[1]
Vohra S, Arnold G, Doshi S, Marcantonio D. Normal MR imaging anatomy of the thigh and leg. Magnetic resonance imaging clinics of North America. 2011 Aug:19(3):621-36, ix. doi: 10.1016/j.mric.2011.05.011. Epub 2011 Jun 14
[PubMed PMID: 21816335]
[2]
Mateen S, Ali S, Meyr AJ. Normal Distal Excursion of the Peroneus Brevis Myotendinous Junction. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons. 2021 Oct 22:():. pii: S1067-2516(21)00398-7. doi: 10.1053/j.jfas.2021.10.013. Epub 2021 Oct 22
[PubMed PMID: 34785130]
[3]
Imre N, Kocabiyik N, Sanal HT, Uysal M, Ozan H, Yazar F. The peroneus brevis tendon at its insertion site on fifth metatarsal bone. Foot and ankle surgery : official journal of the European Society of Foot and Ankle Surgeons. 2016 Mar:22(1):41-5. doi: 10.1016/j.fas.2015.04.009. Epub 2015 Jun 14
[PubMed PMID: 26869499]
[4]
Davda K, Malhotra K, O'Donnell P, Singh D, Cullen N. Peroneal tendon disorders. EFORT open reviews. 2017 Jun:2(6):281-292. doi: 10.1302/2058-5241.2.160047. Epub 2017 Jun 22
[PubMed PMID: 28736620]
[5]
Mabit C, Salanne P, Boncoeur-Martel MP, Fiorenza F, Valleix D, Descottes B, Caix M. [The lateral retromalleolar groove: a radio-anatomic study]. Bulletin de l'Association des anatomistes. 1996 Jun:80(249):17-21
[PubMed PMID: 9102053]
[6]
Drakonaki EE, Gataa KG, Solidakis N, Szaro P. Anatomical variations and interconnections of the superior peroneal retinaculum to adjacent lateral ankle structures: a preliminary imaging anatomy study. Journal of ultrasonography. 2021:21(84):12-21. doi: 10.15557/JoU.2021.0003. Epub 2021 Mar 8
[PubMed PMID: 33791112]
[7]
Gomes MDR, Pinto AP, Fabián AA, Gomes TJM, Navarro A, Oliva XM. Insertional anatomy of peroneal brevis and longus tendon - A cadaveric study. Foot and ankle surgery : official journal of the European Society of Foot and Ankle Surgeons. 2019 Oct:25(5):636-639. doi: 10.1016/j.fas.2018.07.005. Epub 2018 Jul 23
[PubMed PMID: 30321932]
[8]
Bavdek R, Zdolšek A, Strojnik V, Dolenec A. Peroneal muscle activity during different types of walking. Journal of foot and ankle research. 2018:11():50. doi: 10.1186/s13047-018-0291-0. Epub 2018 Sep 3
[PubMed PMID: 30202446]
[9]
Karykowska A, Rohan-Fugiel A, Mączka G, Grzelak J, Gworys B, Tarkowski V, Domagała Z. Topography of muscular branches of the superficial fibular nerve based on anatomical preparation of human foetuses. Annals of anatomy = Anatomischer Anzeiger : official organ of the Anatomische Gesellschaft. 2021 Sep:237():151728. doi: 10.1016/j.aanat.2021.151728. Epub 2021 Apr 3
