Introduction
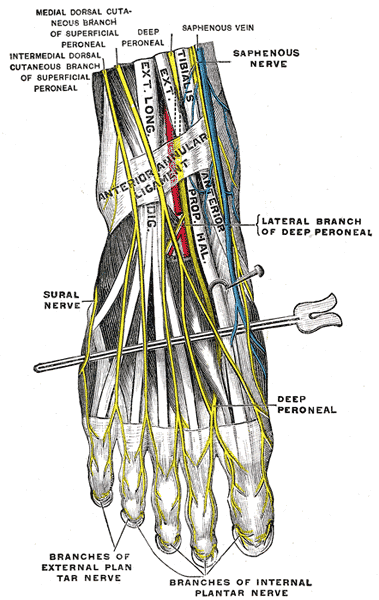
The foot receives its nerve supply from the superficial peroneal (fibular) nerve, deep fibular nerve, tibial nerve (and its branches), sural nerve, and saphenous nerve. These nerves come from peripheral nerves that arise from the L4 to S3 nerve roots and contribute to the somatic motor function, general sensory information, and the cutaneous sensation of the foot.[1][2]
Structure and Function
The foot nerves originate from the sciatic nerve, made up of the L4 to S3 nerve roots. The sciatic nerve, which provides motor innervation to the muscles of the posterior thigh and sensory innervation to the lateral side of the lower leg and lateral side and sole of the foot, ends just above the posterior knee in the popliteal fossa and bifurcates into the common fibular and tibial nerves. The common fibular nerve continues distally into the anterior and lateral compartments of the leg and foot whereas the tibial nerve descends towards the posterior compartment.[1][2] Both nerves contribute significant terminal branches that will eventually supply the foot.
The common fibular nerve bifurcates into the superficial and deep fibular nerves. The superficial fibular nerve supplies the motor innervation to the lateral compartment of the leg, which is responsible for foot eversion, while the deep fibular nerve supplies the motor innervation to the anterior compartment, responsible for ankle dorsiflexion, toe extension, and foot inversion.[2][3] Within the lateral compartment, the superficial fibular nerve courses within the peroneus longus muscle and emerges through the anterolateral aspect of the musculature about 12 cm above the ankle joint at the level of a defect in the deep (crural) fascia. As it arises in the foot and travels more inferiorly, the superficial fibular nerve further divides into two branches: medial and intermediate dorsal cutaneous nerves, which may be subject to anatomic variation. The remaining portion of the superficial fibular nerve in the foot is purely sensory as it supplies sensory information to the dorsal aspect of the foot, except for the first dorsal web space.[4]
The deep fibular nerve descends lateral to the anterior tibial artery and is located just anterior to the interosseous membrane within the anterior compartment of the leg. At approximately 1.3 cm above the ankle joint, the nerve divides into a lateral branch and a medial branch. The lateral branch courses deep to the extensor digitorum brevis and extensor digitorum hallucis muscles and provides their motor innervations and some sensory innervation to the ankle. The medial branch courses medially on the dorsum of the foot, laterally to the dorsalis pedis artery, and inferiorly to the extensor hallucis brevis tendon as it moves towards the first dorsal web space to supply its sensory innervation. It is important to note that although the deep fibular nerve usually courses laterally to the anterior tibial artery, some anatomical variations exist. Regardless of variation, the anterior tibial artery makes an excellent landmark for identifying the deep fibular nerve in the leg on MR imaging. The region where the extensor hallucis brevis tendon crosses over the medial branch also serves as an excellent landmark for identification of the deep fibular nerve in the foot.[4]
The tibial nerve arises in the popliteal fossa as the other branch of the sciatic nerve and supplies the motor innervation to the posterior deep flexor compartment of the lower leg. Proximal to the tip of the medial malleolus, the tibial nerve bifurcates into the medial and lateral plantar nerves at the level of the tarsal tunnel with some variation. This anatomy makes the posterior aspect of the medial malleolus an excellent landmark for visualizing the tibial nerve on MR imaging where it is visible between the flexor digitorum longus and flexor hallucis longus muscle tendons. The medial plantar nerve travels a course lateral to the posterior tibial artery and anterior to the medial plantar artery. Proximally, it travels between the quadratus plantae and abductor hallucis muscles. Distally, it lies close to the master knot of Henry (the crossover point of the flexor digitorum longus and flexor hallucis longus tendons), an excellent anatomical landmark for visualization on MR imaging, and continues its course medial