[1]
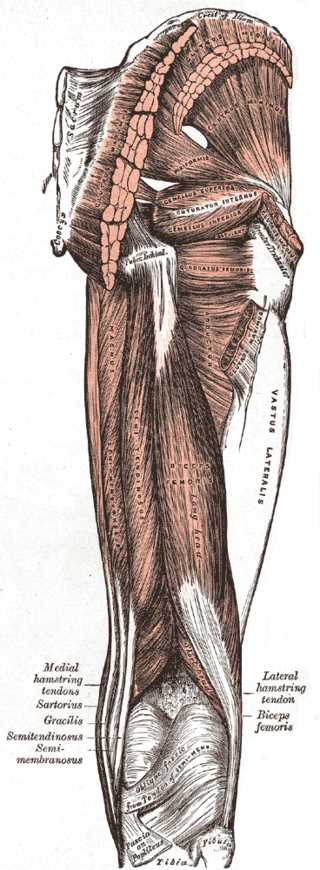
Woodley SJ, Mercer SR. Hamstring muscles: architecture and innervation. Cells, tissues, organs. 2005:179(3):125-41
[PubMed PMID: 15947463]
[2]
Greenwood K, Zyl RV, Keough N, Hohmann E. Defining the popliteal fossa by bony landmarks and mapping of the courses of the neurovascular structures for application in popliteal fossa surgery. Anatomy & cell biology. 2021 Mar 31:54(1):10-17. doi: 10.5115/acb.20.179. Epub
[PubMed PMID: 33594009]
[3]
Koulouris G, Connell D. Hamstring muscle complex: an imaging review. Radiographics : a review publication of the Radiological Society of North America, Inc. 2005 May-Jun:25(3):571-86
[PubMed PMID: 15888610]
[4]
van der Made AD, Wieldraaijer T, Kerkhoffs GM, Kleipool RP, Engebretsen L, van Dijk CN, Golanó P. The hamstring muscle complex. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2015 Jul:23(7):2115-22. doi: 10.1007/s00167-013-2744-0. Epub 2013 Nov 5
[PubMed PMID: 24190369]
[5]
Buckingham M, Bajard L, Chang T, Daubas P, Hadchouel J, Meilhac S, Montarras D, Rocancourt D, Relaix F. The formation of skeletal muscle: from somite to limb. Journal of anatomy. 2003 Jan:202(1):59-68
[PubMed PMID: 12587921]
[6]
Tickle C. How the embryo makes a limb: determination, polarity and identity. Journal of anatomy. 2015 Oct:227(4):418-30. doi: 10.1111/joa.12361. Epub 2015 Aug 7
[PubMed PMID: 26249743]
[7]
Tickle C, Barker H. The Sonic hedgehog gradient in the developing limb. Wiley interdisciplinary reviews. Developmental biology. 2013 Mar-Apr:2(2):275-90. doi: 10.1002/wdev.70. Epub 2012 May 25
[PubMed PMID: 24009037]
[8]
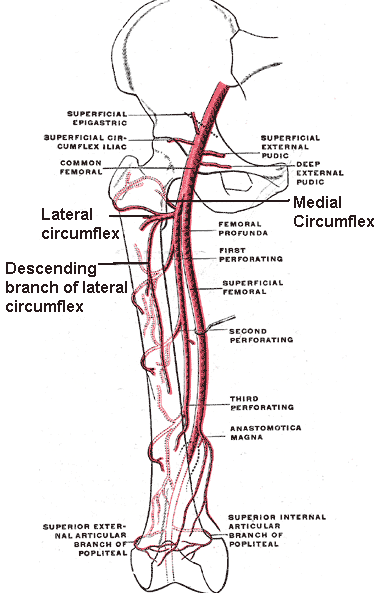
Tomaszewski KA, Henry BM, Vikse J, Pękala P, Roy J, Svensen M, Guay D, Hsieh WC, Loukas M, Walocha JA. Variations in the origin of the deep femoral artery: A meta-analysis. Clinical anatomy (New York, N.Y.). 2017 Jan:30(1):106-113. doi: 10.1002/ca.22691. Epub 2016 Feb 2
[PubMed PMID: 26780216]
Level 1 (high-level) evidence
[9]
Choy KW, Kogilavani S, Norshalizah M, Rani S, Aspalilah A, Hamzi H, Farihah HS, Das S. Topographical anatomy of the profunda femoris artery and the femoral nerve: normal and abnormal relationships. La Clinica terapeutica. 2013:164(1):17-9. doi: 10.7417/T.2013.1504. Epub
[PubMed PMID: 23455736]
[10]
Tomaszewski KA, Graves MJ, Henry BM, Popieluszko P, Roy J, Pękala PA, Hsieh WC, Vikse J, Walocha JA. Surgical anatomy of the sciatic nerve: A meta-analysis. Journal of orthopaedic research : official publication of the Orthopaedic Research Society. 2016 Oct:34(10):1820-1827. doi: 10.1002/jor.23186. Epub 2016 Feb 22
[PubMed PMID: 26856540]
Level 1 (high-level) evidence
[11]
Chakravarthi K. Unusual unilateral multiple muscular variations of back of thigh. Annals of medical and health sciences research. 2013 Nov:3(Suppl 1):S1-2. doi: 10.4103/2141-9248.121206. Epub
[PubMed PMID: 24349835]
[12]
