Introduction
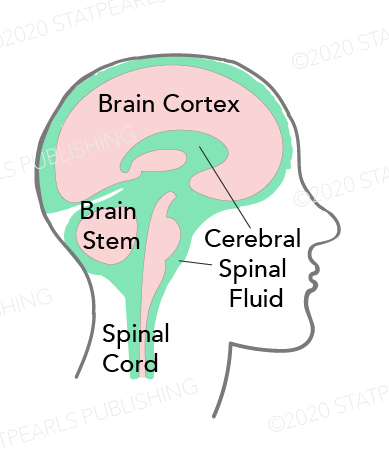
Cerebrospinal fluid (CSF) is a clear, plasma-like fluid that bathes the central nervous system (CNS). It occupies the central spinal canal, the ventricular system, and the subarachnoid space. It is produced mostly by the choroidal plexus of the ventricular system as well as its ependymal lining. The CSF has a physiologic volume of about 150 ml with a daily turnover of about 500 ml. Produced mostly in the lateral ventricles, the CSF passes through the interventricular foramen (of Monro), into the third ventricle. It exits the third ventricle through the cerebral aqueduct (of Sylvius) into the fourth ventricle. It exits the fourth ventricle into the cerebral subarachnoid space through the median aperture of Magendie and the two lateral apertures of Luschka. The CSF continues into the spinal subarachnoid space through the central canal of the spinal cord.[1][2][3]
Normal CSF pressure (8 mmHg to 15 mmHg supine and about 20 mmHg erect) is a function of a tightly maintained equilibrium in rates of production and resorption of CSF. The out-pouching of the arachnoid mater called arachnoid granulations are responsible for the resorption of CSF into the dural venous sinuses. Disequilibrium in synthesis and resorption or obstruction of circulation results in CSF accumulation and raised intracranial pressure called hydrocephalus.
Structure and Function
Support
The CSF supports the weight of the brain estimated at 1500 gm and suspends it in neutral buoyancy to a net weight of about 25 gm. Hence, the entire brain density is cushioned, protecting it from crushing into the bony cranium.
Shock absorber
It protects the brain from damage during head trauma. Otherwise, even minor head-bopping will result in severe brain injury.
Homeostasis
The biochemical constituents and volume of the CSF play vital cerebral homeostatic roles:
- Maintains stable intrinsic CNS temperature
- Biochemical constituents and electrolytes maintain the osmotic pressure responsible for normal CSF pressure which is essential to maintaining normal cerebral perfusion
- Biochemical waste products diffuse into the CSF and are removed as CSF is resorbed through arachnoid granulations into the venous circulation, a small percentage of CSF also drains into lymphatic circulation.
Nutrition
The CSF contains glucose, proteins, lipids, and electrolytes, providing essential CNS nutrition.
Immune function
The CSF contains immunoglobulins and mononuclear cells.
Embryology
At the beginning of week 4, before the formation of choroid plexus, the neural tube is found with CSF; this suggests extra-choroidal sources of CSF during embryonic development.
The choroid plexus became visible at around week 6 (about day 40), the arachnoid granulations did not form until the third trimester and up until around the 20th month of life.
Congenital hydrocephalus develops during intrauterine life, common developmental defects implicated are aqueductal stenosis and neural tube defects.
Blood Supply and Lymphatics
The choroid plexus refers to a group of fenestrated blood capillaries located in the ventricular system. The choroid plexus mostly synthesizes CSF.
Arachnoid granulations are responsible for CSF resorption; they drain CSF into the dural venous sinuses.
CSF drains into the lymphatic circulation, through lymph ducts contiguous to the olfactory duct as it passes through the cribriform plate.
Surgical Considerations
Hydrocephalus
This is a condition in which CSF accumulates in the CNS due to a dis-equilibrium between synthesis, circulation, and resorption of CSF.
