mobitz type II varies based on the cause of the rhythm. Patients require placement of implanted pacemaker devices to avoid complications of Mobitz type II AV blocks such as decreased cardiac output, symptomatic bradycardia, and sudden cardiac arrest.
Complications
- Complete heart block
- Syncope
- Dizziness
- Chest pain
- Death
Postoperative and Rehabilitation Care
All patients with AV block need lifelong follow up.
Consultations
Once an AV block has been identified, the cardiologist should be consulted for management.
Pearls and Other Issues
It can often be challenging to separate the two types of second-degree AV blocks. A rhyme is often used to remember type I or Wenckebach: “longer, longer, longer, DROP, now you have a Wenckebach.” This rhyme is alluding to the progressive prolongation of the PR interval before a non-conducted beat or the lack of a QRS complex after a P wave.
When a Mobitz type I has a fixed conduction ratio of 2:1, meaning 2 conducted beats to one non-conducted beat, it is difficult to differentiate between type I and type II. In this scenario, it is recommended to assume the worst-case scenario and call this rhythm a “non-typeable second-degree AV block.” This should be managed like a type II with transcutaneous or transvenous pacing until further workup can be completed.
Enhancing Healthcare Team Outcomes
The diagnosis and management of second-degree heart block is made by an interprofessional team that includes a cardiologist, ICU nurse, and an internist. When patients are diagnosed with a heart block, an appropriate referral to a cardiologist is highly recommended. [10]
In the emergency room type 1 Mobitz block without symptoms requires no treatment. However, symptomatic patients may be managed with atropine or transvenous pacing and a cardiology consult should be obtained. The patient must be admitted to a monitored unit.
All patients with type ll Mobitz block need admission and treatment. Nurses should be aware of this type of block and its treatment. Hypotension and bradycardia are often resistant to atropine and transvenous pacing can be life-saving. The pharmacist should ensure that the patient is on no medication that can aggravate or trigger the heart block. In addition, the patient must be educated on both types 1 and 2 heart block and their management. Close communication between the team members is vital to prevent mortality.
The prognosis for Mobitz type I (Wenckebach) is excellent. This is usually asymptomatic and requires no intervention in asymptomatic patients.
The prognosis for Mobitz type II varies based on the cause of the rhythm. Patients require placement of implanted pacemaker devices to avoid complications of Mobitz type II AV blocks such as decreased cardiac output, symptomatic bradycardia, and sudden cardiac arrest.