[1]
Beer JI, Sieber DA, Scheuer JF 3rd, Greco TM. Three-dimensional Facial Anatomy: Structure and Function as It Relates to Injectable Neuromodulators and Soft Tissue Fillers. Plastic and reconstructive surgery. Global open. 2016 Dec:4(12 Suppl Anatomy and Safety in Cosmetic Medicine: Cosmetic Bootcamp):e1175. doi: 10.1097/GOX.0000000000001175. Epub 2016 Dec 14
[PubMed PMID: 28018776]
[2]
Westbrook KE, Nessel TA, Hohman MH, Varacallo M. Anatomy, Head and Neck: Facial Muscles. StatPearls. 2023 Jan:():
[PubMed PMID: 29630261]
[3]
Frisdal A, Trainor PA. Development and evolution of the pharyngeal apparatus. Wiley interdisciplinary reviews. Developmental biology. 2014 Nov-Dec:3(6):403-18. doi: 10.1002/wdev.147. Epub 2014 Aug 29
[PubMed PMID: 25176500]
[4]
Blumenfeld AM, Silberstein SD, Dodick DW, Aurora SK, Brin MF, Binder WJ. Insights into the Functional Anatomy Behind the PREEMPT Injection Paradigm: Guidance on Achieving Optimal Outcomes. Headache. 2017 May:57(5):766-777. doi: 10.1111/head.13074. Epub 2017 Apr 6
[PubMed PMID: 28387038]
[5]
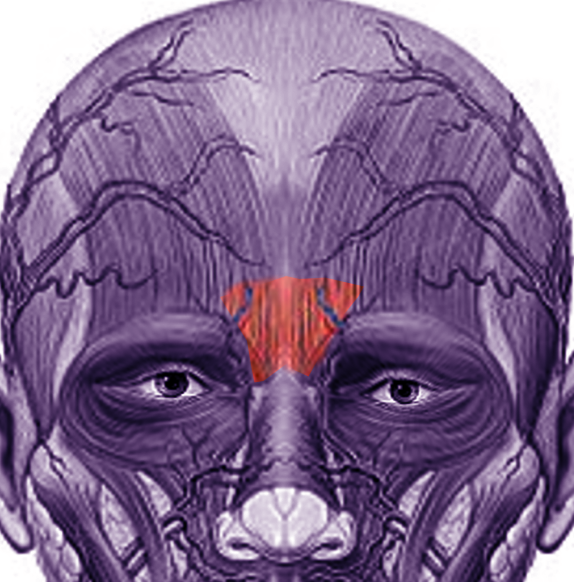
Caminer DM, Newman MI, Boyd JB. Angular nerve: new insights on innervation of the corrugator supercilii and procerus muscles. Journal of plastic, reconstructive & aesthetic surgery : JPRAS. 2006:59(4):366-72
[PubMed PMID: 16756251]
[6]
Glaich AS, Cohen JL, Goldberg LH. Injection necrosis of the glabella: protocol for prevention and treatment after use of dermal fillers. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2006 Feb:32(2):276-81
[PubMed PMID: 16442055]
[7]
Foustanos A. Suture fixation technique for endoscopic brow lift. Seminars in plastic surgery. 2008 Feb:22(1):43-9. doi: 10.1055/s-2007-1019142. Epub
[PubMed PMID: 20567688]
[8]
Levaillant JM, Touboul C, Sinico M, Vergnaud A, Serero S, Druart L, Blondeau JR, Abd Alsamad I, Haddad B, Gérard-Blanluet M. Prenatal forehead edema in 4p- deletion: the 'Greek warrior helmet' profile revisited. Prenatal diagnosis. 2005 Dec:25(12):1150-5
[PubMed PMID: 16258951]
[9]
Adam MP, Mirzaa GM, Pagon RA, Wallace SE, Bean LJH, Gripp KW, Amemiya A, Battaglia A, Carey JC, South ST. Wolf-Hirschhorn Syndrome – RETIRED CHAPTER, FOR HISTORICAL REFERENCE ONLY. GeneReviews(®). 1993:():
[PubMed PMID: 20301362]
[10]
Bhattacharjee S. Procerus Sign: Mechanism, Clinical Usefulness, and Controversies. Annals of Indian Academy of Neurology. 2018 Apr-Jun:21(2):164-165. doi: 10.4103/aian.AIAN_408_17. Epub
[PubMed PMID: 30122846]
[11]
Fekete R, Jankovic J. Upper facial chorea in Huntington disease. Journal of clinical movement disorders. 2014:1():7. doi: 10.1186/2054-7072-1-7. Epub 2014 Nov 20
[PubMed PMID: 26788333]
[12]
Batla A, Nehru R, Vijay T. Vertical wrinkling of the forehead or Procerus sign in Progressive Supranuclear Palsy. Journal of the neurological sciences. 2010 Nov 15:298(1-2):148-9. doi: 10.1016/j.jns.2010.08.010. Epub 2010 Sep 1
[PubMed PMID: 20810128]