It may be classified based on etiology or mechanism.[4][5][6]
Etiology:
- Congenital: this develops in-utero, a common cause is an aqueductal stenosis. It is usually associated with other congenital disabilities like neural tube defects, Arnold-Chiari malformation, and Dandy-Walker syndrome.
- Acquired: This may result from a cerebral infection like meningitis or a space-occupying lesion/tumor, for example, ependymoma or toxoplasmosis.
Mechanism:
- Communicating: also called non-obstructive hydrocephalus, this results because the rate of CSF production exceeds the rate of resorption. Causes include ependymoma, arachnoid granulation inflammation due to meningitis.
- Non-communicating: also called obstructive hydrocephalus, results from an obstruction in the ventricular system either acquired or congenital.
Treatment:
- Ventriculostomy: also called external ventricular drain (EVD), drains away excess CSF using a ventricular catheter to provide immediate relief
- Ventricular shunting: drains excess CSF into existing body compartments. Examples are a ventriculoperitoneal shunt, ventriculoatrial shunt, or ventricular-pleural shunt.
- The lumbar-peritoneal shunt drains excess CSF from the spinal subarachnoid space into the peritoneum.
- Endoscopic third ventriculostomy is a recent surgical approach, often done with cauterization of the choroid plexus.
Shunt failure
This may complicate a shunt surgery with a re-occurrence of presenting symptoms necessitating a shunt revision. Common causes of shunt failure are infections, blocked shunt, or a displaced shunt.
Clinical Significance
Lumbar Puncture and CSF Analysis
Lumbar puncture is a sterile procedure, done to obtain CSF samples for diagnostic purposes. It involves passing a needle into the subarachnoid space at the levels between L2 and L5 vertebrae. However, most commonly lumbar puncture is performed between L4 and L5. Biochemical, microbiologic, and cytologic studies are carried out, some possible pathognomic pictures in comparison to physiologic CSF parameters are as follows:
Normal CSF
- Color: clear or colorless
- CSF Pressure: 8 mmHg to 15 mmHg
- Glucose: 50 mg/dl to 80 mg/dl or two-thirds of blood glucose level
- Protein: 15 mg/dl to 45 mg/dl
- Mononuclear cells: 0 to 5/mm3
- Bacterial Meningitis: Grossly cloudy or purulent, elevated CSF protein, low CSF glucose, elevated CSF lactate, and markedly elevated neutrophils
- Viral Meningitis[7]: Grossly clear CSF, Normal or slightly low glucose, moderately elevated protein, and markedly elevated lymphocyte levels
- Tuberculous Meningitis: Grossly yellowish and viscous CSF, low glucose, markedly elevated protein, normal or slightly elevated neutrophils, moderately elevated lymphocytes
- Subarachnoid Hemorrhage[8]: Lumbar puncture may be used to diagnose a subarachnoid hemorrhage about 12 hours after onset of a debilitating occipital headache usually when brain CT scan returns negative. The CSF studies showing a red cell count of more than 100/mm3 and grossly yellowish CSF termed "xanthochromia" due to CSF bilirubin, which may be confirmed via CSF spectrophotometry is strongly suggestive of subarachnoid hemorrhage.
Subarachnoid Block[9]
Also called a spinal block, is a method of regional anesthesia. It involves the injection of a local anesthetic agent into the subarachnoid space through a needle at the level between L2 and L5 vertebrae.
Intrathecal Administration
Specially formulated drugs were administered intrathecally into the CSF to assess the blood-brain barrier. Cancer chemotherapeutic agents like methotrexate are available in intrathecal formulations as well as intrathecal opioids using an intrathecal pump or catheter.
Other Issues
Normal Pressure Hydrocephalus[10]
Increased CSF with concomitant ventriculomegaly, causes this condition; hence, intracranial pressure appears within normal or levels at high normal. However, slightly elevated ICP may be recorded with continuous ICP monitoring. This often affects subjects older than 65 years and presents with the triad of gait abnormalities, urinary incontinence, and dementia. This triad is from where the mnemonic "wobbly, wet, and wacky" comes.