Continuing Education Activity
The olecranon is the proximal articular portion of the ulna. Along with the coronoid process, it forms the greater sigmoid notch which articulates with the humerus to provide flexion and extension of the elbow. Fractures of the olecranon are a relatively common injury in adults; its subcutaneous location leaves it vulnerable to injury from a direct blow. Fractures sustained range from simple undisplaced fractures to complex open fracture dislocations. Olecranon fractures frequently require surgical management to restore articular congruity and elbow stability. This activity reviews the etiology, presentation, evaluation, and management of fractures of the olecranon and reviews the role of the interprofessional team in evaluating, diagnosing, and managing the condition.
Objectives:
- Describe the most common mechanisms of injury that can result in olecranon fractures.
- Summarize the diagnostic approach for an evaluation and assessment of a patient presenting with a potential olecranon fracture, including any indicated imaging studies.
- Outline the treatment options for olecranon fractures, depending on patient population and fracture severity grading.
- Review the role of improving coordination amongst the interprofessional team to streamline diagnosis, reduction, and/or surgery for patients with olecranon fracture.
Introduction
The olecranon is the proximal articular portion of the ulna. Along with the coronoid process, it forms the greater sigmoid (semilunar) notch which articulates with the humerus to provide flexion and extension of the elbow. Fractures of the olecranon are a relatively common injury in adults; its subcutaneous location leaves it vulnerable to injury from a direct blow. Fractures sustained range from simple nondisplaced fractures to complex open fracture dislocations. Olecranon fractures frequently require surgical management to restore articular congruity and elbow stability. Although outcomes after surgery are relatively good, it is not uncommon for patients to have a range of motion (ROM) deficit or require a repeat procedure to remove hardware.
Etiology
Most olecranon fractures occur in individuals aged 50 years or greater after a fall from standing height[1]. Younger individuals are likely to have injuries related to a higher energy injury mechanism[2]. Olecranon fractures can occur from forced elbow hyperextension or a direct blow to the elbow at 90 degrees of flexion. Avulsion injuries may also occur from an eccentric contraction of the triceps tendon[3]. These typically have a transverse or oblique fracture line and tend to be more common in osteoporotic patients.
Epidemiology
Olecranon fractures account for approximately 10% of upper extremity fractures[2]. The incidence is 12 per 10,000 [4]. The mean age of occurrence is 57, with males more likely to sustain an injury at a younger age. These injuries are frequently associated with concomitant elbow injuries, most frequently to the radial head and coronoid. Approximately 6.4% of injuries are open fractures[4].
Pathophysiology
Olecranon fractures typically involve the articular surface of the elbow. Posttraumatic arthritis occurs in approximately 20% of cases and persistent malreduction >2mm of the articular surface is associated with this outcome[1]. In fractures with significant comminution, inadvertent malreduction by narrowing the greater sigmoid notch may further predispose the patient to arthritis[5].
The triceps muscle (innervated by the radial n) inserts onto the olecranon, blending with the periosteum. A displaced fracture interrupts the extensor mechanism resulting in loss of active elbow extension. The pull from the triceps is the key deforming force, pulling the separated fragment superiorly. Greater displacement suggests tearing of the fibrous sheath over the olecranon.
The olecranon confers stability to the elbow joint, acting as a block to the anterior translation of the ulna in relation to the distal humerus. Olecranon fractures can have associated with ligamentous injury (the medial and lateral collateral ligaments stabilize against valgus and varus stress respectively), coronoid process, and radial head fractures. Unstable injuries require reduction and stable fixation of the olecranon to restore elbow stability.
The ulnar nerve lies on the medial aspect, posterior to the medial collateral ligament before crossing anteriorly to run alongside the ulnar artery. Awareness of these structures is key when operating in this region.
