Introduction
The inguinal ligament is involved in the condition known as the sportsman groin (inguinal disruption). Additionally, this ligament is an important surgical landmark and a groin hernia repair component. About 20 million people have an inguinal hernia repair yearly, making this type of surgery one of the most commonly performed worldwide. The lifetime occurrence of groin hernia, including visceral or adipose tissue protrusions through the inguinal or femoral canal, is 27% to 43% in men and 3% to 6% in women.[1][2] Inguinal hernias are almost always symptomatic, and surgery is the only cure. This topic discusses the anatomy of the inguinal ligament and its clinical importance.
Gabrielle Falloppio first discovered the inguinal or Poupart ligament in 1562. Famous French anatomist Francois Poupart further described this important structure.[3] Cunningham later discussed the inguinal ligament's tendinous nature in detail.
Structure and Function
Inguinal Ligament Location And Structure
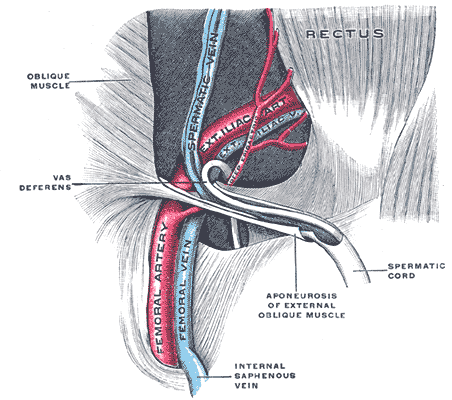
The most superficial anterior abdominal wall muscle is the external oblique, which arises from the posterior aspect of the lower 8 ribs. The muscle fibers run diagonally, starting superolaterally and running inferomedially, forming an aponeurosis. The fibers fan out and inserted, from superior to inferior, into the xiphoid process, linea