[1]
Bicalho E. The Intraosseous Dysfunction in the Osteopathic Perspective: Mechanisms Implicating the Bone Tissue. Cureus. 2020 Jan 24:12(1):e6760. doi: 10.7759/cureus.6760. Epub 2020 Jan 24
[PubMed PMID: 32140328]
Level 3 (low-level) evidence
[2]
Fischer C. [General fracture principles and imaging characteristics]. Der Radiologe. 2020 Jun:60(6):477-486. doi: 10.1007/s00117-020-00694-2. Epub
[PubMed PMID: 32415316]
[3]
Flis M, Gugała D, Muszyński S, Dobrowolski P, Kwiecień M, Grela ER, Tomaszewska E. The Influence of the Partial Replacing of Inorganic Salts of Calcium, Zinc, Iron, and Copper with Amino Acid Complexes on Bone Development in Male Pheasants from Aviary Breeding. Animals : an open access journal from MDPI. 2019 May 13:9(5):. doi: 10.3390/ani9050237. Epub 2019 May 13
[PubMed PMID: 31086121]
Level 3 (low-level) evidence
[5]
Orlandi-Oliveras G, Nacarino-Meneses C, Koufos GD, Köhler M. Bone histology provides insights into the life history mechanisms underlying dwarfing in hipparionins. Scientific reports. 2018 Nov 21:8(1):17203. doi: 10.1038/s41598-018-35347-x. Epub 2018 Nov 21
[PubMed PMID: 30464210]
[6]
Buckwalter JA, Cooper RR. Bone structure and function. Instructional course lectures. 1987:36():27-48
[PubMed PMID: 3325555]
[7]
Vico L, van Rietbergen B, Vilayphiou N, Linossier MT, Locrelle H, Normand M, Zouch M, Gerbaix M, Bonnet N, Novikov V, Thomas T, Vassilieva G. Cortical and Trabecular Bone Microstructure Did Not Recover at Weight-Bearing Skeletal Sites and Progressively Deteriorated at Non-Weight-Bearing Sites During the Year Following International Space Station Missions. Journal of bone and mineral research : the official journal of the American Society for Bone and Mineral Research. 2017 Oct:32(10):2010-2021. doi: 10.1002/jbmr.3188. Epub 2017 Jun 28
[PubMed PMID: 28574653]
[9]
Henrichsen JL, Wilhem SK, Siljander MP, Kalma JJ, Karadsheh MS. Treatment of Patella Fractures. Orthopedics. 2018 Nov 1:41(6):e747-e755. doi: 10.3928/01477447-20181010-08. Epub 2018 Oct 16
[PubMed PMID: 30321439]
[10]
Sui Z, Sun H, Weng Y, Zhang X, Sun M, Sun R, Zhao B, Liang Z, Zhang Y, Li C, Zhang L. Quantitative proteomics analysis of deer antlerogenic periosteal cells reveals potential bioactive factors in velvet antlers. Journal of chromatography. A. 2020 Jan 4:1609():460496. doi: 10.1016/j.chroma.2019.460496. Epub 2019 Aug 28
[PubMed PMID: 31519406]
[11]
de Baat P, Heijboer MP, de Baat C. [Development, physiology, and cell activity of bone]. Nederlands tijdschrift voor tandheelkunde. 2005 Jul:112(7):258-63
[PubMed PMID: 16047964]
[12]
Bahney CS, Zondervan RL, Allison P, Theologis A, Ashley JW, Ahn J, Miclau T, Marcucio RS, Hankenson KD. Cellular biology of fracture healing. Journal of orthopaedic research : official publication of the Orthopaedic Research Society. 2019 Jan:37(1):35-50. doi: 10.1002/jor.24170. Epub 2018 Nov 30
[PubMed PMID: 30370699]
[13]