History and Physical
Patients typically present with elbow pain and swelling following a fall. If the fracture is displaced there may be marked deformity at the elbow with a palpable gap. The hallmark of an olecranon fracture is the inability to extend the elbow against gravity. The examiner must ensure that the patient is not using gravity to mimic active elbow extension. This is typically done by abducting the shoulder to 90 degrees, supporting the upper arm, and asking the patient to straighten their elbow from this position.
It is important to examine the entire involved extremity for associated injuries or lacerations suggestive of an open fracture.
Associated injuries of the coronoid process, radial head, or proximal radioulnar joint (Monteggia fracture) may be present and evaluated for on radiographs.
The examiner should palpate the elbow as well as the adjacent joints. A complete upper extremity neurovascular examination of the involved extremity should be conducted. The ulnar nerve is most at risk due to its superficial position on the medial aspect of the elbow. When the injury occurred secondary to a high-energy mechanism, the practitioner should be vigilant to avoid missing injuries that may be unrecognized by the patient due to the distracting nature of the olecranon fracture. It is prudent to question the patient about other sources of pain and examine all four extremities for crepitus, deformity, or pain with range of motion.
Evaluation
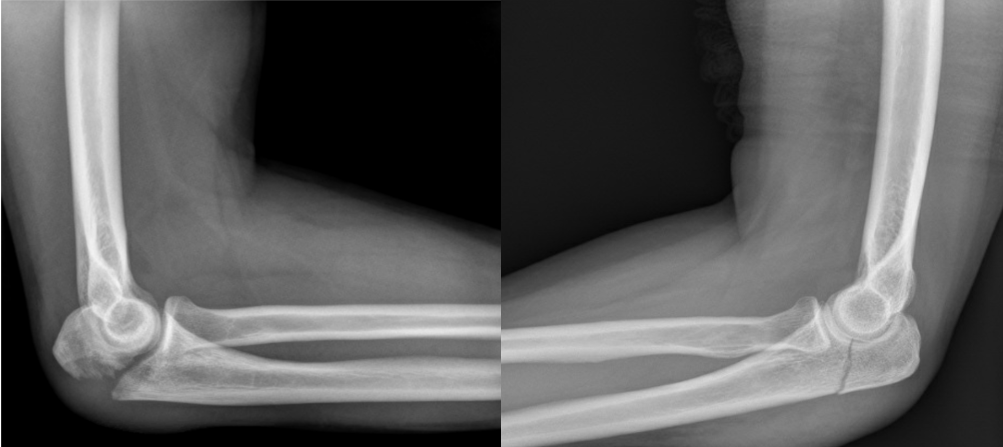
Initial evaluation with anteroposterior (AP) and lateral radiographs of the elbow are sufficient for most fractures to determine fracture pattern. A dedicated radiocapitellar view may also be performed to evaluate for radial head and capitellum fractures. Images should be examined for associated coronoid, radial head fracture or dislocation, and ulno-humeral congruity[2]. Computed tomography (CT) may be used in complex fracture patterns with associated injuries for pre-operative planning.
There are several classification systems of olecranon fractures. The most commonly used is the Mayo classification first described by Morrey in 1993. The goal of this system was to simplify the classification of olecranon fractures based on fracture comminution, displacement, and stability of the ulno-humeral joint. There are three types, each one further subdivided into type A and B, indicating non-comminuted and comminuted respectively[5]. Type I fractures are nondisplaced. Type II fractures are displaced at least 3mm, however, the ulno-humeral articulation is maintained indicating intact collateral ligaments. In type III injuries the fracture is displaced and the ulno-humeral joint is unstable. This injury is a fracture-dislocation, collateral ligaments may be incompetent causing instability[6]. The most common fracture pattern is Type II, which occurs in 80-85% of olecranon fractures. Type I injuries account for 5-12% of cases and approximately 6% are type III injuries[4][5].
Treatment / Management
Suspected olecranon fractures require orthopedic consultation. After a thorough history, physical exam, and imaging, the fracture should be immobilized in a posterior splint with slight extension. The reduction is indicated in type 3 injuries with the aim of reducing the remaining articular surface with the trochlea.
