[1]
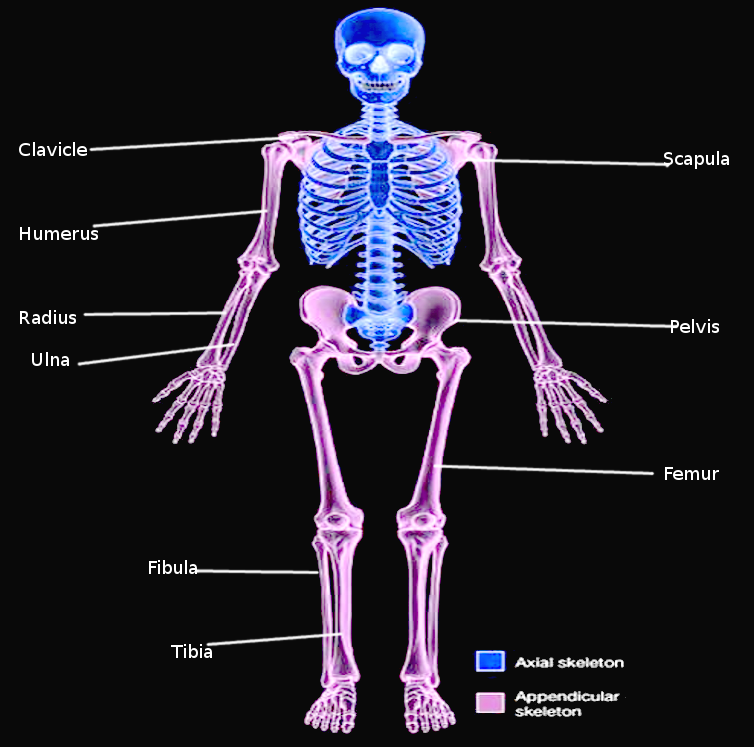
Docherty B. Skeletal system: part four--the appendicular skeleton. Nursing times. 2007 Feb 20-26:103(8):26-7
[PubMed PMID: 17333873]
[2]
Panchal-Kildare S, Malone K. Skeletal anatomy of the hand. Hand clinics. 2013 Nov:29(4):459-71. doi: 10.1016/j.hcl.2013.08.001. Epub
[PubMed PMID: 24209945]
[3]
Wobser AM, Adkins Z, Wobser RW. Anatomy, Abdomen and Pelvis: Bones (Ilium, Ischium, and Pubis). StatPearls. 2024 Jan:():
[PubMed PMID: 30137809]
[6]
Fox AJ, Wanivenhaus F, Rodeo SA. The basic science of the patella: structure, composition, and function. The journal of knee surgery. 2012 May:25(2):127-41
[PubMed PMID: 22928430]
[8]
Dhawan R, Singh RA, Tins B, Hay SM. Sternoclavicular joint. Shoulder & elbow. 2018 Oct:10(4):296-305. doi: 10.1177/1758573218756880. Epub 2018 Apr 2
[PubMed PMID: 30214497]
[9]
Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. Journal of anatomy. 2012 Dec:221(6):537-67. doi: 10.1111/j.1469-7580.2012.01564.x. Epub 2012 Sep 19
[PubMed PMID: 22994881]
Level 3 (low-level) evidence
[10]
Frank RM, Ramirez J, Chalmers PN, McCormick FM, Romeo AA. Scapulothoracic anatomy and snapping scapula syndrome. Anatomy research international. 2013:2013():635628. doi: 10.1155/2013/635628. Epub 2013 Nov 28
[PubMed PMID: 24369502]
[11]
McKeon PO, Hertel J, Bramble D, Davis I. The foot core system: a new paradigm for understanding intrinsic foot muscle function. British journal of sports medicine. 2015 Mar:49(5):290. doi: 10.1136/bjsports-2013-092690. Epub 2014 Mar 21
[PubMed PMID: 24659509]
Level 3 (low-level) evidence
[12]
Al-Qattan MM, Kozin SH. Update on embryology of the upper limb. The Journal of hand surgery. 2013 Sep:38(9):1835-44. doi: 10.1016/j.jhsa.2013.03.018. Epub 2013 May 17
[PubMed PMID: 23684522]
[13]
Ortega N, Behonick DJ, Werb Z. Matrix remodeling during endochondral ossification. Trends in cell biology. 2004 Feb:14(2):86-93
[PubMed PMID: 15102440]
[14]
Verbruggen SW, Nowlan NC. Ontogeny of the Human Pelvis. Anatomical record (Hoboken, N.J. : 2007). 2017 Apr:300(4):643-652. doi: 10.1002/ar.23541. Epub
[PubMed PMID: 28297183]
[15]
Yiming A, Baqué P, Rahili A, Mayer J, Braccini AL, Fontaine A, Leplatois A, Clavé A, Bourgeon A, de Peretti F. Anatomical study of the blood supply of the coxal bone: radiological and clinical application. Surgical and radiologic anatomy : SRA. 2002 May:24(2):81-6
[PubMed PMID: 12197024]
[16]
Zlotorowicz M, Czubak-Wrzosek M, Wrzosek P, Czubak J. The origin of the medial femoral circumflex artery, lateral femoral circumflex artery and obturator artery. Surgical and radiologic anatomy : SRA. 2018 May:40(5):515-520. doi: 10.1007/s00276-018-2012-6. Epub 2018 Apr 12
[PubMed PMID: 29651567]
[17]
Hirtler L, Lübbers A, Rath C. Vascular coverage of the anterior knee region - an anatomical study. Journal of anatomy. 2019 Aug:235(2):289-298. doi: 10.1111/joa.13004. Epub 2019 May 9
[PubMed PMID: 31070789]
[18]
