Introduction
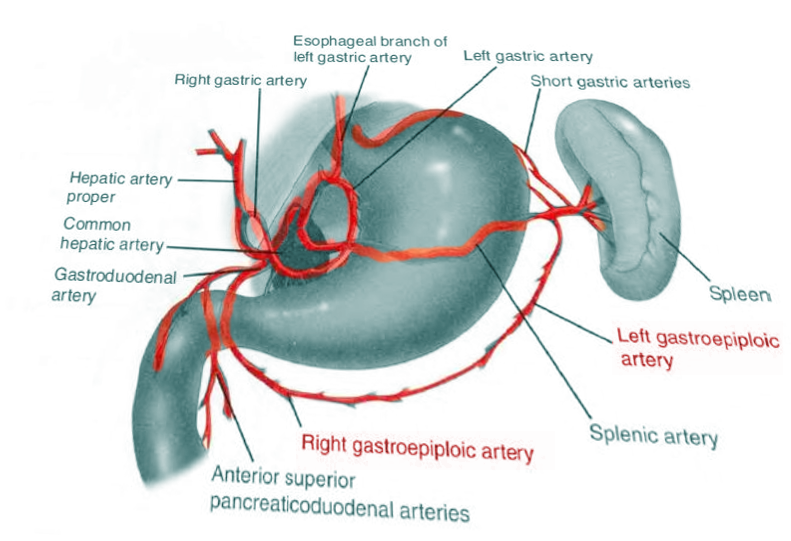
The gastroepiploic artery (GEA) is made up of two arteries which supply the greater omentum and the stomach (see Image. Gastroepipolic Artery). The right gastroepiploic artery (RGEA) is also referred to as the right gastro-omental artery or arteria gastroepiploic dextra in older texts. The RGEA is one of the distal vessels branching off the gastroduodenal artery. The vessel courses along the great curvature of the stomach in a right-to-left direction. It travels between layers of greater omentum giving off gastric and omental branches and can create an anastomosis with the left gastroepiploic artery. The left gastroepiploic artery (LGEA) is also known to as the left gastro-omental artery or arteria gastroepiploic sinistra in older texts. The LGEA is usually smaller in diameter than the RGEA, and commonly branches from the splenic artery near the tail of the pancreas. It courses medially along the greater curvature of the stomach towards the RGEA, giving off gastric and omental branches.
Structure and Function
The RGEA supplies blood to the anterior and posterior antrum and lower body of the stomach. The RGEA also supplies inferior branches to the right greater omentum, which can sometimes branch and supply the final segments of the duodenum. The LGEA reaches the stomach about the midpoint of the greater curvature and supplies blood to the anterior and posterior body of the stomach. The LGEA also supplies the greater omentum along with anastomotic branches of the middle colic artery.[1]
Embryology
The formation of blood vessels initiates with the development of blood islands or islets of Wolff in the mesenchyme of the splanchnic mesoderm, before the yolk sac and later of the allantois. The intra-embryonic vessels originate from the blood islands, in front of the protocordal disk, where a horseshoe-shaped plexiform network forms that surrounds the cephalic portion of the embryo. At the same time two groups of angioblastic cells, in a dorsal paramedian position, form two parallel vessels, the dorsal aortas, which cephalically connect to the plexiform network. The further development of the vascular system consists of the formation of ducts of greater caliber from the primitive plexiform network. The most voluminous of these are the right and left primitive aorta, from which the fetal arterial tree originates which develops parallel to the cardiac tube and its subsequent evolution.
The formation of anastomoses between the intra- and extra-embryonic vessels complete the circulatory system.
The vasculature that supplies the gastrointestinal system originates from the anterior ventral segmental arteries of the primitive aorta between two layers of dorsal mesogastrium. The tenth segmental artery is the source of the foregut artery (celiac artery). This artery supplies blood to all foregut structures, migrates caudally and rotates in concert with the stomach during embryonic development. The celiac artery gives rise to both the hepatic artery and the splenic artery. The hepatic artery further branches into the gastroduodenal artery, giving rise to the RGEA. The splenic artery then gives rise to the LGEA. The RGEA and LGEA, along with other local structures elongate with the development of the greater curvature of the stomach and lesser sac.