Nondisplaced olecranon fractures can be treated with an initial period of immobilization in a posterior slab long arm splint with the elbow in 45-90 degrees of flexion followed by early progressive active range of motion exercises with avoidance of active extension[2]. If treated non-operatively, patients should be monitored with serial radiographs to ensure adequate healing and that the fracture does not displace.
Type II and III injuries generally require surgical intervention. Non-operative management of type II injuries may be an option as there is [7] evidence that suggests that conservative management of displaced fractures in those over 70 years old can still lead to satisfactory function[8][9]. They may full elbow extension due to disruption of the extensor mechanism but in some patients, this is thought to be preferential to the risks of surgery. Risks and benefits of surgical versus non-surgical management should be fully discussed with the patient and treatment plan individualized for each patient based on medical comorbidities and overall function.
Displaced, stable, non-comminuted fractures (Mayo type 2A) may be amenable to tension band wiring (TBW). This construct converts the tension force from the pull of the triceps into a compressive force at the articular surface. It requires an intact dorsal cortex. Fractures treated with TBW should not have significant comminution, or they will cause collapse and narrowing of the distance between the coronoid and olecranon[5].
Plate and screw fixation is recommended for unstable fracture patterns with significant comminution or a fracture line exiting distal to the semilunar notch (Mayo Type 2B) and fracture-dislocations (Mayo Type 3)[1]. An oblique fracture line may be amenable to a lag screw and plate fixation. Plate options include one-third tubular plates, hook plates, limited contact dynamic compression plates, and frequently fracture-specific locked plates[2]. Care should be taken to obtain an anatomic reduction with direct visualization of the articular surface. There is a bare area on the articular surface of the olecranon which lacks articular cartilage. This should be reduced to maintain joint congruity[10]. The plate is typically placed on the dorsal aspect.
Intramedullary nails are now available and may be suitable for some fracture types. Intramedullary devices may avoid the wound complications related to the superficial location of traditional hardware used to treat olecranon fractures[1][2].
Excision and triceps advancement is an option in elderly, low-demand individuals where the fragment is too small for fixation or where less than 50% of the joint surface is involved. Cadaveric studies have shown that excising over 50% of the olecranon results in elbow instability, therefore this is the maximum recommended resection[11]. It is vital to ensure that the collateral ligaments, distal radioulnar joint, and intraosseous membrane are intact to prevent instability from occurring. It involves the removal of the fracture fragment and reattachment of the triceps muscle to the proximal ulna.
Differential Diagnosis
It is important to rule out other injuries about the elbow which may affect the treatment plan. The skin should be evaluated for open fractures. Other frequent associated injuries include coronoid fractures, radial head, and neck fractures, radial head dislocation, and collateral ligament injuries[12][4].
Prognosis
Patients usually have a good functional outcome after treatment of an olecranon fracture. Approximately 10-15 degrees loss of terminal extension may occur, although this is usually not clinically significant[10][13]. Long-term follow-up ranging 15-25 years reported good or excellent functional outcomes in 96% of patients [14]. Fractures have a high rate of healing with a nonunion rate of approximately 1% [15].
Complications
Hardware Irritation - Irritation leading to hardware removal is the most common complication due to the subcutaneous nature of the proximal olecranon. There is a variable rate of hardware removal for TBW and plate fixation in the literature. A recent prospective randomized control study reported a hardware removal rate of 50% with TBW and 22% with plate fixation[16]. Intramedullary devices are less prominent and have a lower risk of a secondary operation for hardware irritation[1]. Wire migration can occur in conjunction with wire breakage and fracture displacement.
