Introduction
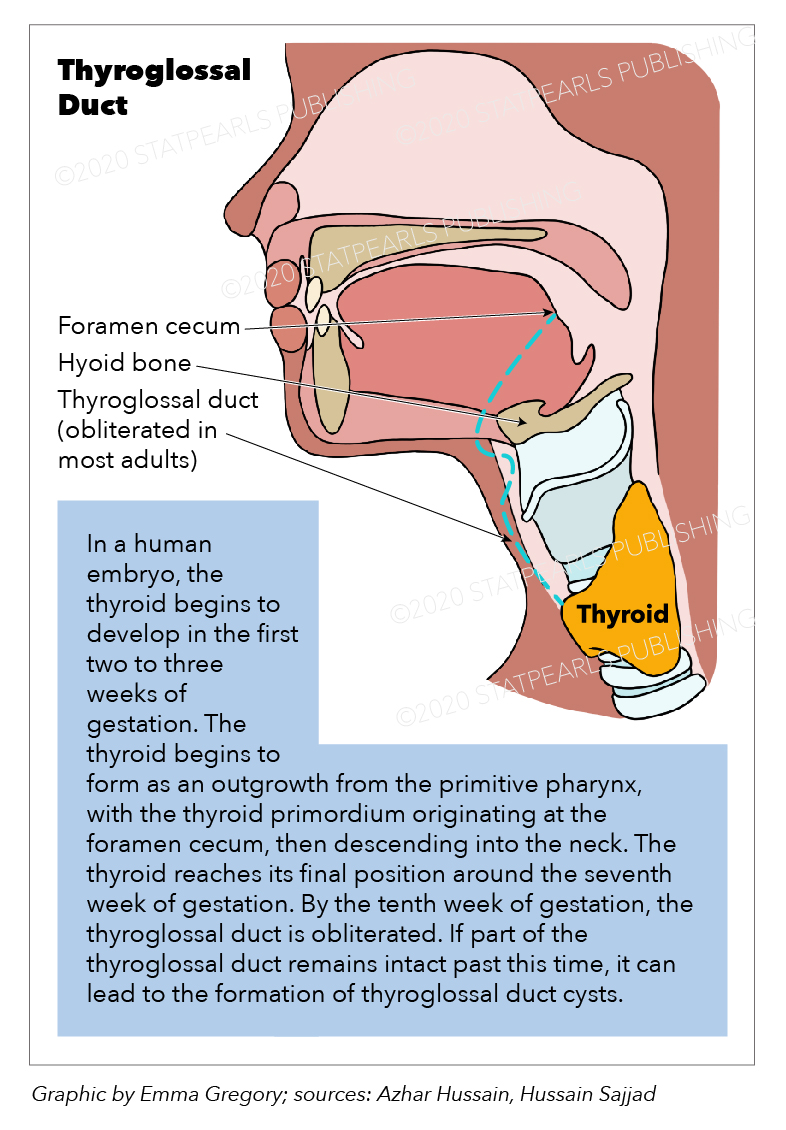
The thyroglossal duct is a connection that serves as a pathway for the primordium thyroid gland in its embryogenesis. This pathway originates at the junction of the anterior two-thirds and the posterior third of the tongue at its base. This pathway commences at the foramen caecum, goes anteriorly, and ends at 2nd and 3rd cartilage of the trachea, where the thyroid ends its trajectory and matures. In its trajectory, the thyroglossal duct passes anteriorly to the forming hyoid bone and thyroid cartilage, until it finally reaches its final position, anterolaterally, at the superior portion of the trachea.[1][2][3]
Structure and Function
The primary function of the duct is to function as the pathway for the trajectory of the primordium thyroid gland, before its descent from the base of the tongue, at the foramen caecum, to the 2nd and 3rd cartilages of the trachea.[2]
Embryology
Thyroid development begins in the 2 to 3 weeks of gestation and starts as a median outgrowth from the primitive pharynx. The thyroid primordium originates at the foramen caecum, which is the junction of the anterior two-thirds and posterior one-third of the tongue.
