[1]
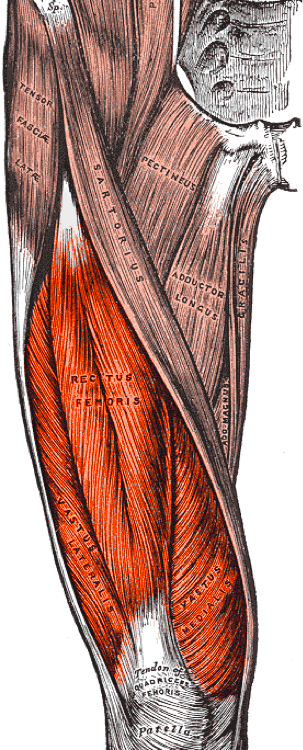
Bordoni B, Varacallo M. Anatomy, Bony Pelvis and Lower Limb: Thigh Quadriceps Muscle. StatPearls. 2023 Jan:():
[PubMed PMID: 30020706]
[2]
Kumaravel M, Bawa P, Murai N. Magnetic resonance imaging of muscle injury in elite American football players: Predictors for return to play and performance. European journal of radiology. 2018 Nov:108():155-164. doi: 10.1016/j.ejrad.2018.09.028. Epub 2018 Sep 27
[PubMed PMID: 30396649]
[4]
Biondi NL, Varacallo M. Anatomy, Bony Pelvis and Lower Limb: Vastus Lateralis Muscle. StatPearls. 2023 Jan:():
[PubMed PMID: 30335342]
[5]
Mendiguchia J, Alentorn-Geli E, Idoate F, Myer GD. Rectus femoris muscle injuries in football: a clinically relevant review of mechanisms of injury, risk factors and preventive strategies. British journal of sports medicine. 2013 Apr:47(6):359-66. doi: 10.1136/bjsports-2012-091250. Epub 2012 Aug 3
[PubMed PMID: 22864009]
[6]
Volk WR, Yagnik GP, Uribe JW. Complications in brief: Quadriceps and patellar tendon tears. Clinical orthopaedics and related research. 2014 Mar:472(3):1050-7. doi: 10.1007/s11999-013-3396-6. Epub 2013 Dec 12
[PubMed PMID: 24338040]
[7]
Cross TM, Gibbs N, Houang MT, Cameron M. Acute quadriceps muscle strains: magnetic resonance imaging features and prognosis. The American journal of sports medicine. 2004 Apr-May:32(3):710-9
[PubMed PMID: 15090389]
[8]
Gyftopoulos S, Rosenberg ZS, Schweitzer ME, Bordalo-Rodrigues M. Normal anatomy and strains of the deep musculotendinous junction of the proximal rectus femoris: MRI features. AJR. American journal of roentgenology. 2008 Mar:190(3):W182-6. doi: 10.2214/AJR.07.2947. Epub
[PubMed PMID: 18287410]
[9]
Pesquer L, Poussange N, Sonnery-Cottet B, Graveleau N, Meyer P, Dallaudiere B, Feldis M. Imaging of rectus femoris proximal tendinopathies. Skeletal radiology. 2016 Jul:45(7):889-97. doi: 10.1007/s00256-016-2345-3. Epub 2016 Mar 8
[PubMed PMID: 26956398]
[10]
Esser S, Jantz D, Hurdle MF, Taylor W. Proximal Rectus Femoris Avulsion: Ultrasonic Diagnosis and Nonoperative Management. Journal of athletic training. 2015 Jul:50(7):778-80. doi: 10.4085/1052-6050-50.2.13. Epub 2015 May 15
[PubMed PMID: 25978099]
[11]
Colombelli A, Polidoro F, Guerra G, Belluati A. Patellar and quadriceps tendons acute repair with suture anchors. Acta bio-medica : Atenei Parmensis. 2019 Jan 14:90(1-S):209-213. doi: 10.23750/abm.v90i1-S.8108. Epub 2019 Jan 14
[PubMed PMID: 30715027]
[12]
Lempainen L, Mechó S, Valle X, Mazzoni S, Villalon J, Freschi M, Stefanini L, García-Romero-Pérez A, Burova M, Pleshkov P, Pruna R, Pasta G, Kosola J. Management of anterior thigh injuries in soccer players: practical guide. BMC sports science, medicine & rehabilitation. 2022 Mar 18:14(1):41. doi: 10.1186/s13102-022-00428-y. Epub 2022 Mar 18
[PubMed PMID: 35303927]
[13]
Marques JP, Pinheiro JP, Santos Costa J, Moura D. Myositis ossificans of the quadriceps femoris in a soccer player. BMJ case reports. 2015 Aug 11:2015():. doi: 10.1136/bcr-2015-210545. Epub 2015 Aug 11
[PubMed PMID: 26264943]
Level 3 (low-level) evidence
[14]
Devilbiss Z, Hess M, Ho GWK. Myositis Ossificans in Sport: A Review. Current sports medicine reports. 2018 Sep:17(9):290-295. doi: 10.1249/JSR.0000000000000515. Epub
[PubMed PMID: 30204632]