[1]
Ozmen S,Dogru M,Bozkurt C,Kocaoglu AC, Probable cytarabine-induced acral erythema: report of 2 pediatric cases. Journal of pediatric hematology/oncology. 2013 Jan;
[PubMed PMID: 22767133]
Level 3 (low-level) evidence
[2]
Giacchero D,Monpoux F,Chiavérini C,Lacour JP, [6-mercaptopurine-related hand-foot syndrome in a four-year-old child]. Annales de dermatologie et de venereologie. 2008 Aug-Sep;
[PubMed PMID: 18789293]
[3]
Degen A,Alter M,Schenck F,Satzger I,Völker B,Kapp A,Gutzmer R, The hand-foot-syndrome associated with medical tumor therapy - classification and management. Journal der Deutschen Dermatologischen Gesellschaft = Journal of the German Society of Dermatology : JDDG. 2010 Sep;
[PubMed PMID: 20482685]
[4]
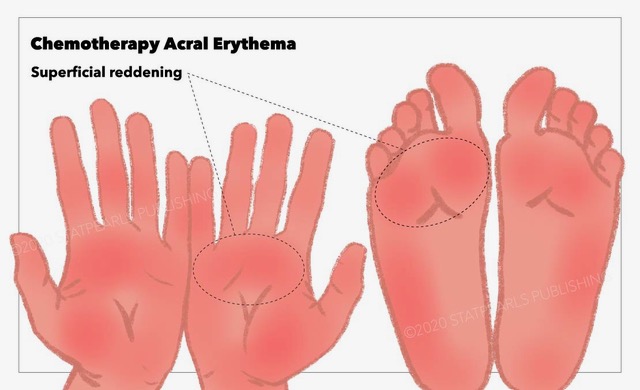
Chidharla A,Kasi A, Cancer, Chemotherapy Acral Erythema (Palmar-Plantar Erythrodysesthesia, Palmoplantar Erythrodysesthesia, Hand-Foot Syndrome) 2018 Jan;
[PubMed PMID: 29083584]
[5]
Hueso L,Sanmartín O,Nagore E,Botella-Estrada R,Requena C,Llombart B,Serra-Guillén C,Alfaro-Rubio A,Guillén C, [Chemotherapy-induced acral erythema: a clinical and histopathologic study of 44 cases]. Actas dermo-sifiliograficas. 2008 May;
[PubMed PMID: 18394404]
Level 3 (low-level) evidence
[6]
Gupta A,Sardana K,Bhardwaj M,Singh A, Methotrexate Cutaneous Toxicity following a Single Dose of 10 mg in a Case of Chronic Plaque Psoriasis: A Possible Idiosyncratic Reaction. Indian dermatology online journal. 2018 Sep-Oct;
[PubMed PMID: 30258802]
Level 3 (low-level) evidence
[7]
Jalandhara P,Kaeley G, Cutaneous toxicity of oral low-dose methotrexate. Proceedings (Baylor University. Medical Center). 2018 Jul;
[PubMed PMID: 29904314]
[9]
Rosmarin D,Palles C,Church D,Domingo E,Jones A,Johnstone E,Wang H,Love S,Julier P,Scudder C,Nicholson G,Gonzalez-Neira A,Martin M,Sargent D,Green E,McLeod H,Zanger UM,Schwab M,Braun M,Seymour M,Thompson L,Lacas B,Boige V,Ribelles N,Afzal S,Enghusen H,Jensen SA,Etienne-Grimaldi MC,Milano G,Wadelius M,Glimelius B,Garmo H,Gusella M,Lecomte T,Laurent-Puig P,Martinez-Balibrea E,Sharma R,Garcia-Foncillas J,Kleibl Z,Morel A,Pignon JP,Midgley R,Kerr D,Tomlinson I, Genetic markers of toxicity from capecitabine and other fluorouracil-based regimens: investigation in the QUASAR2 study, systematic review, and meta-analysis. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2014 Apr 1;
[PubMed PMID: 24590654]
Level 1 (high-level) evidence
[10]
Gambichler T,Strutzmann S,Tannapfel A,Susok L, Paraneoplastic acral vascular syndrome in a patient with metastatic melanoma under immune checkpoint blockade. BMC cancer. 2017 May 12;
[PubMed PMID: 28499411]
[11]
Caccavale S,Ruocco E, Acral manifestations of systemic diseases: Drug-induced and infectious diseases. Clinics in dermatology. 2017 Jan - Feb;
[PubMed PMID: 27938813]
[12]
Levine LE,Medenica MM,Lorincz AL,Soltani K,Raab B,Ma A, Distinctive acral erythema occurring during therapy for severe myelogenous leukemia. Archives of dermatology. 1985 Jan;
[PubMed PMID: 3855356]
[13]