to the flexor digitorum brevis muscle. From there, the medial plantar nerve continues to divide into muscular and cutaneous branches, ultimately contributing to the motor innervation to the abductor hallucis, flexor digitorum brevis, flexor hallucis brevis, and first lumbrical muscles and the sensory innervation to the medial side of the sole (i.e. first three digits and the medial half of the fourth digit). The lateral plantar nerve courses posterior to the posterior tibial artery and in between the lateral and medial plantar arteries. Proximally, it travels between the quadratus plantae and flexor digitorum brevis muscles in the middle plantar space and continues laterally to the flexor digitorum brevis muscle distally. From there, it divides into superficial and deep branches that provide motor innervation to all the intrinsic muscles of the foot and the sensory innervation to the lateral side of the sole (i.e., lateral half of the fourth digit and fifth digit).[4]
Other direct and indirect branches of the tibial nerve in the foot include the medial calcaneal, inferior calcaneal, and digital nerves. The medial calcaneal nerve is a sensory nerve that typically arises from the tibial nerve, although variations exist, proximal to the tarsal tunnel, 4 to 10 cm above the ankle joint, and courses medially towards the medial heel and calcaneus. Visualization on MR imaging is difficult because of the many variations in its origin and course. The inferior calcaneal nerve, also known as the nerve to the abductor digiti minimi or Baxter’s nerve, typically arises as the first branch of the lateral plantar nerve and courses approximately 5 mm anterior to the anterior tubercle of the calcaneus, which may serve as an anatomical landmark on MR imaging. This nerve provides both motor innervation to the abductor digiti minimi muscle and sensory innervation to the anterior aspect of the calcaneus. The digital nerves originate from both the medial and lateral plantar nerves and provide innervation to the plantar web spaces. The digital nerves that come from the medial plantar nerve contribute to the innervation of the first three web spaces whereas the digital nerves that stem from the lateral plantar nerve innervate the fourth web space. The third web space typically receives communicating branches from both the medial and lateral plantar nerves and is subsequently most commonly involved in Morton neuromas.[4]
The sural nerve arises from the branches of both the common fibular nerve (lateral sural nerve) and tibial nerves (medial sural nerve). In its descent towards the distal foot, the sural nerve travels between the two heads of the gastrocnemius muscle proximally and courses subcutaneously along the posterolateral aspect of the lower leg. It lies close to the lesser saphenous vein, which may serve as an anatomical landmark on MR imaging, and is lateral to the Achilles tendon. At the level of the ankle, it further branches out and provides sensory innervation to the lateral aspect of the foot and the fifth toe.[4]
Last, the saphenous nerve arises from the femoral nerve. Proximally, it travels medially within the adductor canal and exits distally between the sartorius and the gracilis muscles. It continues its descent within the subcutaneous fat along the medial aspect of the lower leg where it courses next to the great saphenous vein, which can function as an anatomical landmark. Distally, the nerve crosses the medial malleolus towards the medial aspect of the dorsum of the foot where it provides sensory innervation to the medial foot up to the first metatarsophalangeal joint.[4]
Embryology
Embryological derivatives of the foot nerves arise from the development of the central and peripheral nervous systems. This development starts with neurulation beginning around week 3 of the developing fetus. The notochord, which comes from midline mesoderm, induces the overlying ectoderm to form the neural plate (neuroectoderm). By the end of the third week, the lateral edges of the neural plate rise to become the neural folds while the center of the plate forms the neural groove. The neural plate then folds onto itself to create the neural tube and neural crest cells (formed as detachments of the neural cells at the crest of the neural folds upon closure of the neural plate) by the end of week 4, thus completing the process of neurulation.[5]