Cooper KL, Oh S, Sung Y, Dasari RR, Kirschner MW, Tabin CJ. Multiple phases of chondrocyte enlargement underlie differences in skeletal proportions. Nature. 2013 Mar 21:495(7441):375-8. doi: 10.1038/nature11940. Epub 2013 Mar 13
[PubMed PMID: 23485973]
[14]
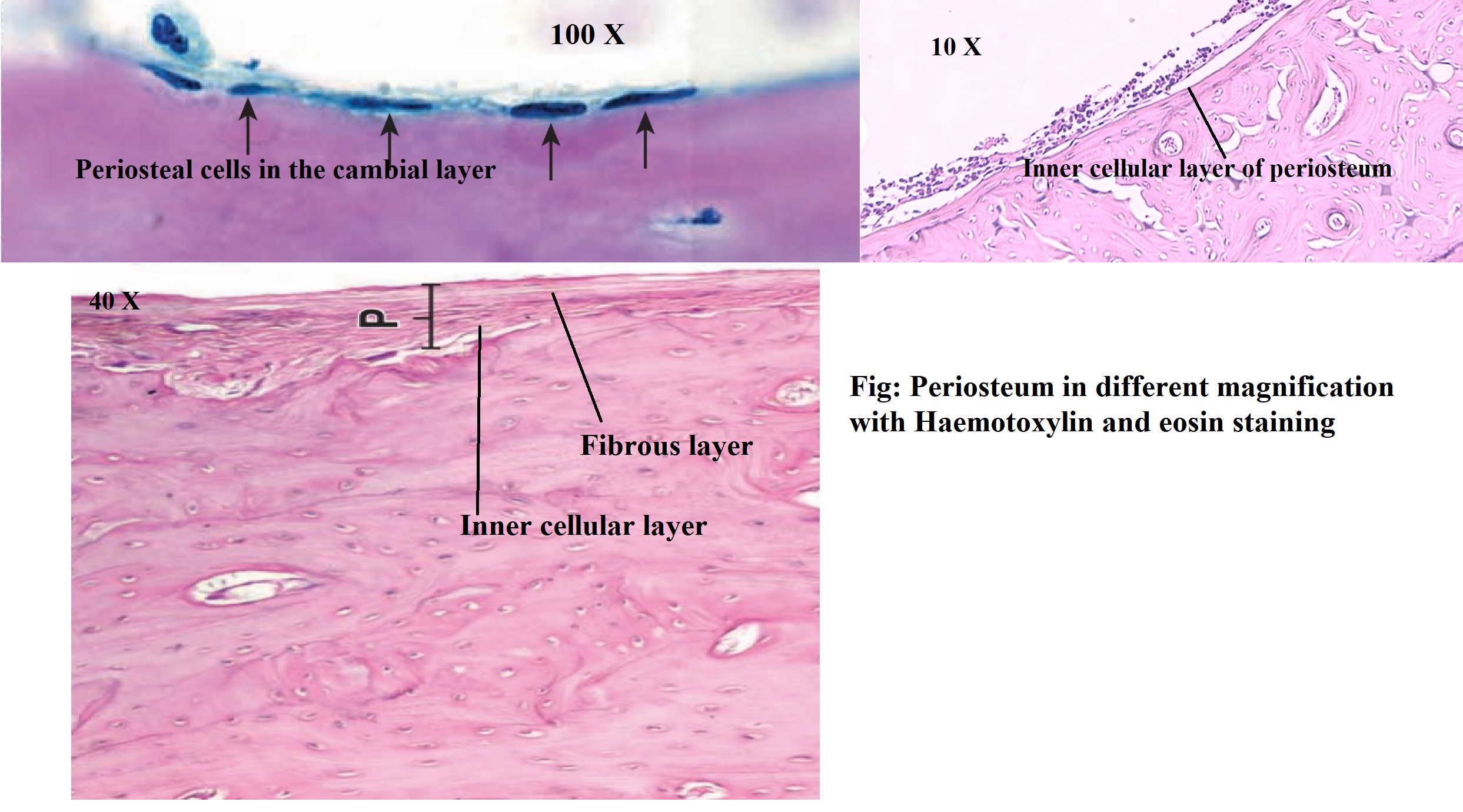
Dwek JR. The periosteum: what is it, where is it, and what mimics it in its absence? Skeletal radiology. 2010 Apr:39(4):319-23. doi: 10.1007/s00256-009-0849-9. Epub
[PubMed PMID: 20049593]
[15]
Squier CA, Ghoneim S, Kremenak CR. Ultrastructure of the periosteum from membrane bone. Journal of anatomy. 1990 Aug:171():233-9
[PubMed PMID: 2081707]
[16]
Allen MR, Hock JM, Burr DB. Periosteum: biology, regulation, and response to osteoporosis therapies. Bone. 2004 Nov:35(5):1003-12
[PubMed PMID: 15542024]
[17]
de Souza LE, Malta TM, Kashima Haddad S, Covas DT. Mesenchymal Stem Cells and Pericytes: To What Extent Are They Related? Stem cells and development. 2016 Dec 15:25(24):1843-1852
[PubMed PMID: 27702398]
[18]
Boskey AL, Posner AS. Bone structure, composition, and mineralization. The Orthopedic clinics of North America. 1984 Oct:15(4):597-612
[PubMed PMID: 6387574]
[19]
Diaz-Flores L, Gutierrez R, Lopez-Alonso A, Gonzalez R, Varela H. Pericytes as a supplementary source of osteoblasts in periosteal osteogenesis. Clinical orthopaedics and related research. 1992 Feb:(275):280-6
[PubMed PMID: 1735226]
[20]
Uddströmer L. The osteogenic capacity of tubular and membranous bone periosteum. A qualitative and quantitative experimental study in growing rabbits. Scandinavian journal of plastic and reconstructive surgery. 1978:12(3):195-205
[PubMed PMID: 368969]
[21]
Bland YS, Ashhurst DE. Fetal and postnatal development of the patella, patellar tendon and suprapatella in the rabbit; changes in the distribution of the fibrillar collagens. Journal of anatomy. 1997 Apr:190 ( Pt 3)(Pt 3):327-42
[PubMed PMID: 9147220]
[22]
Aper RL, Saltzman CL, Brown TD. The effect of hallux sesamoid excision on the flexor hallucis longus moment arm. Clinical orthopaedics and related research. 1996 Apr:(325):209-17
[PubMed PMID: 8998878]
[23]
Sims NA, Vrahnas C. Regulation of cortical and trabecular bone mass by communication between osteoblasts, osteocytes and osteoclasts. Archives of biochemistry and biophysics. 2014 Nov 1:561():22-8. doi: 10.1016/j.abb.2014.05.015. Epub 2014 May 26
[PubMed PMID: 24875146]
[24]
Christodoulou C, Spencer JA, Yeh SA, Turcotte R, Kokkaliaris KD, Panero R, Ramos A, Guo G, Seyedhassantehrani N, Esipova TV, Vinogradov SA, Rudzinskas S, Zhang Y, Perkins AS, Orkin SH, Calogero RA, Schroeder T, Lin CP, Camargo FD. Live-animal imaging of native haematopoietic stem and progenitor cells. Nature. 2020 Feb:578(7794):278-283. doi: 10.1038/s41586-020-1971-z. Epub 2020 Feb 5
[PubMed PMID: 32025033]
[25]
Hage IS, Hamade RF. Intracortical stiffness of mid-diaphysis femur bovine bone: lacunar-canalicular based homogenization numerical solutions and microhardness measurements. Journal of materials science. Materials in medicine. 2017 Sep:28(9):135. doi: 10.1007/s10856-017-5924-5. Epub 2017 Jul 31