Blood Supply and Lymphatics
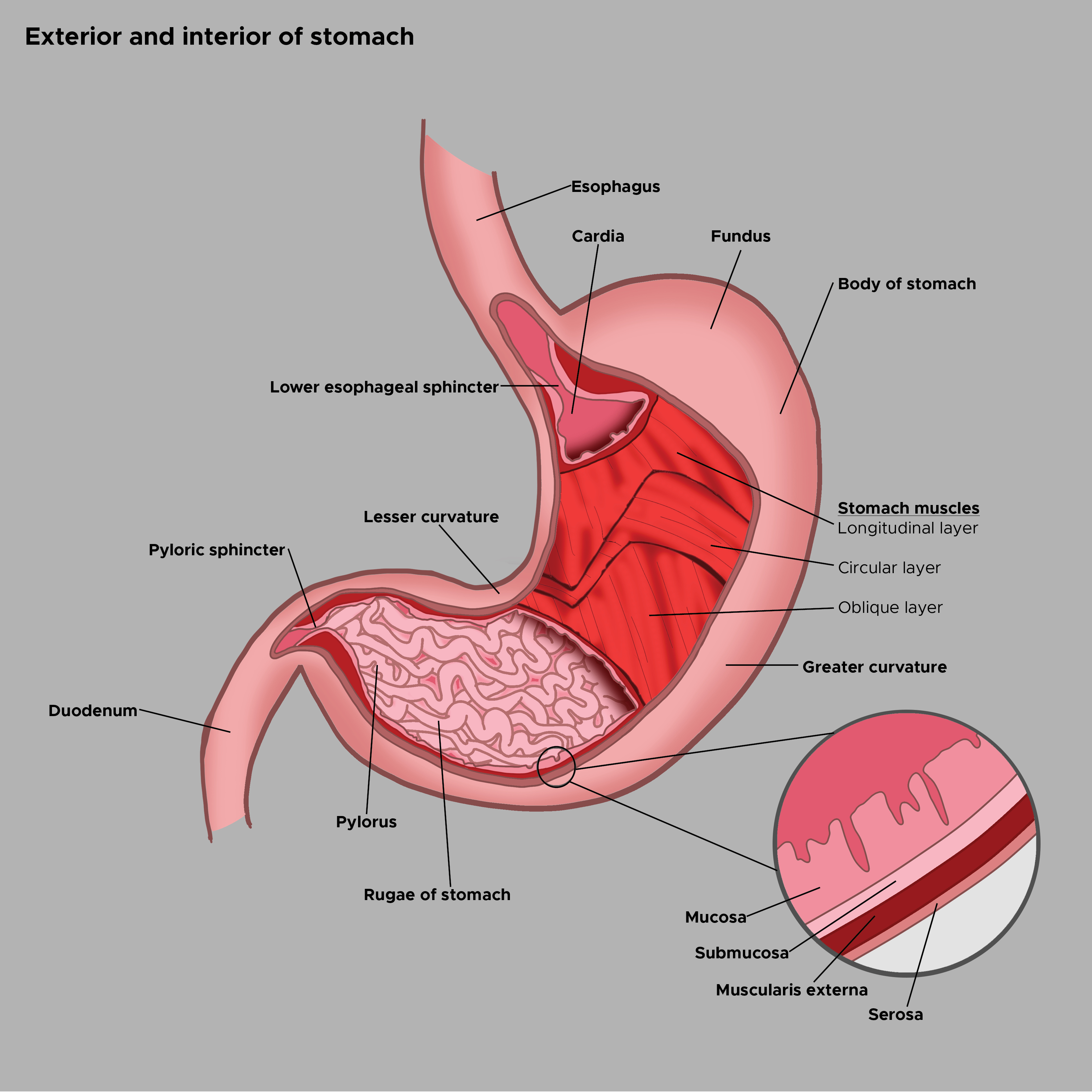
The origin of the RGEA is usually posterior to the first part of the duodenum, arising from the gastroduodenal artery. Its course varies, but often, it parallels the gastroduodenal artery distally along the pylorus, turns medially and travels between the greater curvature of the stomach and the greater omentum (see Image. Exterior and Interior of the Stomach). After turning medially, the RGEA commonly lies about 2 centimeters below the stomach, sandwiched between layers of the gastrocolic omentum anteriorly and posteriorly. The artery gives off superior branches that supply the anterior and posterior gastric antrum and the distal body of the stomach. The RGEA also gives off inferior branches that supply the greater omentum, and a few of these branches can sometimes supply the final segments of the duodenum.[1]
The LGEA originates from the splenic artery (or as a branch with the inferior splenic artery) near the pancreatic tail. The artery originates slightly medial to, and then courses toward, the gastrosplenic ligament; it runs toward the stomach reaching the greater curvature at the level of the anterior pole of the spleen. It then turns and runs left-to-right and caudally about 2 centimeters below the stomach letting off superior gastric and posterior omental branches.[1] The LGEA can sometimes create an anastomosis with the RGEA. Through instrumental evaluations using computed tomographic angiography, we highlight the presence of lymphosomes and lymph nodes relative to the gastroepiploic artery.
Nerves
The gastroepiploic artery is innervated by the periarterial sympathetic nerve, which allows the artery to contract, stimulating the endothelial and smooth muscle. The contraction of the artery can be slow (if stimulated by alpha2-adrenoceptors) or faster (if stimulated by alpha1-adrenoceptors). The production of nitric oxide (NO) influences the presence of arterial tone modulation.