Sussmann AR. Congenital bilateral absence of the semimembranosus muscles. Skeletal radiology. 2019 Oct:48(10):1651-1655. doi: 10.1007/s00256-019-03210-3. Epub 2019 Apr 15
[PubMed PMID: 30982941]
[13]
Park JH, Park KR, Yang J, Park GH, Cho J. Unusual variant of distal biceps femoris muscle associated with common peroneal entrapment neuropathy: A cadaveric case report. Medicine. 2018 Sep:97(38):e12274. doi: 10.1097/MD.0000000000012274. Epub
[PubMed PMID: 30235672]
Level 3 (low-level) evidence
[14]
Lempainen L, Banke IJ, Johansson K, Brucker PU, Sarimo J, Orava S, Imhoff AB. Clinical principles in the management of hamstring injuries. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2015 Aug:23(8):2449-2456. doi: 10.1007/s00167-014-2912-x. Epub 2014 Feb 21
[PubMed PMID: 24556933]
[15]
Folsom GJ, Larson CM. Surgical treatment of acute versus chronic complete proximal hamstring ruptures: results of a new allograft technique for chronic reconstructions. The American journal of sports medicine. 2008 Jan:36(1):104-9
[PubMed PMID: 18055919]
[16]
Liu H, Zhang Y, Rang M, Li Q, Jiang Z, Xia J, Zhang M, Gu X, Zhao C. Avulsion Fractures of the Ischial Tuberosity: Progress of Injury, Mechanism, Clinical Manifestations, Imaging Examination, Diagnosis and Differential Diagnosis and Treatment. Medical science monitor : international medical journal of experimental and clinical research. 2018 Dec 27:24():9406-9412. doi: 10.12659/MSM.913799. Epub 2018 Dec 27
[PubMed PMID: 30589058]
[18]
Gidwani S, Jagiello J, Bircher M. Avulsion fracture of the ischial tuberosity in adolescents--an easily missed diagnosis. BMJ (Clinical research ed.). 2004 Jul 10:329(7457):99-100
[PubMed PMID: 15242916]
[19]
Frank RM, Hamamoto JT, Bernardoni E, Cvetanovich G, Bach BR Jr, Verma NN, Bush-Joseph CA. ACL Reconstruction Basics: Quadruple (4-Strand) Hamstring Autograft Harvest. Arthroscopy techniques. 2017 Aug:6(4):e1309-e1313. doi: 10.1016/j.eats.2017.05.024. Epub 2017 Aug 14
[PubMed PMID: 29354434]
[20]
Goldblatt JP, Fitzsimmons SE, Balk E, Richmond JC. Reconstruction of the anterior cruciate ligament: meta-analysis of patellar tendon versus hamstring tendon autograft. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2005 Jul:21(7):791-803
[PubMed PMID: 16012491]
Level 1 (high-level) evidence
[21]
Kocher MS, Steadman JR, Briggs K, Zurakowski D, Sterett WI, Hawkins RJ. Determinants of patient satisfaction with outcome after anterior cruciate ligament reconstruction. The Journal of bone and joint surgery. American volume. 2002 Sep:84(9):1560-72
[PubMed PMID: 12208912]
[22]
Heiderscheit BC, Sherry MA, Silder A, Chumanov ES, Thelen DG. Hamstring strain injuries: recommendations for diagnosis, rehabilitation, and injury prevention. The Journal of orthopaedic and sports physical therapy. 2010 Feb:40(2):67-81. doi: 10.2519/jospt.2010.3047. Epub
[PubMed PMID: 20118524]
[23]