[PubMed PMID: 28762142]
[26]
Lu X, Jerban S, Wan L, Ma Y, Jang H, Le N, Yang W, Chang EY, Du J. Three-dimensional ultrashort echo time imaging with tricomponent analysis for human cortical bone. Magnetic resonance in medicine. 2019 Jul:82(1):348-355. doi: 10.1002/mrm.27718. Epub 2019 Mar 7
[PubMed PMID: 30847989]
[27]
He X, Bougioukli S, Ortega B, Arevalo E, Lieberman JR, McMahon AP. Sox9 positive periosteal cells in fracture repair of the adult mammalian long bone. Bone. 2017 Oct:103():12-19. doi: 10.1016/j.bone.2017.06.008. Epub 2017 Jun 13
[PubMed PMID: 28627474]
[28]
Ren L, Yang P, Wang Z, Zhang J, Ding C, Shang P. Biomechanical and biophysical environment of bone from the macroscopic to the pericellular and molecular level. Journal of the mechanical behavior of biomedical materials. 2015 Oct:50():104-22. doi: 10.1016/j.jmbbm.2015.04.021. Epub 2015 Apr 24
[PubMed PMID: 26119589]
[29]
Zhou X, von der Mark K, Henry S, Norton W, Adams H, de Crombrugghe B. Chondrocytes transdifferentiate into osteoblasts in endochondral bone during development, postnatal growth and fracture healing in mice. PLoS genetics. 2014 Dec:10(12):e1004820. doi: 10.1371/journal.pgen.1004820. Epub 2014 Dec 4
[PubMed PMID: 25474590]
[30]
Szabó A, Janovszky Á, Pócs L, Boros M. The periosteal microcirculation in health and disease: An update on clinical significance. Microvascular research. 2017 Mar:110():5-13. doi: 10.1016/j.mvr.2016.11.005. Epub 2016 Nov 23
[PubMed PMID: 27889558]
[31]
Buckwalter JA, Glimcher MJ, Cooper RR, Recker R. Bone biology. I: Structure, blood supply, cells, matrix, and mineralization. Instructional course lectures. 1996:45():371-86
[PubMed PMID: 8727757]
[32]
Datta HK, Ng WF, Walker JA, Tuck SP, Varanasi SS. The cell biology of bone metabolism. Journal of clinical pathology. 2008 May:61(5):577-87. doi: 10.1136/jcp.2007.048868. Epub
[PubMed PMID: 18441154]
[33]
Grover K, Lin L, Hu M, Muir J, Qin YX. Spatial distribution and remodeling of elastic modulus of bone in micro-regime as prediction of early stage osteoporosis. Journal of biomechanics. 2016 Jan 25:49(2):161-6. doi: 10.1016/j.jbiomech.2015.11.052. Epub 2015 Dec 3
[PubMed PMID: 26705110]
Level 2 (mid-level) evidence
[34]
Choudry UH, Bakri K, Moran SL, Karacor Z, Shin AY. The vascularized medial femoral condyle periosteal bone flap for the treatment of recalcitrant bony nonunions. Annals of plastic surgery. 2008 Feb:60(2):174-80. doi: 10.1097/SAP.0b013e318056d6b5. Epub
[PubMed PMID: 18216511]
[35]
Gorter EA, Gerretsen BM, Krijnen P, Appelman-Dijkstra NM, Schipper IB. Does osteoporosis affect the healing of subcapital humerus and distal radius fractures? Journal of orthopaedics. 2020 Nov-Dec:22():237-241. doi: 10.1016/j.jor.2020.05.004. Epub 2020 May 6
[PubMed PMID: 32425424]
[36]