[PubMed PMID: 33823227]
[10]
Ohmura Y, Morokuma S, Kato K, Kuniyoshi Y. Species-specific Posture of Human Foetus in Late First Trimester. Scientific reports. 2018 Jan 8:8(1):27. doi: 10.1038/s41598-017-18384-w. Epub 2018 Jan 8
[PubMed PMID: 29311655]
[11]
Gosselin MM, Haynes JA, McCormick JJ, Johnson JE, Klein SE. The Arterial Anatomy of the Lateral Ligament Complex of the Ankle: A Cadaveric Study. The American journal of sports medicine. 2019 Jan:47(1):138-143. doi: 10.1177/0363546518808060. Epub 2018 Nov 19
[PubMed PMID: 30452871]
[12]
Uhl JF, Gillot C. Anatomy of the veno-muscular pumps of the lower limb. Phlebology. 2015 Apr:30(3):180-93. doi: 10.1177/0268355513517686. Epub 2014 Jan 10
[PubMed PMID: 24415543]
[13]
Solomon LB, Ferris L, Tedman R, Henneberg M. Surgical anatomy of the sural and superficial fibular nerves with an emphasis on the approach to the lateral malleolus. Journal of anatomy. 2001 Dec:199(Pt 6):717-23
[PubMed PMID: 11787825]
[14]
Bilgili MG, Kaynak G, Botanlioğlu H, Basaran SH, Ercin E, Baca E, Uzun I. Peroneus quartus: prevalance and clinical importance. Archives of orthopaedic and trauma surgery. 2014 Apr:134(4):481-7. doi: 10.1007/s00402-014-1937-4. Epub 2014 Feb 14
[PubMed PMID: 24525795]
[15]
Sobel M, Levy ME, Bohne WH. Congenital variations of the peroneus quartus muscle: an anatomic study. Foot & ankle. 1990 Oct:11(2):81-9
[PubMed PMID: 2265813]
[16]
Zammit J, Singh D. The peroneus quartus muscle. Anatomy and clinical relevance. The Journal of bone and joint surgery. British volume. 2003 Nov:85(8):1134-7
[PubMed PMID: 14653594]
[17]
Wang XT, Rosenberg ZS, Mechlin MB, Schweitzer ME. Normal variants and diseases of the peroneal tendons and superior peroneal retinaculum: MR imaging features. Radiographics : a review publication of the Radiological Society of North America, Inc. 2005 May-Jun:25(3):587-602
[PubMed PMID: 15888611]
[18]
Mirmiran R, Squire C, Wassell D. Prevalence and Role of a Low-Lying Peroneus Brevis Muscle Belly in Patients With Peroneal Tendon Pathologic Features: A Potential Source of Tendon Subluxation. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons. 2015 Sep-Oct:54(5):872-5. doi: 10.1053/j.jfas.2015.02.012. Epub 2015 May 19
[PubMed PMID: 25998478]
[19]
Geller J, Lin S, Cordas D, Vieira P. Relationship of a low-lying muscle belly to tears of the peroneus brevis tendon. American journal of orthopedics (Belle Mead, N.J.). 2003 Nov:32(11):541-4
[PubMed PMID: 14653483]
[20]
