Continuing Education Activity
Corneal arcus are white or gray incomplete rings that form around the cornea. They are usually clinically insignificant but may be associated with an underlying disorder. This activity describes what they are, and what evaluation is needed. This activity also highlights and explains the role of the interprofessional team and management of corneal arcus in an attempt to improve patient care and outcomes.
Objectives:
- Identify corneal arcus on a physical exam.
- Outline when further evaluation is required for corneal arcus.
- Review a differential diagnosis for patients with corneal arcus.
- Describe an interprofessional approach in the management of corneal arcus.
Introduction
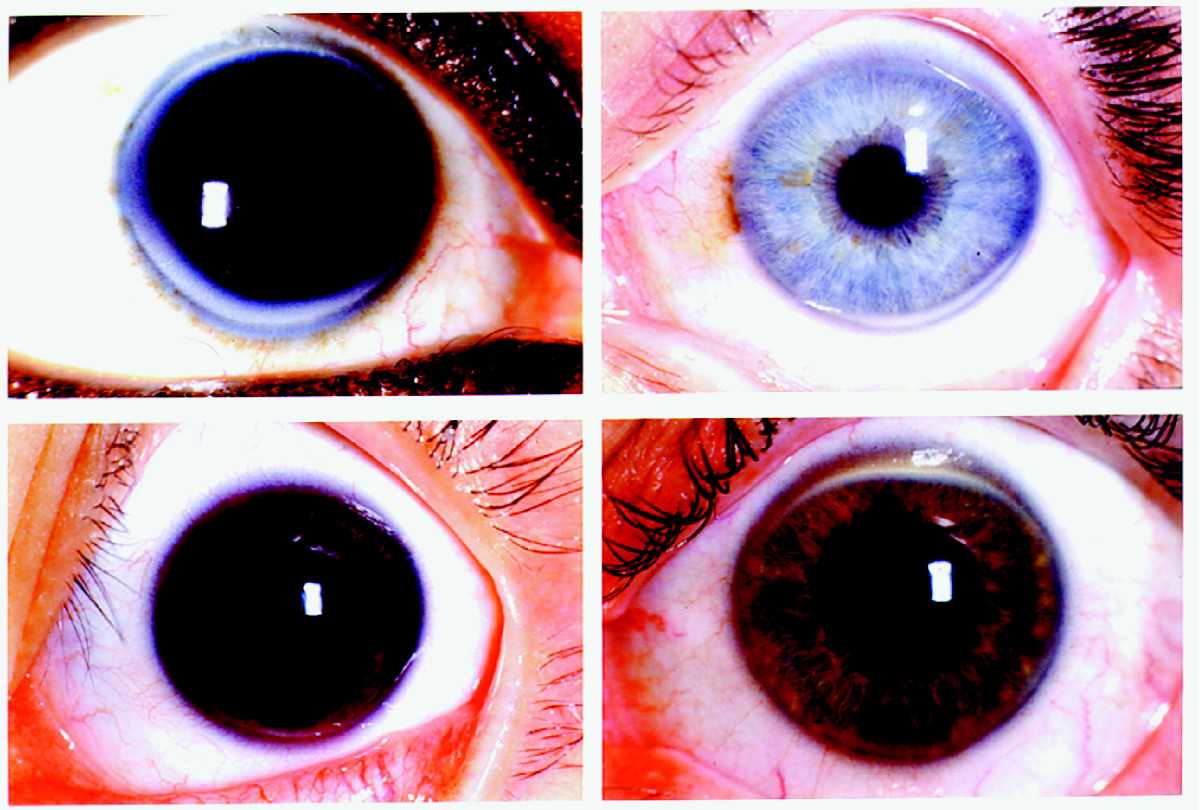
The eye is one of the most anatomically complex regions of the body, and often systemic diseases manifest in the eye, sometimes these ophthalmic manifestations predate other systemic manifestations. The cornea is the thin clear covering of the eye. Arcus senilis (cornea senilis) are lipid deposits that appear as rings on the outer region of the cornea. They are usually gray or white and are usually opaque. They often appear denser in the superior and inferior regions. They can grow with time, and can eventually form a ring around the entire cornea. The diagnosis of corneal arcus is made visually by examination with a biomicroscope (slit lamp). The diagnosis of corneal arcus can be confused with limbus sign (calcium deposits in the cornea).