The neural tube will eventually become the brain and the spinal cord as part of the central nervous system whereas the neural crest cells will migrate throughout the embryo to form many structures, including the spinal nerves of the upper and lower limbs, as part of the peripheral nervous system.[5][6]
Blood Supply and Lymphatics
The fibular, anterior tibial, and posterior tibial arteries and their branches provide the blood supply of the foot.[7] The superficial fibular nerve receives its blood supply predominantly from the fibular and posterior tibial arteries within the lateral compartment of the lower limb and from the anterior tibial artery as it moves towards the dorsum of the foot.[8] The deep fibular nerve receives supply by the anterior tibial artery with little variation to its blood supply compared to the tibial nerve.[9] The vascular supply to the tibial nerve is by numerous arterial branches of the popliteal, fibular, and posterior tibial arteries as it courses through the lower limb into the foot.[10] Last, the lateral and medial plantar nerves receive their blood supply from corresponding arteries that come from branches of the posterior tibial artery in the foot.[11]
Lymphatic drainage of the foot comes from the popliteal lymph nodes that subsequently enter the superficial and deep inguinal lymph nodes.[7]
Nerves
The nerves of the foot, their branches, and their origins include [4]
-
Superficial peroneal (fibular) nerve (arises from the common fibular nerve)
-
Deep peroneal (fibular) nerve (arising from the common fibular nerve)
-
Tibial nerve (arises in the popliteal fossa as a division of the sciatic nerve)
-
Medial plantar nerve (arises from the larger terminal branch of the tibial nerve)
- Digital nerves (arise from both the medial and lateral plantar nerves)
-
Lateral plantar nerve (arises from the smaller terminal branch of the tibial nerve)
- Inferior calcaneal nerve, also known as Baxter’s nerve (typically arises as the first branch of the lateral plantar nerve)
-
Medial calcaneal nerve (typically arises from the tibial nerve)
-
Sural nerve (typically arises from branches of both the common fibular and tibial nerves)
-
Saphenous nerve (arises from the femoral nerve)
Muscles
Muscles that involve the foot are extrinsic (originate above the ankle and insert onto the foot) or intrinsic (originate and insert within the foot). Extrinsic muscles divide into three compartments: anterior, lateral, and posterior. The deep fibular nerve innervates the muscles in the anterior compartment of the leg (i.e., tibialis anterior, extensor hallucis longus, extensor digitorum longus, and fibularis tertius muscles), which manage ankle dorsiflexion, toe extension, and foot inversion.[2][3] The superficial fibular nerve innervates the muscles in the lateral compartment (i.e., fibularis longus and fibularis brevis muscles), which are mainly responsible for foot eversion.[2][3] Last, the tibial nerve innervates the muscles in the posterior compartment (i.e., gastrocnemius, plantaris, soleus, popliteus, flexor hallucis longus, flexor digitorum longus, and tibialis posterior muscles), which manage plantar flexion, toe flexion, and foot inversion.[2]
Intrinsic muscles manage the fine movement of the toes. On the dorsal aspect of the foot, the deep fibular nerve innervates the extensor digitorum brevis and the extensor hallucis brevis.[9] On the plantar aspect of the foot, the lateral plantar nerve innervates all the intrinsic muscles except for the four muscles supplied by the medial plantar nerve (i.e., abductor hallucis, flexor digitorum brevis, flexor hallicus brevis, and the first lumbrical muscles).[4] Interestingly, the first two dorsal interossei muscles may also receive innervation from the deep fibular nerve.[12] Of note, the sural and saphenous nerves are purely sensory cutaneous nerves and thus innervate none of the muscles in the foot.[13]
Physiologic Variants
Reported anatomic variations of the foot nerves are common. The superficial fibular nerve has variations of deep fascia piercings and can present in different compartments of the leg compared to its normal anatomic location in the lateral leg compartment.[8] Some reports have also revealed an accessory deep fibular nerve as a branch of the superficial fibular nerve, which provides the somatic motor innervation to the lateral portion of the extensor digitorum brevis muscle and some sensory innervation to the lateral ankle and foot.[9][14]