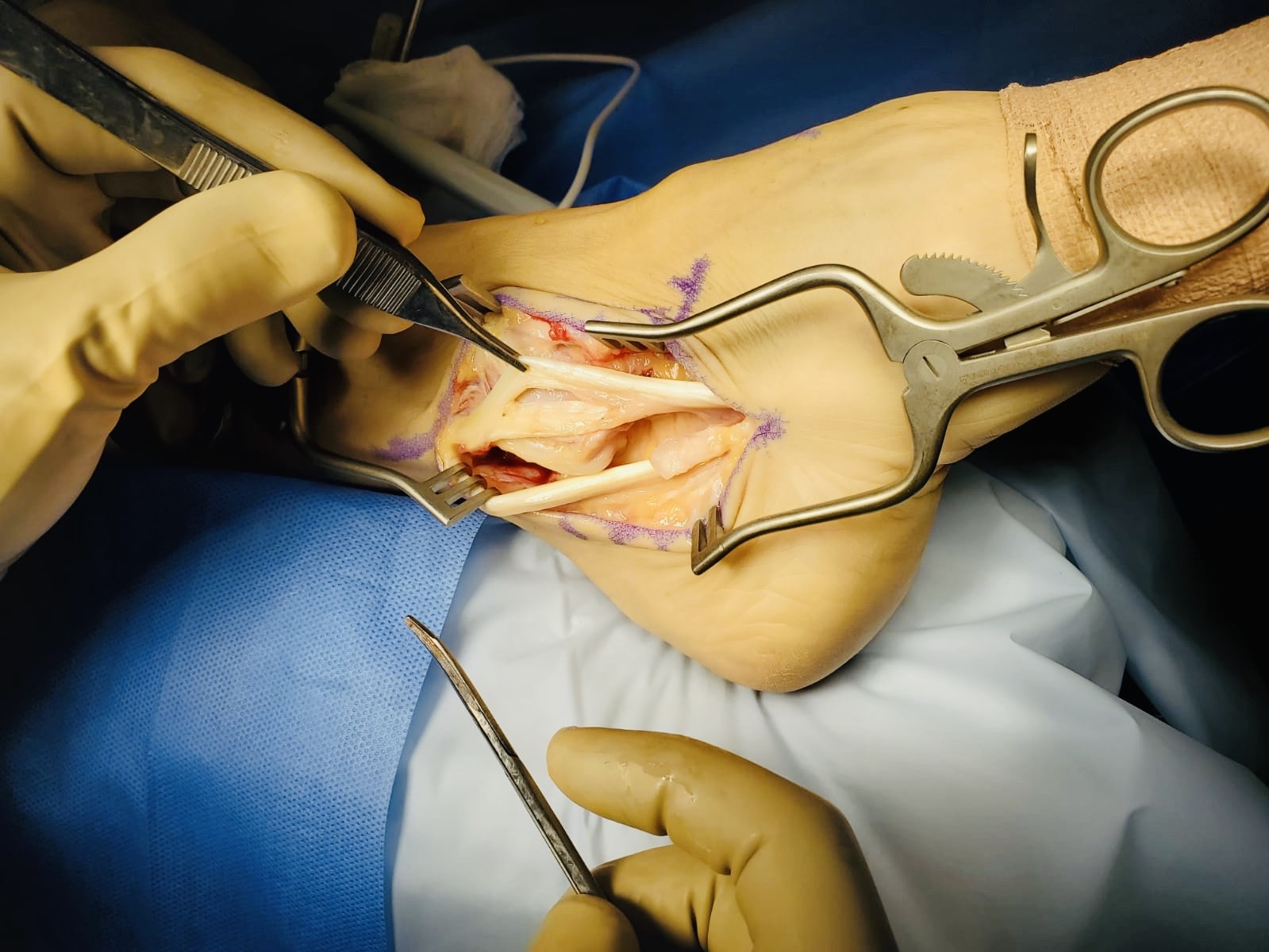
Pitarini A, Anastasia M, Kennedy D, Sumargono E, Kholinne E. The Surgical Procedure in Managing Peroneal Tendon Injury: A Case Series. Orthopedic research and reviews. 2022:14():255-262. doi: 10.2147/ORR.S351356. Epub 2022 Jul 27
[PubMed PMID: 35923302]
Level 2 (mid-level) evidence
[21]
Schubert CD, von Freyhold-Hünecken J, Bittrich T, Onken ML, Tomala L, Montenegro V, Elsner J. Distally Based Peroneus Brevis Muscle Flap for Lower Extremity Defect Reconstruction in Severely Ill Multimorbid Patients. Zeitschrift fur Orthopadie und Unfallchirurgie. 2022 Aug:160(4):422-430. doi: 10.1055/a-1373-6564. Epub 2021 Apr 19
[PubMed PMID: 33873224]
[22]
Ebrahiem AA, Manas RK, Vinagre G. Distally Based Sural Artery Peroneus Flap (DBSPF) for Foot and Ankle Reconstruction. Plastic and reconstructive surgery. Global open. 2017 Apr:5(4):e1276. doi: 10.1097/GOX.0000000000001276. Epub 2017 Apr 18
[PubMed PMID: 28507850]
[23]
Doherty C, Delahunt E, Caulfield B, Hertel J, Ryan J, Bleakley C. The incidence and prevalence of ankle sprain injury: a systematic review and meta-analysis of prospective epidemiological studies. Sports medicine (Auckland, N.Z.). 2014 Jan:44(1):123-40. doi: 10.1007/s40279-013-0102-5. Epub
[PubMed PMID: 24105612]
Level 2 (mid-level) evidence
[24]
Al Adal S, Pourkazemi F, Mackey M, Hiller CE. The Prevalence of Pain in People With Chronic Ankle Instability: A Systematic Review. Journal of athletic training. 2019 Jun:54(6):662-670. doi: 10.4085/1062-6050-531-17. Epub 2019 Jun 11
[PubMed PMID: 31184959]
Level 1 (high-level) evidence
[25]
Gribble PA, Kleis RE, Simon JE, Vela LI, Thomas AC. Differences in health-related quality of life among patients after ankle injury. Frontiers in sports and active living. 2022:4():909921. doi: 10.3389/fspor.2022.909921. Epub 2022 Aug 3
[PubMed PMID: 35992155]
Level 2 (mid-level) evidence
[26]
Philbin TM, Landis GS, Smith B. Peroneal tendon injuries. The Journal of the American Academy of Orthopaedic Surgeons. 2009 May:17(5):306-17
[PubMed PMID: 19411642]
[27]
Metzl JA, Bowers MW, Anderson RB. Fifth Metatarsal Jones Fractures: Diagnosis and Treatment. The Journal of the American Academy of Orthopaedic Surgeons. 2022 Feb 15:30(4):e470-e479. doi: 10.5435/JAAOS-D-21-00542. Epub
[PubMed PMID: 34932521]
[28]
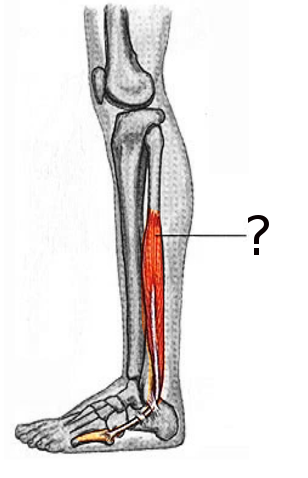
Khan IA, Mahabadi N, D’Abarno A, Varacallo M. Anatomy, Bony Pelvis and Lower Limb: Leg Lateral Compartment. StatPearls. 2023 Jan:():
[PubMed PMID: 30137811]