alba, pubic crest, pubic tubercle, and anterior half of the iliac crest. The obliquely arranged anteroinferior fibers of the aponeurosis fold on themselves inward to form the inguinal ligament, running between the anterior superior iliac spine (ASIS) and pubic tubercle.
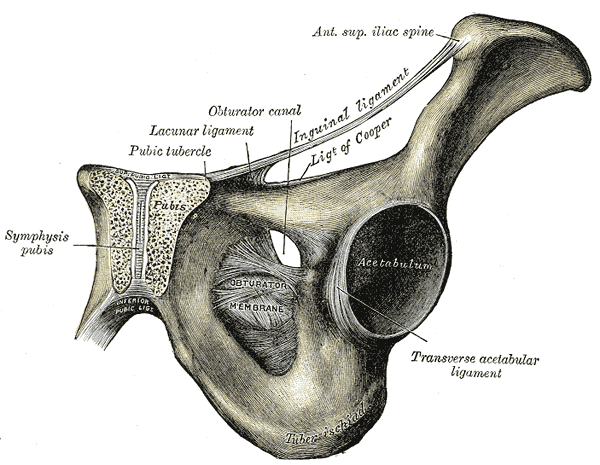
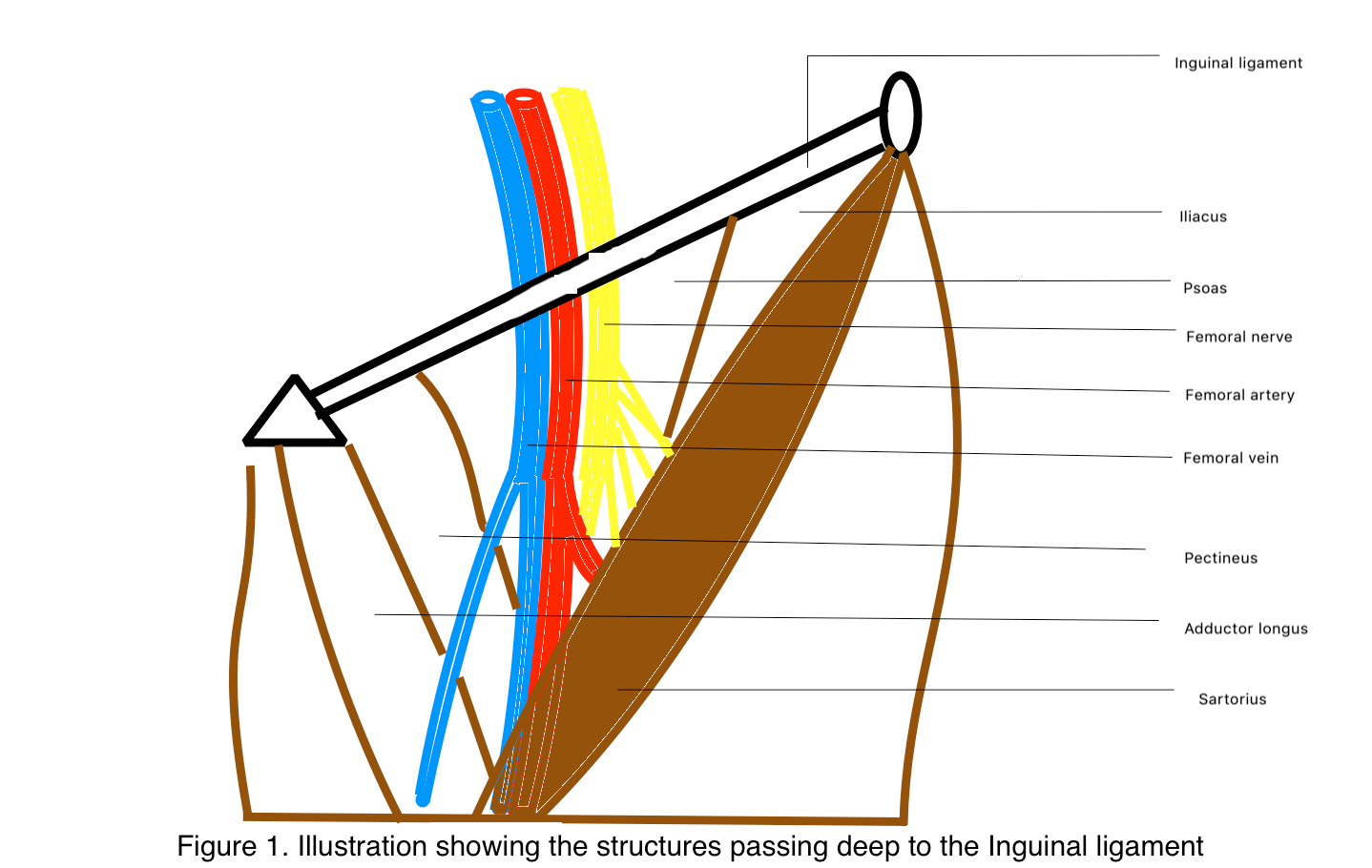
The inguinal ligament is connected inferiorly to the fascia lata of the thigh. Hence, its caudally directed convexity. The ligament bridges the neurovascular and muscular structures passing from the deep pelvis to the thigh.[4] The structures lying deep to the inguinal ligament from lateral to medial are the following (see Image. Femoral Triangle):
- Lateral femoral cutaneous nerve
- Femoral nerve
- External iliac artery and its continuation as the femoral artery
- Femoral vein and its continuation as the external iliac vein
- Femoral ring with deep inguinal lymphatic channels and lymph nodes
- Iliacus, psoas, pectineus, and adductor longus muscles [5]
The mid-inguinal point is an important surgical landmark, as it is the midpoint of the imaginary line joining the ASIS and pubic symphysis. The external iliac artery continues as the femoral artery deep to this point, passing from the pelvic cavity to the lower limb. The femoral artery can only be palpated below the inguinal ligament at the mid-inguinal point.