Etiology
The formation of corneal arcus is dependent upon the vasculature of the limbus (the border between the cornea and the sclera). The arcus initially forms in the superior and inferior regions of the cornea, because these regions have greater perfusion than the central cornea. The regions that have greater perfusion also have capillaries that have greater permeability. Current theories suggest that lipids such as cholesterol, phospholipids, triglycerides, and lipoproteins are preferentially delivered to the more perfused regions of the cornea and the arcus form when the lipids and lipoproteins extend beyond the reach of the small vessels and thus get deposited in these peripheral regions.[1][2][3]
Epidemiology
The prevalence of corneal arcus varies with ethnicity. Individuals of African and Southeast Asian descent have a higher prevalence of arcus than those of white descent. Depending on the population studied, the prevalence of corneal arcus ranges from 20% to 35%; however, regardless of ethnic background, the incidence of corneal arcus increases with age. Some research has indicated that the prevalence of corneal arcus is nearly 100 percent in individuals over the age of 80. Traditionally men have had a higher incidence and prevalence of corneal arcus then women, and men, also have larger arcus. The presence of corneal arcus is usually clinically insignificant; however, the presence of corneal arcus is men under the age of 40 has been associated with a greater risk of cardiovascular disease. Historically it was thought that the presence of arcus was a predictor of cardiovascular disease regardless of age; however, current data has disputed this historical inaccuracy.[4]
Histopathology
Microscopically corneal arcus presents as non-unique lipid infiltration. On histologic analysis, the lipids can often be visualized in the peripheral regions of the cornea, and notably, the central corneal regions are often spared. The lipid deposition usually occurs in the extracellular region. This being said, the diagnosis of corneal arcus is made visually with a slit-lamp examination, and histologic analysis is not the standard of diagnosis in a clinical setting.[4][5][6]
History and Physical
Corneal arcus usually presents as narrow rings of white or gray hazy lipid deposits around the cornea. Although they usually begin in the periphery, they can progress over time and an entire ring can form around the cornea. Further investigation may be needed if they present in patients younger than 40, or if they present unilaterally.[7]
Evaluation
Often corneal arcus are benign findings in the elderly. In individuals under 50 (especially men), the condition is associated with a greater incidence of underlying atherosclerotic disease. These associations warrant a lipid analysis in individuals with corneal arcus in patients under the age of 50, which is not necessary for individuals greater than 50. Although the association between corneal arcus in men younger than 50 and underlying lipid metabolism disorders is significant, it is important to note that sometimes arcus can be clinically insignificant even in men less than 50. The presence of unilateral corneal arcus may be indicative of advanced carotid vascular disease.[8]
Treatment / Management
Arcus senilis in of themselves do not warrant treatment, as they are clinically insignificant and asymptomatic; however, if after further assessment an underlying disorder is found to be the cause of the arcus the disorder should be treated, i.e. if a patient is found to have underlying hypercholesteremia this condition should be addressed through environmental, and pharmacologic treatment options.[4]
Differential Diagnosis
The differential diagnosis of corneal arcus is broad. Some studies have shown a link between alcoholism and the presence of corneal arcus; however, this is likely due to the increase of free fatty acids associated with alcohol ingestion, and not directly because of alcohol.[9] In individuals under 50, the presence of arcus could indicate an underlying atherosclerotic disease. Usually, corneal arcus occurs bilaterally; however, the presence of unilateral arcus may be associated with unilateral carotid artery stenosis. Theories suggest that this may be secondary to decreased ophthalmic blood flow in the ipsilateral side, resulting in protection from forming arcus in the ipsilateral eye (patients with carotid stenosis are likely to have an underlying condition that would result in elevated lipid levels which would, in turn, result in a greater incidence of corneal arcus). Corneal arcus has also been observed at an increased rate in individuals with familial dyslipidemias, and lipid metabolism disorders (such as lecithin- cholesterol acyltransferase deficiency). The most common underlying conditions associated with corneal arcus are lipid disorders such as hypercholesteremia; however, often, corneal arcus is benign findings in the elderly.[4][10][11]
Prognosis
The prognosis of corneal arcus is usually very favorable, as in of themselves, they are clinically insignificant. They do not affect a patient's vision, and no ulcerations or neo-vascularization or proliferation have been observed secondary to corneal arcus. One of the primary concerns the patients have is cosmetic.[4]
Complications
There are usually no complications secondary to corneal arcus; however, the arcus themselves may be a complication of an underlying condition. This is usually a disorder of lipid metabolism, or if unilateral carotid vascular disease.
Consultations
Corneal arcus is often clearly seen on a physical exam; however, if there are doubts about the diagnosis, the patient should be referred to an optometrist or ophthalmologist for further assessment.
Deterrence and Patient Education
There are several important things that patients should be made aware of if cornea arcus are observed on a physical exam. The first thing they should be made aware of is the lack of direct clinical significance, the arcus are not going to affect their vision, and they are unlikely to have any complications because of them. One of the concerns patients are likely to have are cosmetic, and patients should be reassured and comforted in regards to this. They should also be made aware that the arcus may be a complication of an underlying condition; which may need to be assessed. They should also be made aware that the arcus are unlikely to regress, even if the underlying condition is assessed. Patients should also be consoled on the cosmetic implication of the arcus.
Pearls and Other Issues
Further research is required to elucidate the actual mechanism of arcus formation; the current theories are fairly unsubstantiated, and more research could be done to elucidate the relationship between arcus and systemic diseases further. The relationship between underlying lipid disease and arcus should be further elucidated to make further recommendations. The relationship between unilateral arcus and carotid vascular disease should also be studied further.
Enhancing Healthcare Team Outcomes
The management of corneal arcus while often clinically insignificant requires an interprofessional approach. If the patient is young the clinician may decide to further assess lipids. If the patient is older the may decide to monitor the condition and not proceed with any further diagnostic studies. An ophthalmology nurse will be involved in a more complete assessment and may assist with patient education. Nurses coordinate care and document for the team. If a future lipid study is required a nurse will likely be required to perform this test. Pending the results of the lipid study, additional healthcare professionals may be required including cardiology, vascular surgery, neurology, etc. This interprofessional team paradigm will drive better patient outcomes. [Level 5]