Szelerski Ł, Żarek S, Górski R, Mochocki K, Górski R, Morasiewicz P, Małdyk P. Surgical treatment outcomes of the Ilizarov and internal osteosynthesis methods in posttraumatic pseudarthrosis of the tibia-a retrospective comparative analysis. Journal of orthopaedic surgery and research. 2020 May 19:15(1):179. doi: 10.1186/s13018-020-01697-4. Epub 2020 May 19
[PubMed PMID: 32430044]
[37]
Langdahl B, Ferrari S, Dempster DW. Bone modeling and remodeling: potential as therapeutic targets for the treatment of osteoporosis. Therapeutic advances in musculoskeletal disease. 2016 Dec:8(6):225-235. doi: 10.1177/1759720X16670154. Epub 2016 Oct 5
[PubMed PMID: 28255336]
[38]
Manolagas SC. Birth and death of bone cells: basic regulatory mechanisms and implications for the pathogenesis and treatment of osteoporosis. Endocrine reviews. 2000 Apr:21(2):115-37
[PubMed PMID: 10782361]
[39]
Eriksen EF. Normal and pathological remodeling of human trabecular bone: three dimensional reconstruction of the remodeling sequence in normals and in metabolic bone disease. Endocrine reviews. 1986 Nov:7(4):379-408
[PubMed PMID: 3536460]
[40]
Clark J, Stechschulte DJ Jr. The interface between bone and tendon at an insertion site: a study of the quadriceps tendon insertion. Journal of anatomy. 1998 May:192 ( Pt 4)(Pt 4):605-16
[PubMed PMID: 9723987]
[41]
Tabuchi K, Soejima T, Kanazawa T, Noguchi K, Nagata K. Chronological changes in the collagen-type composition at tendon-bone interface in rabbits. Bone & joint research. 2012 Sep:1(9):218-24. doi: 10.1302/2046-3758.19.2000109. Epub 2012 Sep 1
[PubMed PMID: 23610694]
[42]
Strocchi R, Raspanti M, Ruggeri A, Franchi M, De Pasquale V, Stringa L, Ruggeri A. Intertwined Sharpey fibers in human acellular cementum. Italian journal of anatomy and embryology = Archivio italiano di anatomia ed embriologia. 1999 Oct-Dec:104(4):175-83
[PubMed PMID: 10684181]
[43]
Daley ELH, Kuttig J, Stegemann JP. Development of Modular, Dual-Perfused Osteochondral Constructs for Cartilage Repair. Tissue engineering. Part C, Methods. 2019 Mar:25(3):127-136. doi: 10.1089/ten.TEC.2018.0356. Epub
[PubMed PMID: 30724134]
[44]
Cheng ZL, Cai M, Chen XY, Li P, Chen XH, Lin ZM, Xu M. A novel cutting machine supports dental students to study the histology of the tooth hard tissue. Journal of dental sciences. 2019 Jun:14(2):113-118. doi: 10.1016/j.jds.2019.03.012. Epub 2019 May 15
[PubMed PMID: 31210885]
[45]
Goldschlager T, Abdelkader A, Kerr J, Boundy I, Jenkin G. Undecalcified bone preparation for histology, histomorphometry and fluorochrome analysis. Journal of visualized experiments : JoVE. 2010 Jan 8:(35):. pii: 1707. doi: 10.3791/1707. Epub 2010 Jan 8
[PubMed PMID: 20062000]
[46]
Mohsin S, O' Brien FJ, Lee TC. New embedding medium for sectioning undecalcified bone. Biotechnic & histochemistry : official publication of the Biological Stain Commission. 2006 Mar-Jun:81(2-3):99-103
[PubMed PMID: 16908434]
[47]