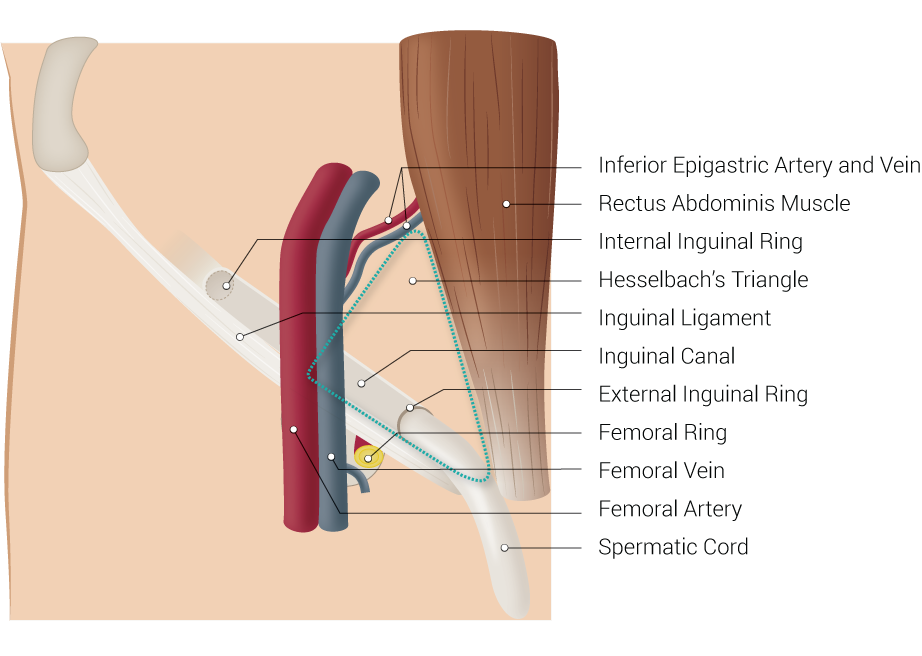
The inguinal ligament midpoint differs from the mid-inguinal point, as it is the midpoint between the ASIS and the pubic tubercle (see Image. Left Inguinal Ligament, Anterior View). The midpoint of the inguinal ligament is just lateral to the mid-inguinal point. The deep inguinal ring lies 0.5 inches above the inguinal ligament midpoint.[6]
The inguinal ligament is rounded and oblique laterally. Medially, this fibrous structure is grooved and becomes more horizontal. The superior surface of the inguinal ligament is grooved and forms the inguinal canal floor. This region contains the ilioinguinal nerve and spermatic cord in male individuals and round ligament in female individuals (see Image. Inguinal Canal).
Inguinal Ligament Attachments
The inguinal ligament attaches inferiorly to the fascia lata (deep thigh fascia). Superiorly, the inguinal ligament gives rise to the internal oblique muscle from its lateral two-thirds, the transversus abdominus muscle from the lateral one-third, and the cremaster muscle from the middle third.
Inguinal Ligament Extensions
The inguinal ligament fans out at the medial end before attaching to the pubic tubercle, forming what is called the "lacunar ligament" or "Gimbernat ligament." The lacunar ligament's apex is at the pubic tubercle, attached anteriorly to the inguinal ligament and posteriorly to the pectinate line (pecten pubis). The lacunar ligament's base lies laterally. The pectinate ligament (ligament of Cooper) extends laterally from the lacunar ligament base, which attaches to the pectineal line.
A few reflected inguinal ligament fibers travel superomedially at an angle of 45°. These fibers travel from the lateral crus of the superficial inguinal ring and decussate with contralateral fibers at the linea alba just anterior to the pyramidal muscle (or rectus sheath in some individuals). Reflected fibers of the inguinal ligament are also called the "Colle ligament," "triangular fascia," or "reflex ligament." About 83% of the cadavers examined in a 2009 study had a reflected inguinal ligament.[7]
Inguinal Ligament: Is It A Ligament Or Tendon?