From this point onwards, the thyroid then descends to the neck, passing anteriorly and closely to the developing hyoid bone and thyroid cartilage, finally reaching its final position in the inferior pre-tracheal neck by the seventh week of gestation. The distal part of the thyroglossal duct differentiates into the pyramidal lobe of the thyroid gland in 50% of the cases, while the thyroid gland is forming itself. The rest of the duct is, supposedly, expected to obliterate by the tenth week of gestation. If any part of the thyroglossal duct persists after the tenth week of gestation, a rise in the probability of pathology occurs. The persistence of any portion of the thyroglossal duct becomes the gateway to the formation of the thyroglossal duct cyst. If given enough development to the pathology, it can even cause thyroglossal duct cyst carcinoma.[2][4]
Surgical Considerations
The development of thyroglossal duct cyst, due to the failed obliteration of the thyroglossal duct before the tenth week of gestation, requires a surgical procedure with removal of the cyst/mass. This surgical procedure necessary for the removal of the cyst/mass is referred to as the Sistrunk procedure and is considered the preferred method of resection of these midline neck cysts and/or masses. Depending on whether the developed mass is benign or malignant, treatment should go accordingly. As previously mentioned, the Sistrunk procedure would be the treatment of choice in cystic masses, which have a recurrence rate of under 3% while applying this procedure.
The procedure consists of a neck incision in which we go up the hyoid bone located in the upper neck. The mid-portion of the hyoid bone is then removed along with a small amount of tongue tissue. This last step, removal of the mid-portion of the hyoid bone along with a slight bit of tongue tissue, is done to prevent the reoccurrence of a cystic mass.
During the development of the embryo, the thyroglossal duct has a tendency to wrap itself inferiorly around the hyoid bone, and on rare occasions, it can entrap itself and be incorporated into the 2nd and 3rd arch components of the hyoid bone, causing the reoccurrence of cystic masses to be possible.
Due to the possibility of reoccurrences, the procedure requires excision of the mid-portion of the hyoid bone and a small amount of tongue tissue. The incision wound is then closed-up with an absorbable suture, and the dermabond is used for skin closure.
In case of a malignant mass, depending on the case and team of surgeons at hand, the procedure will or will not be applied. Radioiodine and levothyroxine therapy is usually the most common treatments in these cases and is also the treatment of choice. Partial resection or complete resection of the thyroid might also be part of the procedure.[4][5][6]
Clinical Significance
The clinical relevance of the thyroglossal duct adheres to its embryologic function. The descent of the thyroid primordium begins at the base of the tongue, specifically at the foramen caecum, until it reaches its final resting place at the level of the 2nd and 3rd cartilage of the trachea, where the thyroid primordium will differentiate itself into the thyroid gland.
Clinically, the failure for the thyroglossal duct to obliterate by the 10th week of gestation is a frequent cause for the apparition of midline neck masses, called thyroglossal duct cyst. Around 7% of the normal population will suffer from this condition. The location of these masses can appear anywhere along the traject of the thyroglossal duct, and can even result from partial obliteration of the duct. This, essentially, means that if at any point in the pathway, the duct did not obliterate itself, a possible cystic mass will appear.
Most cystic masses arise at the infrahyoid level (65% of the cases) and result from the secretion of the epithelial lining that remained from the non-obliterated duct, resulting in possible inflammation and, therefore, the formation of a thyroglossal duct cyst. These are the most common cause of midline neck masses around the world.
Around 70% of the cases in which thyroglossal duct cyst are present are found during childhood, with a prevalence of intracystic thyroid tissue ranging from 5% to 62% of the cases, meaning that the prevalence of thyroglossal duct cyst carcinoma is very low.
Other masses may arise from the persistence of the thyroglossal duct, such as thyroglossal duct cyst carcinomas, which are more prevalent in women within the age range of 20 to 50 years old. The exact etiology behind these carcinomas is not well understood, and even though they are very well associated with various types of thyroid cancer, they account for less than 1% of the cases. The most common form of cancer associated with thyroglossal duct cyst carcinoma is the thyroid papillary carcinoma, which is present in 85% of the cases. Following the papillary thyroid carcinoma, histologically speaking, the most common cancers associated with thyroglossal duct cyst carcinoma are the squamous cell carcinoma, follicular cell carcinoma, anaplastic carcinoma, epidermoid carcinoma, and Hurthle cell carcinoma.
As for the treatment and prognostics of these masses, given that the most common type of thyroglossal duct cyst carcinoma is the papillary thyroid cancer, the prognosis is good. Because the treatment of papillary thyroid cancer has improved over the years, patients tend to respond well to the usual therapy. As for other types of carcinoma, prognosis worsens as cancer becomes more aggressive, and thus, the treatment options become limited due to the poor response to chemotherapeutic and radiotherapeutic agents.[2][7][8][9][10]