Introduction
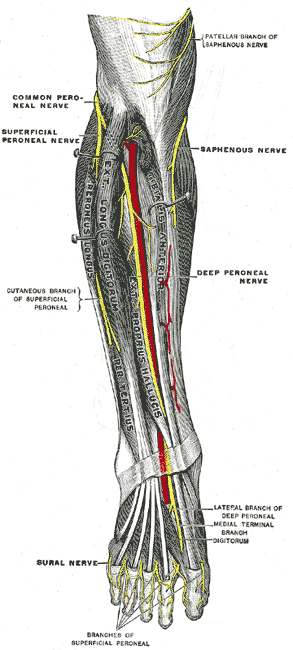
The common peroneal nerve, also known as the common fibular nerve, is a major nerve that innervates the lower extremity (see Image. The Sacral and Coccygeal Nerve). As one of the two major branches off the sciatic nerve, it receives fibers from the posterior divisions of L4 through S2. Specifically, it originates from the sciatic nerve and separates from it proximal to the popliteal fossa, and courses its way along the posterolateral aspect of the leg deep to the long head of the biceps femoris and through the popliteal fossa before passing behind the proximal fibular head. Just inferior and lateral to the fibular head, it divides into two nerves at the fibular neck–the superficial and deep fibular nerves. The superficial fibular nerve courses anterolaterally between the fibularis longus muscle and extensor digitorum longus muscle within the lateral compartment.
As it moves distally, it terminates within the lateral compartment before reaching the ankle and foot. The deep fibular nerve courses anteriorly and runs adjacent to the anterior tibial artery between the extensor digitorum longus muscle and the tibialis anterior muscle. As the deep fibular nerve travels distally, it runs within the anterior compartment of the leg between two muscles. These muscles include the extensor hallucis longus muscle and the tibialis anterior muscle. As the nerve approaches the foot just anterior to the talus, it divides into medial and lateral branches. The medial branch travels alongside the dorsalis pedis artery and terminates in between the first two metatarsals. The lateral branch travels alongside the lateral tarsal artery and terminates near the fifth metatarsal.[1]
Structure and Function
The common fibular nerve is ultimately responsible for innervating the muscles that compose the anterior and lateral muscular compartments of the lower extremity. The anterior muscular compartment of the lower extremity consists of the tibialis anterior muscle, the extensor hallucis longus muscle, and the extensor digitorum longus muscle. This compartment is responsible primarily for the dorsiflexion of the foot.[2] The lateral muscular compartment of the lower extremity consists of the fibularis longus muscle and the fibularis brevis muscle. This compartment is responsible primarily for the eversion of the foot.
In addition to carrying motor fibers, the common fibular nerve carries afferent cutaneous sensory fibers from the lower extremity that ultimately travel proximally to the spinal cord. The majority of anterior sensation of the leg is carried by the superficial fibular nerve; however, the deep fibular nerve carries some as well. Specifically, the superficial fibular nerve carries sensory fibers from the anterolateral aspect of the lower extremity that extends from midway down the leg to the majority of the dorsal aspect of the foot and toes. The deep fibular nerve carries sensory fibers from between the first and second toes. These nerves also carry some posterolateral sensation, albeit minimal. The common fibular nerve is responsible for sensation inferolaterally to the knee via the lateral sural cutaneous nerve, which is a small cutaneous branch off the common fibular nerve. The superficial fibular nerve is responsible for some lateral leg sensation just below where the sensation from the lateral sural cutaneous nerve ends.[1]
Physiologic Variants
As in most parts of the human anatomy, the course and surrounding anatomy of the common fibular nerve has several variants that should be noted, especially for surgeons who may have to decompress the nerve. These variants may also result in an increase or decrease in the likelihood of compressed nerves.[3] In a study comparing the anatomy in cadavers and the anatomy in surgically decompressed nerves, there were found to be a few major variants. The first one includes fibrous tissue that forms a band-like structure underneath the superficial head of the peroneus longus. The next variant also includes fibrous tissue forming a band-like structure; however, this tissue is located on the superficial surface of the deep head of a muscle known as the peroneus longus. The last variant noted includes two muscles and their uncommon junction and origin. Usually, the soleus muscle and the fibularis longus muscle originate separately on the fibular head; however, in some people, they originate together at the fibular head and separate as they move distally.[4]
Clinical Significance
The common fibular nerve is a frequently discussed subject compared to other neuromuscular complaints due to its frequent injury and its classic clinical presentation. Because of its location, it is fairly vulnerable to damage. It travels across the lateral aspect of the knee over the neck of the fibula, where its only protection is skin and subcutaneous fat and fascia. Thus, various trauma to the lateral knee often results in damage to the common fibular nerve. For example, if a football player is tackled from the side, the result may be a fibular neck fracture and common fibular nerve injury.[5] The patient would most likely present with knee pain, loss of foot dorsiflexion, loss of ankle eversion, and loss of sensation down the lateral leg and dorsum of the foot. Because of the patient’s inability to dorsiflex the foot, they will also likely present with “foot drop.” This condition occurs during the swinging phase of the gait cycle. Because there is a loss of dorsiflexion, the toes will drag on the ground rather than clear the ground as in a normal gait. In many cases, the patient will compensate for their foot-dragging by exaggerating hip abduction to allow for increased clearance of their foot.[6][7]
Another frequent mechanism of injury to the common fibular nerve is through compression of the nerve as it crosses the fibular head and neck or distal to them. This may occur after a splint or cast is placed incorrectly or too tight, or in the case of compartment syndrome after a trauma or burn. These examples would present similarly: the compressed nerve would initially cause paresthesias, followed by loss of sensation and weakness and ultimately resulting in loss of dorsiflexion of the foot and loss of ankle eversion if left untreated. It should be noted that in these cases, there might also be a vascular compromise, so distal pulses should be examined.[2]
There are also clinical presentations that may mimic an injury to the common fibular nerve but are actually due to proximal injuries at the level of the sciatic nerve. One common example is in the case of piriformis syndrome. In some cases or anatomical variants, the sciatic nerve, which carries fibers for the common fibular nerve, may become entrapped within the piriformis muscle. A tight piriformis may then cause similar symptoms to the classic common fibular nerve injury: loss of dorsiflexion, loss of foot eversion, and loss of sensation to the anterolateral aspect of the leg and dorsum of the foot. However, in addition to these symptoms, the patient might also experience symptoms proximal to the knee similar to the classic presentation of sciatica. Thus, it is essential to differentiate between sciatica, piriformis syndrome, or just simply an injury to the common fibular nerve in order to formulate a proper treatment plan.[8]