Molpus KL,Anderson LB,Craig CL,Puleo JG, The effect of regional cooling on toxicity associated with intravenous infusion of pegylated liposomal doxorubicin in recurrent ovarian carcinoma. Gynecologic oncology. 2004 May
[PubMed PMID: 15099971]
[14]
Mangili G,Petrone M,Gentile C,De Marzi P,Viganò R,Rabaiotti E, Prevention strategies in palmar-plantar erythrodysesthesia onset: the role of regional cooling. Gynecologic oncology. 2008 Feb
[PubMed PMID: 18083217]
[15]
Wolf SL,Qin R,Menon SP,Rowland KM Jr,Thomas S,Delaune R,Christian D,Pajon ER Jr,Satele DV,Berenberg JL,Loprinzi CL, Placebo-controlled trial to determine the effectiveness of a urea/lactic acid-based topical keratolytic agent for prevention of capecitabine-induced hand-foot syndrome: North Central Cancer Treatment Group Study N05C5. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2010 Dec 10
[PubMed PMID: 21060036]
Level 2 (mid-level) evidence
[16]
Hofheinz RD,Gencer D,Schulz H,Stahl M,Hegewisch-Becker S,Loeffler LM,Kronawitter U,Bolz G,Potenberg J,Tauchert F,Al-Batran SE,Schneeweiss A, Mapisal Versus Urea Cream as Prophylaxis for Capecitabine-Associated Hand-Foot Syndrome: A Randomized Phase III Trial of the AIO Quality of Life Working Group. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2015 Aug 1
[PubMed PMID: 26124485]
Level 2 (mid-level) evidence
[17]
Kang YK,Lee SS,Yoon DH,Lee SY,Chun YJ,Kim MS,Ryu MH,Chang HM,Lee JL,Kim TW, Pyridoxine is not effective to prevent hand-foot syndrome associated with capecitabine therapy: results of a randomized, double-blind, placebo-controlled study. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2010 Aug 20
[PubMed PMID: 20625131]
Level 1 (high-level) evidence
[18]
Chalermchai T,Tantiphlachiva K,Suwanrusme H,Voravud N,Sriuranpong V, Randomized trial of two different doses of pyridoxine in the prevention of capecitabine-associated palmar-plantar erythrodysesthesia. Asia-Pacific journal of clinical oncology. 2010 Sep
[PubMed PMID: 20887495]
Level 1 (high-level) evidence
[19]
Chen M,Zhang L,Wang Q,Shen J, Pyridoxine for prevention of hand-foot syndrome caused by chemotherapy: a systematic review. PloS one. 2013
[PubMed PMID: 23977264]
Level 1 (high-level) evidence
[20]
Macedo LT,Lima JP,dos Santos LV,Sasse AD, Prevention strategies for chemotherapy-induced hand-foot syndrome: a systematic review and meta-analysis of prospective randomised trials. Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2014 Jun
[PubMed PMID: 24463616]
Level 1 (high-level) evidence
[21]
Drake RD,Lin WM,King M,Farrar D,Miller DS,Coleman RL, Oral dexamethasone attenuates Doxil-induced palmar-plantar erythrodysesthesias in patients with recurrent gynecologic malignancies. Gynecologic oncology. 2004 Aug
[PubMed PMID: 15297168]
[22]
Jain L,Sissung TM,Danesi R,Kohn EC,Dahut WL,Kummar S,Venzon D,Liewehr D,English BC,Baum CE,Yarchoan R,Giaccone G,Venitz J,Price DK,Figg WD, Hypertension and hand-foot skin reactions related to VEGFR2 genotype and improved clinical outcome following bevacizumab and sorafenib. Journal of experimental
[PubMed PMID: 20630084]
Level 2 (mid-level) evidence