Askling CM, Tengvar M, Saartok T, Thorstensson A. Acute first-time hamstring strains during high-speed running: a longitudinal study including clinical and magnetic resonance imaging findings. The American journal of sports medicine. 2007 Feb:35(2):197-206
[PubMed PMID: 17170160]
[24]
Opar DA, Williams MD, Shield AJ. Hamstring strain injuries: factors that lead to injury and re-injury. Sports medicine (Auckland, N.Z.). 2012 Mar 1:42(3):209-26. doi: 10.2165/11594800-000000000-00000. Epub
[PubMed PMID: 22239734]
[25]
Hamilton B, Valle X, Rodas G, Til L, Grive RP, Rincon JA, Tol JL. Classification and grading of muscle injuries: a narrative review. British journal of sports medicine. 2015 Mar:49(5):306. doi: 10.1136/bjsports-2014-093551. Epub 2014 Nov 13
[PubMed PMID: 25394420]
Level 3 (low-level) evidence
[26]
Brukner P. Hamstring injuries: prevention and treatment-an update. British journal of sports medicine. 2015 Oct:49(19):1241-4. doi: 10.1136/bjsports-2014-094427. Epub 2015 Jun 23
[PubMed PMID: 26105015]
[27]
Järvinen MJ, Lehto MU. The effects of early mobilisation and immobilisation on the healing process following muscle injuries. Sports medicine (Auckland, N.Z.). 1993 Feb:15(2):78-89
[PubMed PMID: 8446826]
[28]
Reynolds JF, Noakes TD, Schwellnus MP, Windt A, Bowerbank P. Non-steroidal anti-inflammatory drugs fail to enhance healing of acute hamstring injuries treated with physiotherapy. South African medical journal = Suid-Afrikaanse tydskrif vir geneeskunde. 1995 Jun:85(6):517-22
[PubMed PMID: 7652633]
[29]
Mishra DK, Fridén J, Schmitz MC, Lieber RL. Anti-inflammatory medication after muscle injury. A treatment resulting in short-term improvement but subsequent loss of muscle function. The Journal of bone and joint surgery. American volume. 1995 Oct:77(10):1510-9
[PubMed PMID: 7593059]
[30]
Engebretsen L, Steffen K, Alsousou J, Anitua E, Bachl N, Devilee R, Everts P, Hamilton B, Huard J, Jenoure P, Kelberine F, Kon E, Maffulli N, Matheson G, Mei-Dan O, Menetrey J, Philippon M, Randelli P, Schamasch P, Schwellnus M, Vernec A, Verrall G. IOC consensus paper on the use of platelet-rich plasma in sports medicine. British journal of sports medicine. 2010 Dec:44(15):1072-81. doi: 10.1136/bjsm.2010.079822. Epub
[PubMed PMID: 21106774]
Level 3 (low-level) evidence
[31]
Kraiem Z, Alkobi R, Sadeh O. Sensitization and desensitization of human thyroid cells in culture: effects of thyrotrophin and thyroid-stimulating immunoglobulin. The Journal of endocrinology. 1988 Nov:119(2):341-9
[PubMed PMID: 2462004]
[32]
Brooks JH, Fuller CW, Kemp SP, Reddin DB. Incidence, risk, and prevention of hamstring muscle injuries in professional rugby union. The American journal of sports medicine. 2006 Aug:34(8):1297-306
[PubMed PMID: 16493170]
[33]
Sherry MA, Best TM. A comparison of 2 rehabilitation programs in the treatment of acute hamstring strains. The Journal of orthopaedic and sports physical therapy. 2004 Mar:34(3):116-25
[PubMed PMID: 15089024]