Yang R, Davies CM, Archer CW, Richards RG. Immunohistochemistry of matrix markers in Technovit 9100 New-embedded undecalcified bone sections. European cells & materials. 2003 Dec 31:6():57-71; discussion 71
[PubMed PMID: 14722903]
[48]
Cano-Sánchez J, Campo-Trapero J, Gonzalo-Lafuente JC, Moreno-López LA, Bascones-Martínez A. Undecalcified bone samples: a description of the technique and its utility based on the literature. Medicina oral, patologia oral y cirugia bucal. 2005 Apr 1:10 Suppl 1():E74-87
[PubMed PMID: 15800470]
[49]
Kiani MT, Takzare N, Khoshzaban A, Jalilianfar E, Aghajanpour L, Tabrizi R. Histological Changes in the Periosteum Following Subperiosteal Expansion in Rabbit Scalp. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2018 Apr:76(4):900-904. doi: 10.1016/j.joms.2017.08.020. Epub 2017 Aug 31
[PubMed PMID: 28911959]
[50]
McClellan P, Jacquet R, Yu Q, Landis WJ. A Method for the Immunohistochemical Identification and Localization of Osterix in Periosteum-Wrapped Constructs for Tissue Engineering of Bone. The journal of histochemistry and cytochemistry : official journal of the Histochemistry Society. 2017 Jul:65(7):407-420. doi: 10.1369/0022155417705300. Epub 2017 Apr 17
[PubMed PMID: 28415912]
[51]
Frey SP, Jansen H, Doht S, Filgueira L, Zellweger R. Immunohistochemical and molecular characterization of the human periosteum. TheScientificWorldJournal. 2013:2013():341078. doi: 10.1155/2013/341078. Epub 2013 May 2
[PubMed PMID: 23737713]
[52]
Melhus G, Solberg LB, Dimmen S, Madsen JE, Nordsletten L, Reinholt FP. Experimental osteoporosis induced by ovariectomy and vitamin D deficiency does not markedly affect fracture healing in rats. Acta orthopaedica. 2007 Jun:78(3):393-403
[PubMed PMID: 17611855]
[53]
Hultenby K, Reinholt FP, Oldberg A, Heinegård D. Ultrastructural immunolocalization of osteopontin in metaphyseal and cortical bone. Matrix (Stuttgart, Germany). 1991 Jun:11(3):206-13
[PubMed PMID: 1870452]
[54]
Li M, Amizuka N, Oda K, Tokunaga K, Ito T, Takeuchi K, Takagi R, Maeda T. Histochemical evidence of the initial chondrogenesis and osteogenesis in the periosteum of a rib fractured model: implications of osteocyte involvement in periosteal chondrogenesis. Microscopy research and technique. 2004 Jul 1:64(4):330-42
[PubMed PMID: 15481050]
[55]
Long PH, Tarpley JE, Rowland GN, Lee SR, Britton WM. A simple procedure for preparing and staining undecalcified sections of avian growth plate and metaphysis. Avian diseases. 1984 Jan-Mar:28(1):285-8
[PubMed PMID: 6372780]
[57]
Rentsch C, Schneiders W, Manthey S, Rentsch B, Rammelt S. Comprehensive histological evaluation of bone implants. Biomatter. 2014:4():. doi: 10.4161/biom.27993. Epub 2014 Feb 6
[PubMed PMID: 24504113]
[58]
Gruber HE. Adaptations of Goldner's Masson trichrome stain for the study of undecalcified plastic embedded bone. Biotechnic & histochemistry : official publication of the Biological Stain Commission. 1992 Jan:67(1):30-4
[PubMed PMID: 1617000]