Wound Complications/Infection - The subcutaneous nature of the olecranon provides little soft tissue coverage over hardware used for fixation. Placing plates on the side of the olecranon where there is a more robust soft tissue envelope may reduce the risk. Kirshner wires (k-wires) may back out and create wound problems or soft tissue irritation. Engaging the distal tip of the wire in the anterior cortex of the ulna[17]and turning the wires 180 degrees and burying them[18]can reduce the risk of the wires backing out. Injury to the anterior interosseus nerve and ulnar artery due to the penetration of the k-wire through the anterior cortex can be mitigated by placing wires at an angle of 20-30 degrees from the longitudinal axis of the ulna on the lateral view[19]. Pins that are too long can restrict supination by impinging on the radial neck or damaging the biceps tendon or supinator muscle. One series reported a higher rate of infection in patients treated with plate fixation compared to TBW (13% vs 0%)[16].
Loss of Motion - Patients commonly have a loss of terminal elbow extension of 10-15 degrees. This is usually not clinically significant as the functional elbow range of motion is a 30-130 degree arc of motion. One study reported a 39% incidence of a flexion contracture >10 degrees after plate fixation which did not significantly impact functional outcome scores[13]. General stiffness is thought to occur in up to 50% of patients but usually does not affect function.
Arthrosis - Degenerative changes can be seen on radiographs up to 50% percent of patients at long-term follow-up. This is not necessarily clinically significant as 96% of this cohort reported good or excellent outcomes. Narrowing of the distance between the tip of the olecranon and the coronoid may lead to malreduction and subsequent arthrosis[5].
Heterotopic ossification - This can occur in approximately 13% of patients
Ulnar Nerve Neuritis - This is an infrequent complication that occurs in approximately 2-12% of cases[1],[3]. The majority of cases will resolve with conservative management. Recalcitrant cases may require neurolysis and ulnar nerve transposition.
Nonunion - The risk of nonunion is approximately 1%[1]. Treatment options include conservative measures, internal fixation with or without bone graft, excision and triceps advancement, and elbow arthroplasty[15][20].
Malunion - This may be intra-articular or extra-articular. Interarticular malunion may occur from an inadequate reduction of a comminuted fracture, leading to narrowing of the sigmoid notch. Early arthritis will likely occur and may require an arthroplasty procedure. Extra-articular malunion presents with radial head subluxation and can be treated with an osteotomy[1].
Postoperative and Rehabilitation Care
Postoperative protocols vary by institution. Most physicians consider fracture stability, wound healing, and patient compliance when determining the duration of immobilization[3]. In general, a posterior removable splint or above elbow back-slab can be used postoperatively for 7-10 days with the elbow at ninety degrees of flexion and wrist in neutral. Immobilization is followed by a gravity-assisted range of motion exercises. Active range of motion and strengthening begin when radiographic evidence of healing is seen, approximately 6-8 weeks postoperatively[1]. One would expect to return to sporting activities or those that require full active movement of the elbow at 3-4 months.
Deterrence and Patient Education
It is critical to properly educate the patient regarding possible complications and treatment expectations of operative and non-operative management. Operative interventions carry general and specific risks with a high chance of needing a secondary procedure for hardware removal due to irritation. There is frequently a loss of terminal elbow extension of 10-15 degrees. Although this rarely results in a functional deficit, it may be of cosmetic concern and should be discussed with the patient prior to the procedure. Patient compliance with weight-bearing restrictions, a range of motion exercises, and strengthening is imperative for a good outcome.
Pearls and Other Issues
- Obtain adequate preoperative radiographs, especially a lateral view, to determine fracture morphology, comminution, and displacement.
- Fractures of the olecranon are intra-articular injuries and require anatomic reduction. Be careful to reduce the bare area of the articular surface.
- Do not malreduce the fracture and narrow the distance between the coronoid process and the tip of the olecranon.
- Nondisplaced fractures may be treated with a short period of immobilization followed by a range of motion. Close radiographic follow-up is necessary to monitor for displacement.
- The most common complication of TBW or plate fixation is hardware irritation. Inform the patient that they may need a second general anesthetic to remove the hardware.
Enhancing Healthcare Team Outcomes
Post-operative rehabilitation depends on regaining a functional range of motion and strength. Communication between the patient, physician, and therapist can improve patient adherence, satisfaction, and functional outcomes[21].