Other reports have commented on the variations of the bifurcation of the tibial nerve and have shown that the tibial nerve more commonly bifurcates under the tarsal tunnel (88%) than it does proximally (12%).[15] Also, the level of the division of the tibial nerve into the medial and lateral plantar nerves is variable.[4] Additionally, the medial calcaneal and inferior calcaneal nerves have been shown to have variations in their origins and the number of terminal branches. Multiple reports show that the medial calcaneal nerve most commonly originates from the tibial nerve while only a few originate from the lateral plantar nerve. The medial calcaneal nerve also most commonly presents with a single terminal branch but may have up to three terminal branches. Reports have shown that the inferior calcaneal nerve most commonly originates from the lateral plantar nerve and may have up to two terminal branches.[15][16] Also, other reports on the anatomic variations of digital nerves of the foot have also documented the absence of a communicating branch in some patients, alternating communicating branches from the fourth to the third web space and vice versa, and even neuromas in the second web space.[17]
Regarding the anatomic variations of the sural and saphenous nerves of the foot, reports have explained the variable cutaneous innervation patterns of the sural nerves, suggesting that the sural nerve may supply a wider area of skin than previously described.[18] Last, reports exist on the variable emergence of the infrapatellar branch of the saphenous nerve that arises distal to the adductor canal, which may pose complications during surgical interventions involving the anteromedial aspect of the knee.[19]
Surgical Considerations
Surgical approaches involving lower limb structures require meticulous care and emphasize understanding anatomical landmarks to prevent iatrogenic damage to the nerves that supply the foot. One of the most commonly reported complications of an anterior approach of a total ankle arthroplasty is an injury to the superficial fibular nerve and its aberrant branches, especially the intermediate dorsal cutaneous nerve. It is therefore recommended to visualize the nerve and mark its course preoperatively to avoid iatrogenic damage.[8] One report identified a reference line extending from the intermalleolar line and the line from the fifth metatarsal bone to the highest point of the Lisfranc line as easily identifiable bony landmarks when investigating the distal course of the superficial fibular nerve along the ankle.[20] Other surgeries that increase the risk of injury to the superficial fibular nerve include repair of a lateral malleolus fracture or surgical procedures that require an approach towards the lateral malleolus.[21]
Another study presented a case of deep fibular nerve injury secondary to ankle external fixator replacement surgery. If divided into four zones, the tibia may be used to assess the extent this nerve injury. The deep fibular nerve is at highest risk of injury in the zones where the nerve lies on the interosseous membrane while present at the posterior edge of the lateral tibia (zone 2) or where the nerve moves away from the membrane but lies directly in contact with the tibia (zone 3) when placing an external fixator.[9]
The lateral plantar nerve may be at more risk for injury than the medial plantar nerve when performing a calcaneal osteotomy through a lateral approach in the treatment of valgus deformity of the hindfoot. This risk exists because the lateral plantar nerve and its branches more commonly cross over the osteotomy site compared to the medial plantar nerve, which does not present at the osteotomy site. Thus, recommendations are that performing osteotomies through the medial calcaneal cortex be undertaken in a carefully controlled manner.[22]
Sural nerve injury may be present during laser surgery, lesser saphenous vein harvest, or posterolateral ankle surgery involving the Achilles tendon, the peroneal tendon, or even the lateral malleolus.[4][21] Its bony landmarks can be identified in the ankle using a reference line that includes the line from the lateral malleolus to the upper border of the calcaneus and the line from the fifth metatarsal bone to the highest point of the Lisfranc line.[20] Because of the variability in the anatomy of the sural nerve, it is recommended to use an ultrasound study to locate it accurately, thus preventing iatrogenic injury to the nerve.[23]