[59]
SANO ME. Trichrome stain for tissue section, culture or smear. American journal of clinical pathology. 1949 Sep:19(9):898
[PubMed PMID: 18137790]
[60]
Filgueira L. Fluorescence-based staining for tartrate-resistant acidic phosphatase (TRAP) in osteoclasts combined with other fluorescent dyes and protocols. The journal of histochemistry and cytochemistry : official journal of the Histochemistry Society. 2004 Mar:52(3):411-4
[PubMed PMID: 14966208]
[61]
Meagher J, Zellweger R, Filgueira L. Functional dissociation of the basolateral transcytotic compartment from the apical phago-lysosomal compartment in human osteoclasts. The journal of histochemistry and cytochemistry : official journal of the Histochemistry Society. 2005 May:53(5):665-70
[PubMed PMID: 15872059]
[62]
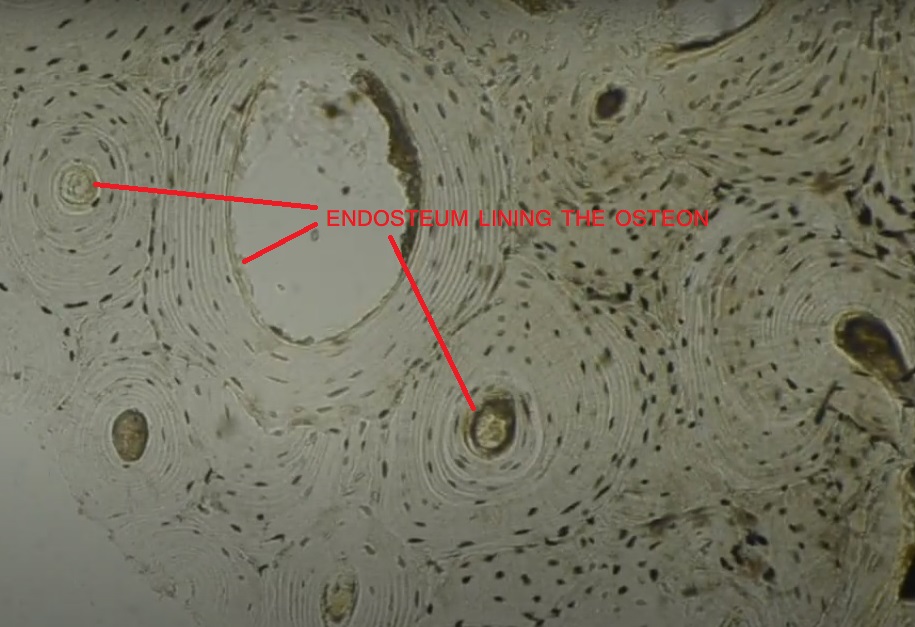
Miller SC, Bowman BM, Smith JM, Jee WS. Characterization of endosteal bone-lining cells from fatty marrow bone sites in adult beagles. The Anatomical record. 1980 Oct:198(2):163-73
[PubMed PMID: 7212302]
[63]
Bisseret D,Kaci R,Lafage-Proust MH,Alison M,Parlier-Cuau C,Laredo JD,Bousson V, Periosteum: characteristic imaging findings with emphasis on radiologic-pathologic comparisons. Skeletal radiology. 2015 Mar;
[PubMed PMID: 25269751]
[64]
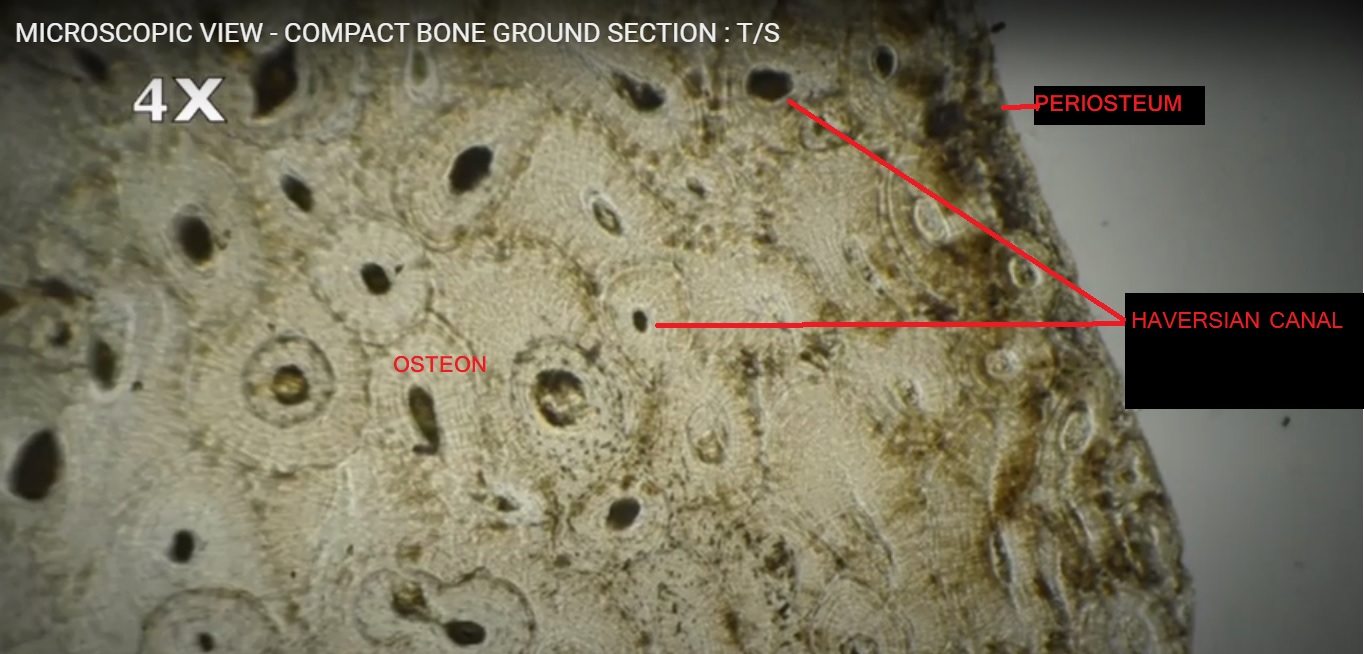
Kim JN, Lee JY, Shin KJ, Gil YC, Koh KS, Song WC. Haversian system of compact bone and comparison between endosteal and periosteal sides using three-dimensional reconstruction in rat. Anatomy & cell biology. 2015 Dec:48(4):258-61. doi: 10.5115/acb.2015.48.4.258. Epub 2015 Dec 21
[PubMed PMID: 26770876]
[65]
Simon TM, Van Sickle DC, Kunishima DH, Jackson DW. Cambium cell stimulation from surgical release of the periosteum. Journal of orthopaedic research : official publication of the Orthopaedic Research Society. 2003 May:21(3):470-80
[PubMed PMID: 12706020]
[66]
Yu PK, Balaratnasingam C, Cringle SJ, McAllister IL, Provis J, Yu DY. Microstructure and network organization of the microvasculature in the human macula. Investigative ophthalmology & visual science. 2010 Dec:51(12):6735-43. doi: 10.1167/iovs.10-5415. Epub 2010 Aug 4
[PubMed PMID: 20688746]
[67]
Crocker DJ, Murad TM, Geer JC. Role of the pericyte in wound healing. An ultrastructural study. Experimental and molecular pathology. 1970 Aug:13(1):51-65
[PubMed PMID: 5459855]
[68]
Díaz-Flores L, Gutiérrez R, Madrid JF, Varela H, Valladares F, Acosta E, Martín-Vasallo P, Díaz-Flores L Jr. Pericytes. Morphofunction, interactions and pathology in a quiescent and activated mesenchymal cell niche. Histology and histopathology. 2009 Jul:24(7):909-69. doi: 10.14670/HH-24.909. Epub
[PubMed PMID: 19475537]
[69]
Tonna EA, Cronkite EP. The periosteum. Autoradiographic studies on cellular proliferation and transformation utilizing tritiated thymidine. Clinical orthopaedics and related research. 1963:30():218-33
[PubMed PMID: 4172521]
[70]
