Continuing Education Activity
The radial nerve stems from the posterior cord of the brachial plexus and supplies the upper limb. It also supplies the triceps brachii muscle of the arm, the muscles in the posterior compartment of the forearm (also known as the extensors), the wrist joint capsule, and aspects of the dorsal skin of the forearm and hand. This activity reviews the cause, presentation, diagnosis, and pathophysiology of radial nerve injury and highlights the interprofessional team's role in its management.
Objectives:
- Identify the etiology of radial nerve injury.
- Review the physical exam of a patient with radial nerve injury.
- Outline the management options available for radial nerve injury.
- Explain interprofessional team strategies for improving care and outcomes in patients with radial nerve injury.
Introduction
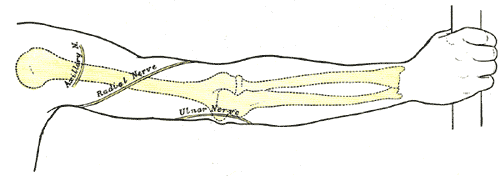
The radial nerve stems from the posterior cord of the brachial plexus and supplies the upper limb. It also supplies the triceps brachii muscle of the arm, the muscles in the posterior compartment of the forearm (also known as the extensors), the wrist joint capsule, and aspects of the dorsal skin of the forearm and hand. The radial nerve proper innervates[1]:
- Triceps
- Anconeus
- Extensor carpi radialis longus (ECRL)
- Extensor carpi radialis brevis (ECRB)
- Brachioradialis
The radial nerve divides into a deep (mostly motor) branch, which becomes the posterior interosseous nerve (PIN), and a superficial branch. The PIN innervates:
- Extensor digitorum
- Supinator muscle
- Extensor digiti minimi (EDM)
- Extensor carpi ulnaris (ECU)
- Abductor pollicis longus (APL)
- Extensor pollicis longus (EPL)
- Extensor pollicis brevis (EPB)
- Extensor indicis proprius (EIP)
Sensory innervation includes:
- Posterior cutaneous nerve (arm and forearm)
- Superficial branch radial nerve (SBRN)
- Dorsal digital branch
The following tests can quickly assess the radial nerve and its motor and sensory functions:
- Motor function: Thumb extension against resistance
- Sensory function: Two-point discrimination on the dorsum of the thumb
Nevertheless, a thorough physical exam is always required. Radial nerve injuries have distinct signs and symptoms depending on where and how the nerve has been injured.
Etiology
Radial nerve injuries can occur after trauma. Common forms of radial nerve injuries occur with the following:
- After fractures of the humerus, especially spiral fracture patterns along the distal third of the humerus (Holstein-Lewis fracture) with a known associated incidence of radial nerve neuropraxia in the range of 15% to 25%
- Improper use of crutches
- Overuse of the arm (secondary to manual labor, chronic overuse, or sport-related participation)
- Work-related accidents
Radial nerve injuries have distinct presentations and symptoms, depending on the anatomic location and type of injury occurring to the nerve. For example, injuring the radial nerve at the axilla has a different clinical presentation than injuring it at the distal forearm.
Epidemiology
Radial mononeuropathies are common, but the exact prevalence of radial nerve injuries causing such neuropathies is unknown. There are no generalized epidemiological studies reported in the literature at this time. Although there have been no recent studies, one study in the late 1980s showed that the radial nerve was the most commonly injured nerve in the upper extremity, although this is debatable.[2]
Pathophysiology
The nerve can be damaged with intensities ranging from Sunderland first to fifth degrees.[3]
History and Physical
A patient with radial neuropathy may present holding their affected extremity with the ipsilateral (normal) hand. He or she may complain of decreased or absent sensation on the dorsoradial side of their hand and wrist with an inability to extend their wrist, thumb, and fingers. With the hand supinated, and the extensors aided by gravity, hand function may appear normal. However, when the hand is pronated, the wrist and hand will drop. This is also referred to as "wrist drop.”
If damaged at the axilla, there will be a loss of extension of the forearm, hand, and fingers. Thus, this usually presents with a wrist drop on physical examination. There will be a sensory loss in the lateral arm. There will also be a sensory loss in the posterior aspect of the forearm, radiating to the radial aspect of the dorsal hand and digits. This is seen commonly with "Saturday night palsy" and improperly using crutches (crutch palsy). Any condition or clinical situation in which the patient has improperly created pathologic forces and/or compression in the axilla can potentially affect the radial nerve by way of the brachial plexus.