The debate on whether the inguinal ligament is a tendon or ligament continues, as both structure types have similar connective tissue compositions. Grossly, ligaments and tendons are classified according to their connections—ligaments attach bones to other bones, while tendons join bones to muscles. However, the inguinal ligament does not fall neatly into either category, as it arises from the external oblique aponeurosis and connects the ASIS to the pubic tubercle. Functionally, the inguinal ligament does not stabilize joints, which is an important role of musculoskeletal ligaments. Mature adults have the ileum and pubis—the inguinal ligament's pelvic attachments—fused into a single bone.
Literature states that ligaments stabilize joints and must always be preserved during surgery. Meanwhile, surgeons continue to perform inguinal ligament tenotomy in patients with inguinal disruption. This practice reinforces the anatomical classification of the inguinal ligament.
Embryology
Somitic dermatomyotomes give rise to the musculature in all vertebrates. The ventral body wall myocytes develop from the lateral or hypaxial half of the dermomyotomes, and the spinal nerve ventral branches innervate them. The hypaxial muscles differentiate into 3 separate layers, becoming apparent by the end of the 6th week of embryonic development. Depending on their position in the succeeding stages, the muscle layers correspond to the abdomen's external oblique (outer layer), internal oblique (middle layer), and transverse abdominal (inner layer) muscles.[8]
Blood Supply and Lymphatics
The external iliac artery exits the pelvis immediately deep to the inguinal ligament and continues as the femoral artery. This artery runs through the femoral triangle, a region bounded by the inguinal ligament, sartorius, and adductor longus muscle. The femoral artery travels parallel to the femoral vein and deep inguinal lymphatics inside the femoral canal.[9]
Nerves
The 2 nerves passing immediately deep to the inguinal ligament are the lateral cutaneous femoral nerve of the thigh and the femoral nerve. The lateral cutaneous femoral nerve of the thigh usually arises from the posterior division of the L2 and L3 spinal nerves. The nerve courses from the lumbar spinal roots through the pelvis and toward the ASIS. The nerve leaves the pelvis afterward, traveling beneath the inguinal ligament anterior to the ASIS. The lateral cutaneous femoral nerve of the thigh divides into 2 branches, the anterior and posterior divisions, once leaving the pelvis. These nerves provide sensory innervation to the skin of the anterolateral and lateral aspects of the thigh.[10]
The femoral nerve arises from the posterior divisions of the ventral rami of L2, L3, and L4. This nerve passes through the pelvis deep to the inguinal ligament, lateral to the femoral artery. The femoral nerve enters the lateral side of the femoral triangle and provides motor and sensory innervation to the thigh.
Surgical Considerations
The inguinal and lacunar ligaments form the anterior and medial walls of the femoral ring, respectively. Femoral ring weakness can lead to femoral hernia, forcing abdominal contents through the narrow opening and potentially leading to bowel strangulation.[6] A Laugier hernia is the protrusion of abdominal contents through a weakness in the lacunar ligament.
Diffuse chronic groin pain syndrome is a condition affecting athletes performing high-intensity exercise. "Sportsman groin," "sportsman hernia," and "inguinal disruption" are synonyms for this disorder. Inguinal ligament dehiscence is a possible cause of inguinal disruption. The condition is usually unresponsive to conservative therapy. However, surgical repair of the inguinal ligament may benefit patients.[11]
Clinical Significance
The inguinal ligament is an important diagnostic and surgical landmark. This structure helps differentiate groin hernia types. Herniation above the ligament indicates an inguinal hernia, while protrusion below the ligament signifies a femoral hernia. Inguinal hernias are direct if they arise within the Hesselbach triangle, a region bounded by the lateral border of the rectus sheath medially, inguinal ligament inferiorly, and inferior epigastric artery laterally (see Image. Inguinal Region). An indirect inguinal hernia forms lateral to the triangle and through the deep inguinal ring.