Roberto-Rodrigues M, Fernandes RM, Senos R, Scoralick AC, Bastos AL, Santos TM, Viana LP, Lima I, Guzman-Silva MA, Kfoury-Júnior JR. Novel rat model of nonunion fracture with vascular deficit. Injury. 2015 Apr:46(4):649-54. doi: 10.1016/j.injury.2015.01.033. Epub 2015 Jan 23
[PubMed PMID: 25661107]
[71]
Hirashima S, Ohta K, Kanazawa T, Uemura K, Togo A, Yoshitomi M, Okayama S, Kusukawa J, Nakamura K. Anchoring structure of the calvarial periosteum revealed by focused ion beam/scanning electron microscope tomography. Scientific reports. 2015 Dec 2:5():17511. doi: 10.1038/srep17511. Epub 2015 Dec 2
[PubMed PMID: 26627533]
[72]
Danalache M, Kliesch SM, Munz M, Naros A, Reinert S, Alexander D. Quality Analysis of Minerals Formed by Jaw Periosteal Cells under Different Culture Conditions. International journal of molecular sciences. 2019 Aug 27:20(17):. doi: 10.3390/ijms20174193. Epub 2019 Aug 27
[PubMed PMID: 31461878]
[73]
Liu C, Cabahug-Zuckerman P, Stubbs C, Pendola M, Cai C, Mann KA, Castillo AB. Mechanical Loading Promotes the Expansion of Primitive Osteoprogenitors and Organizes Matrix and Vascular Morphology in Long Bone Defects. Journal of bone and mineral research : the official journal of the American Society for Bone and Mineral Research. 2019 May:34(5):896-910. doi: 10.1002/jbmr.3668. Epub 2019 Feb 20
[PubMed PMID: 30645780]
[74]
Boyde A, Hordell MH. Scanning electron microscopy of lamellar bone. Zeitschrift fur Zellforschung und mikroskopische Anatomie (Vienna, Austria : 1948). 1969:93(2):213-31
[PubMed PMID: 4905350]
[75]
He X, Cheng R, Benyajati S, Ma JX. PEDF and its roles in physiological and pathological conditions: implication in diabetic and hypoxia-induced angiogenic diseases. Clinical science (London, England : 1979). 2015 Jun:128(11):805-23. doi: 10.1042/CS20130463. Epub
[PubMed PMID: 25881671]
[76]
Famulla S, Lamers D, Hartwig S, Passlack W, Horrighs A, Cramer A, Lehr S, Sell H, Eckel J. Pigment epithelium-derived factor (PEDF) is one of the most abundant proteins secreted by human adipocytes and induces insulin resistance and inflammatory signaling in muscle and fat cells. International journal of obesity (2005). 2011 Jun:35(6):762-72. doi: 10.1038/ijo.2010.212. Epub 2010 Oct 12
[PubMed PMID: 20938440]
[77]
Beck C, Girschick HJ, Morbach H, Schwarz T, Yimam T, Frenkel J, van Gijn ME. Mutation screening of the IL-1 receptor antagonist gene in chronic non-bacterial osteomyelitis of childhood and adolescence. Clinical and experimental rheumatology. 2011 Nov-Dec:29(6):1040-3
[PubMed PMID: 22032624]
[78]
Schnellbacher C, Ciocca G, Menendez R, Aksentijevich I, Goldbach-Mansky R, Duarte AM, Rivas-Chacon R. Deficiency of interleukin-1 receptor antagonist responsive to anakinra. Pediatric dermatology. 2013 Nov-Dec:30(6):758-60. doi: 10.1111/j.1525-1470.2012.01725.x. Epub 2012 Apr 4
[PubMed PMID: 22471702]
[79]