Injuring the radial nerve distal to the elbow joint can occur from:
- Elbow dislocations
- Elbow fractures
- Tight casts/compressive wraps
- Rheumatoid conditions/inflammatory arthritides
This causes weakness in the extension of the hand and fingers and the presence of finger drop and partial wrist drop.
Posterior interosseous nerve syndrome can also occur from damaging the radial nerve below the elbow. This branch provides motor innervation to the extensor compartment. It presents with pain in the forearm and wrist, along with weakness with finger metacarpal extension and wrist extension.[4]
Damaging the nerve at the distal forearm can occur from Wartenberg syndrome, which is an entrapment of the nerve between the brachioradialis and muscle (sometimes due to wearing tight jewelry and watches). There is usually numbness and tingling in the radial half of the dorsum of the hand and the dorsum of the radial 3 1/2 digits. However, motor function stays intact.
Evaluation
When there is a traumatic injury, radiographs are usually adequate. This is especially relevant after traumatic injuries such as fractures. Occasionally, when ruling out or investigating compressive neuropathies, advanced imaging such as magnetic resonance imaging (MRI) can further delineate pathological anatomic determinants.
Electromyograms or nerve conduction studies (EMG/NCS) can help differentiate nerve versus muscle injury, measuring the speed at which the impulses travel along the nerve. EMG/NCS is also utilized for follow-up management in serial observations for the return of nerve function. It is important to note that more than 90% of radial nerve palsies will resolve in 3 to 4 months with observation alone.
There was a recent study of rapid ultrasonographic diagnosis of radial entrapment neuropathy at the spiral groove. If available, this modality can be used for evaluation.[5]
The return of function following radial nerve palsy follows a predictable clinical pattern. Brachioradialis followed by ECRL are the first to return; whereas, EPL and EIP are the last to return.
Treatment / Management
Conservative treatment options depend on the severity of the injury and the patient's symptoms. They include:
- Analgesic medications, including oral or topical non-steroidal anti-inflammatory drugs (NSAIDs)
- Corticosteroid injections and steroids can help decrease any inflammation contributing to the process.
- Physical therapy
- Immobilization with proper splints for at least 2 to 4 weeks, or until the symptoms have resolved
Patients typically recover 4 months after starting treatment as long as the nerve is not lacerated or torn. The prognosis for patients with acute compressive radial nerve injuries is good.
Some radial nerve injuries end up requiring more aggressive management. If the radial nerve is entrapped and symptoms last for several months, surgery is indicated to relieve the pressure on the nerve. This should always be the last option for the patient.[1]
Differential Diagnosis
Sometimes, it is difficult to distinguish radial neuropathies from central nervous system (CNS) lesions, as they can both cause wrist extension weakness (wrist drop). To differentiate between a peripheral radial neuropathy from a central pathology, test the brachioradialis muscle. It is always weak in a peripheral radial nerve injury and less affected with a CNS disorder.[6]
Prognosis
The majority (up to 92%) resolve with observation alone for 3 to 4 months in the setting of injuries or fractures to the humerus.
Complications
Radial nerve injuries are usually treated with conservative modalities, such as physical therapy and splinting. If surgical intervention is required, there is a potential for post-surgical complications.[4] These complications include but are not limited to:
- Stretching of the nerve
- The severing of the nerve
- Incomplete release
- Muscle atrophy
Consultations
If needed, orthopedic surgeons or hand surgeons can be consulted for radial nerve injuries. Patients may also require a neurology consultation for further evaluation with electromyography or nerve conduction studies.
Deterrence and Patient Education
Patients should follow their individualized treatment plans for the best results. They should also follow up with their physicians regularly and appropriately. Physicians should, in turn, educate patients on the treatment options available and talk about prognosis and complications.
Pearls and Other Issues
- Younger patients tend to heal better.
- If radial nerve damage results from underlying comorbidity, such as diabetes mellitus and/or alcohol abuse, a proper lab workup is indicated.
- If surgery is required, a full recovery can take up to 8 months.
- Splints are usually worn for 2 to 4 weeks. Add protective padding for athletes who may be prone to repetitive forearm trauma.
Enhancing Healthcare Team Outcomes
Radial nerve injuries are usually treated conservatively and have a good prognosis if patients comply with their management plans. Primary care clinicians and nurse practitioners who do not regularly manage hand injuries should refer these patients to a neurologist, orthopedist, hand surgeon, or physical therapist for appropriate management. These kinds of interprofessional healthcare team activities will drive improved patient outcomes with radial nerve injuries. [Level 5]