COnversely, C-type natriuretic peptide influences vasodilation. C-type natriuretic peptide relaxes the arterial tone through the activation of some channels, including large-conductance calcium-activated K+ channel and G-protein-gated inwardly-rectifying potassium channel.
Muscles
Smooth muscle cells contain alpha-smooth-actin (SMA), which allows the vessel to contract. We also find other proteins that influence the mobility of the vessel, such as collagen and elastin. Another type of actin is present, gamma-smooth-actin, but in smaller quantities.
Physiologic Variants
Evidence of anastomosis between the LGEA and the RGEA ranges from about 50 to 94%. One anatomical study, consisting of 17 cadavers, has shown that 94% of vessels anastomose with 70% of those being continuous (without a branching system connecting the two). Various other studies using angiograms have shown a 43 to 65% anastomosis rate, with 23 to 37% being continuous.[2]
The RGEA has been shown to have many different origins. The RGEA most commonly branches from the gastroduodenal artery but may branch off of the superior mesenteric artery when no gastroduodenal artery develops [3]. Anatomical studies have also shown the RGEA to receive equal-sized branches from both the celiac artery and the superior mesenteric artery.[4]
The LGEA often arises as a common branch with the inferior splenic artery and then branches into two separate arteries distally in its course. The omental branches of the LGEA have been shown to create anastomoses with branches of the middle colic artery.[1]
Surgical Considerations
The stomach depends largely on the RGEA and right gastric arteries for its blood supply; therefore, surgeons need to minimize iatrogenic damage that could compromise these vessels during surgery. However, it merits noting that there is plentiful collateral blood supply to the stomach. Thus damage to gastric vasculature creates more of a risk of bleeding than ischemia. Gastrointestinal ischemia stemming from a compromised GEA mainly occurs at gastric walls near the anastomoses between the RGEA and LGEA on the anterior and posterior greater curvature of the stomach. The LGEA is sometimes vulnerable during surgical mobilization of the colonic splenic flexure. The early RGEA is not easily accessible surgically because of its location posterior to the duodenum and is not as vulnerable in most surgeries.[1]
Clinical Significance
The RGEA and LGEA serve as notable landmarks when identifying anatomy inside the abdomen. The distal vessels are usually visible both laparoscopically and during open operations. The stomach can be located cephalad to these vessels and the omentum caudad. Penetrating traumatic injury can compromise the RGEA and LGEA, causing copious bleeding. Damage of this type would require prompt surgical intervention to control hemorrhage.
GEA aneurysms
One of the rarest types of aneurysms is a visceral artery aneurysm, and GEA aneurysms make up roughly 3.5% of all visceral artery aneurysms. The most frequent etiology is atherosclerotic disease. The aneurysm is typically asymptomatic; thus, diagnosis is commonly made only after rupture. If a non-ruptured lesion is incidentally found, the recommendation is to have an elective repair performed because the vessel has a high risk of complication and likelihood of future rupture.[5]
Esophagectomy
The RGEA and LGEA both donate blood flow to the stomach and therefore are useful in the creation of a gastric tube during an esophagectomy. Many physicians who perform this procedure choose to preserve the RGEA for blood supply when other vessels are ligated to mobilize the stomach. The RGEA can supply enough blood to serve as the main source of blood for a reconstructed stomach. One anatomic study measuring resins injected into the vasculature of 30 cadavers showed that the RGEA (and its branches) directly supplied 60% of the gastric tube post-esophagectomy. The LGEA and anastomotic branches supplied another 20% of the gastric tube.[6]
Cardiac Grafting/Physiology
The RGEA is an appropriate and dependable graft for coronary bypass surgery and has been shown to undergo less arteriosclerosis than other graft vessel candidates.[3] In some ways, it mirrors the functionality of the internal thoracic artery (ITA) for cardiac grafting. Research into the response of various neurotransmitters and their effect on the RGEA compared to the ITA has shown that both vessels contract in response to ergonovine, serotonin, phenylephrine, and norepinephrine.[7][8] Histamine has a paradoxical effect and differs in response regarding the two vessels, causing contraction of the ITA and dilatation of the RGEA.[9] Doppler mini-probe has shown an increase in RGEA blood flow following meals. This physiological response is thought to be due to the increased need for blood flow to the digestive tract following meals, by histamine.[10][11]
Other Issues
LGEA may have anatomical variations. For example, one study reported a very rare variation discovered by cadaver dissection. After its splenic origin, it could cross the pancreatic parenchyma in its posterior superficial portion; it exits posteriorly from the superior border of the pancreas, to finally branch into an omental branch, into a duplicated LGEA and another branch that ends in the main trunk of the left gastroepiploic artery.