Last, saphenous nerve injuries commonly occur with use of an anteromedial portal for ankle arthroscopy, variceal surgeries, or during saphenous vein harvests.[4][24] In the case of saphenous vein harvests, the most vulnerable area susceptible to saphenous nerve injury is the inferior third of the leg because of venonervous adhesions.[24] Its bony landmarks can be identified in the ankle using a reference line starting from the line from the medial malleolus to the head of the talus.[20]
Clinical Significance
Neuropathies of the ankle and foot are uncommon and often underdiagnosed. Neuropathies may arise from metabolic processes, such as diabetes or alcohol abuse, or as a result of nerve compression syndromes.[25] The most frequent entrapment syndromes in decreasing order involve the digital nerves, Baxter's nerve, isolated medial or lateral plantar nerves, posterior tibial nerve, deep fibular nerve, superficial fibular nerve, sural nerve, and saphenous nerve.[26] Physicians must rely on performing a comprehensive physical examination and have a thorough knowledge of peripheral nerve anatomy to establish an accurate diagnosis as anatomical variations of the foot nerves may produce a spectrum of symptoms and diagnostic findings. Anatomical studies such as roentgenograms, advanced imaging studies, and electrodiagnostic tests help to identify the entrapped nerve. Roentgenograms may reveal bony abnormalities that contribute to the diagnosis. Advanced imaging studies, including MRI or ultrasound, help to localize specific areas of nerve entrapment. Electrodiagnostic tests, such as nerve conduction velocity studies, however, may be normal as these cases often resolve with rest.[26][27]
- Morton's neuroma (digital nerve entrapment):
- Morton's neuroma is a non-neoplastic lesion comprising degenerative changes and perineural fibrosis that impinges the digital nerve at the third web space on the plantar aspect of the foot because of entrapment from the intermetatarsal ligament or compression from the metatarsal heads and/or tissues surrounding the metatarsophalangeal joints. Women are more affected by this nerve entrapment than men most likely because of the availability of narrow-toe box shoes that externally compress the forefoot. Symptoms include burning or electric pain and paresthesias in the affected web space. Physical examination reveals a positive Mulder sign (i.e., reproducible pain and presence of a clicking sensation when squeezing two metatarsal heads together).[27]
- Baxter's neuropathy (lateral calcaneal nerve entrapment):
- Entrapment of the lateral calcaneal nerve typically occurs between the fascia of the abductor hallucis and the quadratus plantae muscles, but may also occur between the flexor digitorum brevis muscle and the calcaneus. Some primary causes for this entrapment include stretching of the nerve in athletes, muscle hypertrophy, bone spurs, and bursitis and inflammation of the plantar fascia. Baxter’s neuropathy presents as chronic medial plantar heel pain that worsens with activity and foot eversion and abduction. It is not usually associated with any paresthesias or weakness. Physical examination shows tenderness upon deep palpation of the abductor hallucis muscle.[27]
- Jogger’s Foot (medial plantar nerve compression):
- The medial plantar nerve may experience compression between the abductor hallucis fascia and its origin at the navicular and calcaneus, between the abductor hallucis muscle belly and the knot of Henry, or as it passes through the medial intermuscular septum. Long-distance runners with valgus hindfeet deformity may be more susceptible to jogger’s foot. Symptoms include exercise-induced pain over the medial plantar surface of the foot that radiates distally to first through third toes (on the plantar surface) and proximally into the medial heel and ankle. Physical examination findings reveal a positive Tinel sign at the plantar border of the navicular tuberosity and dysesthesia along the heel, medial arch, and first through third toes.[27]
- Tarsal tunnel syndrome (tibial nerve compression):