Hyland S, Sinkler MA, Varacallo M. Anatomy, Bony Pelvis and Lower Limb: Popliteal Region. StatPearls. 2024 Jan:():
[PubMed PMID: 30422486]
[19]
Olewnik Ł, Łabętowicz P, Podgórski M, Polguj M, Ruzik K, Topol M. Variations in terminal branches of the popliteal artery: cadaveric study. Surgical and radiologic anatomy : SRA. 2019 Dec:41(12):1473-1482. doi: 10.1007/s00276-019-02262-3. Epub 2019 May 27
[PubMed PMID: 31134299]
[20]
Knudsen FW, Andersen M, Krag C. The arterial supply of the clavicle. Surgical and radiologic anatomy : SRA. 1989:11(3):211-4
[PubMed PMID: 2588097]
[21]
McCausland C, Sawyer E, Eovaldi BJ, Varacallo M. Anatomy, Shoulder and Upper Limb, Shoulder Muscles. StatPearls. 2024 Jan:():
[PubMed PMID: 30521257]
[22]
Haładaj R, Wysiadecki G, Dudkiewicz Z, Polguj M, Topol M. The High Origin of the Radial Artery (Brachioradial Artery): Its Anatomical Variations, Clinical Significance, and Contribution to the Blood Supply of the Hand. BioMed research international. 2018:2018():1520929. doi: 10.1155/2018/1520929. Epub 2018 Jun 11
[PubMed PMID: 29992133]
[23]
Ma CX, Pan WR, Liu ZA, Zeng FQ, Qiu ZQ, Liu MY. Deep lymphatic anatomy of the upper limb: An anatomical study and clinical implications. Annals of anatomy = Anatomischer Anzeiger : official organ of the Anatomische Gesellschaft. 2019 May:223():32-42. doi: 10.1016/j.aanat.2019.01.005. Epub 2019 Feb 1
[PubMed PMID: 30716466]
Level 2 (mid-level) evidence
[24]
Orebaugh SL, Williams BA. Brachial plexus anatomy: normal and variant. TheScientificWorldJournal. 2009 Apr 28:9():300-12. doi: 10.1100/tsw.2009.39. Epub 2009 Apr 28
[PubMed PMID: 19412559]
[25]
Di Benedetto P, Pinto G, Arcioni R, De Blasi RA, Sorrentino L, Rossifragola I, Baciarello M, Capotondi C. Anatomy and imaging of lumbar plexus. Minerva anestesiologica. 2005 Sep:71(9):549-54
[PubMed PMID: 16166916]
[26]
Dupont G, Unno F, Iwanaga J, Oskouian RJ, Tubbs RS. A Variant of the Sciatic Nerve and its Clinical Implications. Cureus. 2018 Jun 25:10(6):e2874. doi: 10.7759/cureus.2874. Epub 2018 Jun 25
[PubMed PMID: 30155377]
[27]
Montalvo N, Redrobán L, Espín VH. Incomplete duplication of a lower extremity (polymelia): a case report. Journal of medical case reports. 2014 Jun 12:8():184. doi: 10.1186/1752-1947-8-184. Epub 2014 Jun 12
[PubMed PMID: 24920152]
Level 3 (low-level) evidence
[28]
Malik S. Syndactyly: phenotypes, genetics and current classification. European journal of human genetics : EJHG. 2012 Aug:20(8):817-24. doi: 10.1038/ejhg.2012.14. Epub 2012 Feb 15
[PubMed PMID: 22333904]
[29]
Kvernmo HD, Haugstvedt JR. Treatment of congenital syndactyly of the fingers. Tidsskrift for den Norske laegeforening : tidsskrift for praktisk medicin, ny raekke. 2013 Aug 20:133(15):1591-5. doi: 10.4045/tidsskr.13.0147. Epub
[PubMed PMID: 23970273]
[30]
Comer GC, Potter M, Ladd AL. Polydactyly of the Hand. The Journal of the American Academy of Orthopaedic Surgeons. 2018 Feb 1:26(3):75-82. doi: 10.5435/JAAOS-D-16-00139. Epub
[PubMed PMID: 29309292]
[31]