Van Wesenbeeck L, Cleiren E, Gram J, Beals RK, Bénichou O, Scopelliti D, Key L, Renton T, Bartels C, Gong Y, Warman ML, De Vernejoul MC, Bollerslev J, Van Hul W. Six novel missense mutations in the LDL receptor-related protein 5 (LRP5) gene in different conditions with an increased bone density. American journal of human genetics. 2003 Mar:72(3):763-71
[PubMed PMID: 12579474]
[80]
O'Driscoll SW. Articular cartilage regeneration using periosteum. Clinical orthopaedics and related research. 1999 Oct:(367 Suppl):S186-203
[PubMed PMID: 10546647]
[81]
Chen D, Shen H, Shao J, Jiang Y, Lu J, He Y, Huang C. Superior mineralization and neovascularization capacity of adult human metaphyseal periosteum-derived cells for skeletal tissue engineering applications. International journal of molecular medicine. 2011 May:27(5):707-13. doi: 10.3892/ijmm.2011.634. Epub 2011 Mar 2
[PubMed PMID: 21369695]
[82]
Gamie Z, Tran GT, Vyzas G, Korres N, Heliotis M, Mantalaris A, Tsiridis E. Stem cells combined with bone graft substitutes in skeletal tissue engineering. Expert opinion on biological therapy. 2012 Jun:12(6):713-29. doi: 10.1517/14712598.2012.679652. Epub 2012 Apr 14
[PubMed PMID: 22500826]
[83]
Burnei G, Vlad C, Gavriliu S, Georgescu I, Hodorogea D, Pârvan A, Burnei C, El Nayef T, Drăghici I. Upper and lower limb length equalization: diagnosis, limb lengthening and curtailment, epiphysiodesis. Romanian journal of internal medicine = Revue roumaine de medecine interne. 2012 Jan-Mar:50(1):43-59
[PubMed PMID: 22788093]
[84]
Limpaphayom N, Prasongchin P. Surgical technique: Lower limb-length equalization by periosteal stripping and periosteal division. Clinical orthopaedics and related research. 2011 Nov:469(11):3181-9. doi: 10.1007/s11999-011-2013-9. Epub 2011 Aug 10
[PubMed PMID: 21830168]
[85]
Edwards DJ, Bickerstaff DB, Bell MJ. Periosteal stripping in achondroplastic children. Little effect on limb length in 10 cases. Acta orthopaedica Scandinavica. 1994 Jun:65(3):333-4
[PubMed PMID: 8042489]
[86]
Wei H, Li S, Wei R, Chen Y. [Free fibula flap and computed tomographic angiography in the functional reconstruction of oral and maxillofacial hard and soft tissue defects]. Lin chuang er bi yan hou tou jing wai ke za zhi = Journal of clinical otorhinolaryngology, head, and neck surgery. 2014 Aug:28(16):1248-50
[PubMed PMID: 25464569]
[87]
Abed PF, El Chaar E, Boltchi F, Bassir SH. The Novel Periosteal Flap Stretch Technique: A Predictable Method to Achieve and maintain Primary Closure in Augmentative Procedures. Journal of the International Academy of Periodontology. 2020 Jan 1:22(1):11-20
[PubMed PMID: 31896103]
[88]
Feingold KR, Anawalt B, Blackman MR, Boyce A, Chrousos G, Corpas E, de Herder WW, Dhatariya K, Dungan K, Hofland J, Kalra S, Kaltsas G, Kapoor N, Koch C, Kopp P, Korbonits M, Kovacs CS, Kuohung W, Laferrère B, Levy M, McGee EA, McLachlan R, New M, Purnell J, Sahay R, Shah AS, Singer F, Sperling MA, Stratakis CA, Trence DL, Wilson DP, Singer FR. Paget’s Disease of Bone. Endotext. 2000:():
[PubMed PMID: 25905262]