- Tarsal tunnel syndrome involves entrapment of the tibial nerve as it passes posterior to the medial malleolus and medial to the talus and calcaneus. This compression may divide into two syndromes: proximal compression of the tibial nerve or distal compression of its terminal branches (i.e., medial plantar nerve, lateral plantar nerve, and medial calcaneal nerve). Because the tibial nerve more commonly branches within the tarsal tunnel, distal compression syndromes present more often from either tarsal tunnel proper compression or distal entrapments outside the tarsal tunnel. Conversely. space-occupying lesions within the tarsal tunnel may cause proximal compression of the tibial nerve, such as tenosynovitis, ganglion, lipoma, venous engorgement, neurilemmoma, exostosis, or accessory muscles. Other causes of proximal compression include osseous or cartilaginous deformities, trauma, flexor retinaculum thickening, or even significant hindfoot pronation causing excessive tension on the tibial nerve. Symptoms of proximal compression include diffuse pain along the medial ankle and plantar foot (typically at night) that may worsen with activity, burning, shooting, and tingling sensations in the distribution of the tibial nerve proximally into the calf or distally into the foot, and even intermittent numbness of the plantar foot. Physical exam findings reveal a positive Tinel sign and reproducible pain with deep palpation of the tarsal tunnel or with foot dorsiflexion and eversion.[27]
- Anterior tarsal syndrome (deep fibular nerve compression):
- Compression of the deep fibular nerve and its branches may occur as it passes through the anterior tarsal tunnel, defined by the inferior extensor retinaculum superficially and the talonavicular joint capsule deeply. Compression of the lateral branch of the deep fibular nerve causes dorsal foot pain radiating to the region of the lateral tarsometatarsal joints whereas compression of the medial branch causes pain and/or numbness of the first web space on the dorsum of the foot.[27]
- Superficial fibular nerve entrapment:
- This nerve entrapment is a rare cause of chronic leg pain. As the superficial fibular nerve pierces the deep fascia of the leg to enter the foot, it may become entrapped by a thickened fascial tunnel, a fascial defect and muscle herniation, or a soft-tissue mass (e.g., lipoma). Athletes with lateral ligament deficiency or functional ankle instability may also experience this nerve entrapment as both conditions may cause traction injury to the superficial fibular nerve. Symptoms of this form of nerve entrapment include activity-related pain to the lower lateral leg and dysesthesia in the dorsum and lateral aspect of the foot. These symptoms may worsen with ankle inversion and plantar flexion and nerve percussion where it emerges from the deep fascia.[27]
- Sural nerve entrapment:
- This is a rare form of entrapment that may be caused by trauma, surgery, bony overgrowth, soft-tissue scarring, or instability. Although rare, sural nerve entrapment may occur in different locations along the leg, ankle, or foot. The most common sites of entrapment include the lateral border of the ankle, the calcaneus, and the fifth metatarsal. Patients with sural nerve entrapment report pain, numbness, or burning sensation at the posterolateral leg, lateral ankle, or lateral foot. Physical examination often reveals a positive Tinel sign and exacerbation of symptoms with plantar flexion and foot inversion.[27]
- Saphenous nerve entrapment:
- This is a rare form of entrapment that is diagnosed clinically and presents with pain and paresthesias to the medial foot and ankle. Proximal entrapment of the saphenous nerve is a more common presentation, whereas distal entrapment is less common and frequently associated with trauma or surgery. Nerve conduction velocity studies may be used to rule out more proximal impingement at the femoral nerve or the lumbar nerve roots.[27]
In most cases, these entrapment neuropathies resolve with rest, NSAIDs, and occasional steroid injections. Removal of any external compressive factors, inflammation and edema reduction, and correction of any deformities or osseous abnormalities are also effective. Recalcitrant cases may require surgical decompression and release of any tissues compressing the affected nerve, which have frequently provided satisfactory results.[26][27]