Belthur MV, Linton JL, Barnes DA. The spectrum of preaxial polydactyly of the foot. Journal of pediatric orthopedics. 2011 Jun:31(4):435-47. doi: 10.1097/BPO.0b013e3182199a68. Epub
[PubMed PMID: 21572282]
[32]
Kyriazis Z, Kollia P, Grivea I, Varitimidis SE, Constantoulakis P, Dailiana ZH. Thumb duplication: molecular analysis of different clinical types. European journal of orthopaedic surgery & traumatology : orthopedie traumatologie. 2019 Feb:29(2):421-426. doi: 10.1007/s00590-018-2343-3. Epub 2018 Nov 29
[PubMed PMID: 30498907]
[33]
Hovius SER, Potuijt JWP, van Nieuwenhoven CA. Triphalangeal thumb: clinical features and treatment. The Journal of hand surgery, European volume. 2019 Jan:44(1):69-79. doi: 10.1177/1753193418797922. Epub 2018 Sep 17
[PubMed PMID: 30223699]
[34]
Potuijt JWP, Galjaard RH, van der Spek PJ, van Nieuwenhoven CA, Ahituv N, Oberg KC, Hovius SER. A multidisciplinary review of triphalangeal thumb. The Journal of hand surgery, European volume. 2019 Jan:44(1):59-68. doi: 10.1177/1753193418803521. Epub 2018 Oct 14
[PubMed PMID: 30318985]
[35]
Shon HC, Park JK, Kim DS, Kang SW, Kim KJ, Hong SH. Supracondylar process syndrome: two cases of median nerve neuropathy due to compression by the ligament of Struthers. Journal of pain research. 2018:11():803-807. doi: 10.2147/JPR.S160861. Epub 2018 Apr 16
[PubMed PMID: 29713193]
Level 3 (low-level) evidence
[36]
Opanova MI, Atkinson RE. Supracondylar process syndrome: case report and literature review. The Journal of hand surgery. 2014 Jun:39(6):1130-5. doi: 10.1016/j.jhsa.2014.03.035. Epub
[PubMed PMID: 24862112]
Level 3 (low-level) evidence
[37]
Gamble JG, Krygier JE. Fracture of the Supracondylar Process in a Child: A Case Report and Review of the Literature. JBJS case connector. 2019 Dec:9(4):e0396. doi: 10.2106/JBJS.CC.18.00396. Epub
[PubMed PMID: 31633496]
Level 3 (low-level) evidence
[38]
Karl JW, Olson PR, Rosenwasser MP. The Epidemiology of Upper Extremity Fractures in the United States, 2009. Journal of orthopaedic trauma. 2015 Aug:29(8):e242-4. doi: 10.1097/BOT.0000000000000312. Epub
[PubMed PMID: 25714441]
[39]
Waterman BR, Gun B, Bader JO, Orr JD, Belmont PJ Jr. Epidemiology of Lower Extremity Stress Fractures in the United States Military. Military medicine. 2016 Oct:181(10):1308-1313
[PubMed PMID: 27753569]
[40]
Eslick R, Talaulikar D. Multiple myeloma: from diagnosis to treatment. Australian family physician. 2013 Oct:42(10):684-8
[PubMed PMID: 24130968]
[41]
Rogozhin DV, Bulycheva IV, Konovalov DM, Talalaev AG, Roshchin VY, Ektova AP, Bogoroditsky YS, Strykov VA, Kazakova AN, Olshanskaya YV, Kachanov DY, Tereshchenko GV. [Classical osteosarcoma in children and adolescent]. Arkhiv patologii. 2015 Sep-Oct:77(5):68-74. doi: 10.17116/patol201577568-74. Epub
[PubMed PMID: 27077157]
[42]
Wong AK. A comparison of peripheral imaging technologies for bone and muscle quantification: a technical review of image acquisition. Journal of musculoskeletal & neuronal interactions. 2016 Dec 14:16(4):265-282
[PubMed PMID: 27973379]